Tsai, HL, et al. Rectal carcinoma in a young female patient with Peutz-Jeghers syndrome: a case report. Med Princ Pract. 2014; 23(1):89–91.
Lucci-Cordisco, E, et al. The growing complexity of the intestinal polyposis syndromes. Am J Med Genet A. 2013; 161A(11):2777–2787.
Gammon, A, et al. Hamartomatous polyposis syndromes. Best Pract Res Clin Gastroenterol. 2009; 23(2):219–231.
Hokama, A, et al. Telescope sign of intussusception in Peutz-Jeghers syndrome. Dig Liver Dis. 2009. [Epub ahead of print].
Huang, SC, et al. Pediatric juvenile polyposis syndromes: an update. Curr Gastroenterol Rep. 2009; 11(3):211–219.
Itaba, S, et al. Education and imaging. Gastrointestinal: Solitary Peutz-Jeghers-type hamartoma of the colon. J Gastroenterol Hepatol. 2009; 24(3):498.
Joshi, V. Peutz-Jeghers Syndrome: A Rare Cause of Gastric Outlet Obstruction. Clin Gastroenterol Hepatol. 2009. [Epub ahead of print].
Yano, T, et al. Vascular, polypoid, and other lesions of the small bowel. Best Pract Res Clin Gastroenterol. 2009; 23(1):61–74.
Cho, GJ, et al. Peutz-Jeghers syndrome and the hamartomatous polyposis syndromes: radiologic-pathologic correlation. Radiographics. 1997; 17(3):785–791.
Harned, RK, et al. The hamartomatous polyposis syndromes: clinical and radiologic features. AJR Am J Roentgenol. 1995; 164(3):565–571.
Buck, JL, et al. Peutz-Jeghers syndrome. Radiographics. 1992; 12(2):365–378.
 , presumably hamartomas, throughout his bowel.
, presumably hamartomas, throughout his bowel.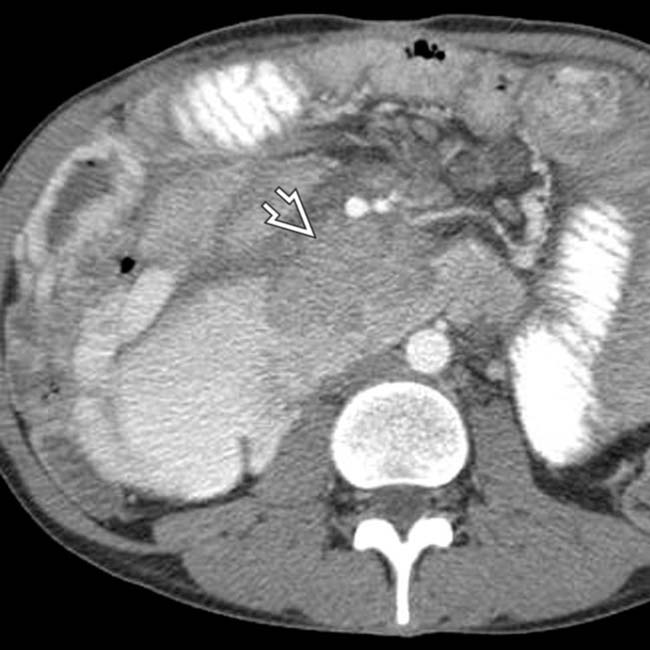
 causing partial obstruction of the duodenum. The mass proved to be a metastasis from a testicular nonseminomatous germ cell tumor.
causing partial obstruction of the duodenum. The mass proved to be a metastasis from a testicular nonseminomatous germ cell tumor.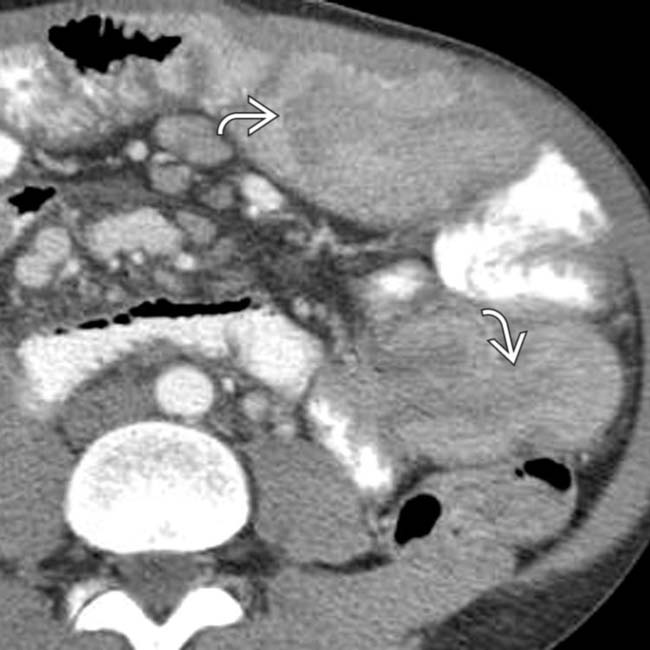
 , probably due to the hamartomatous polyps.
, probably due to the hamartomatous polyps.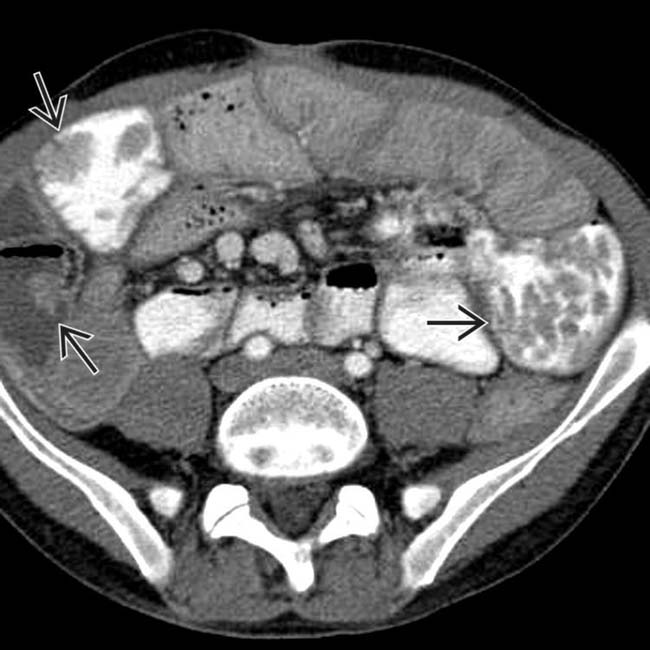
 . As illustrated by this case, some patients with PJS may develop malignant tumors, not just of the bowel, but also of the breast, pancreas, or reproductive tract.
. As illustrated by this case, some patients with PJS may develop malignant tumors, not just of the bowel, but also of the breast, pancreas, or reproductive tract.







































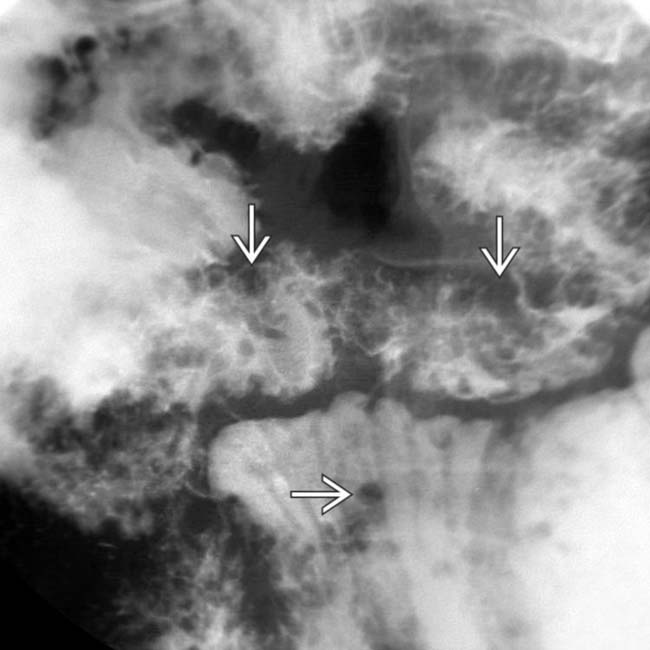
 proven at surgery to be due to hamartomatous polyps.
proven at surgery to be due to hamartomatous polyps.
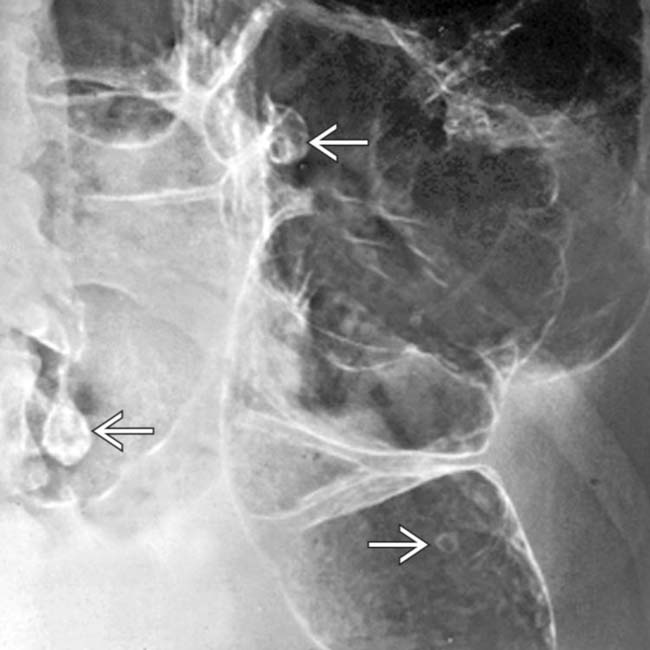
 in a patient with Peutz-Jeghers syndrome.
in a patient with Peutz-Jeghers syndrome.


