Hallucinogens
Serotonin-Like Agents
Perspective: Background and Epidemiology
Serotonin-like agents are a broad category of compounds that share chemical similarities with serotonin (5-hydroxytryptamine [5-HT]) or enhance serotonergic tone within the body. These agents include various lysergic acid derivatives and tryptamines. Serotonin-like agents produce changes in thought, mood, perception, and consciousness. Orientation to person, place, and time is usually preserved, but severe intoxication may cause confusion. Patients present to the emergency department because of acute panic reactions, massive ingestions, or accidental ingestions (e.g., children or adults who have ingested the drugs unknowingly). There is no addictive component in psychedelics and no euphoria-dysphoria cycle, as with cocaine. The rapid development of tolerance also limits the effect of repeated doses.1
LSD
Lysergic acid diethylamide (LSD), or acid, is the most potent psychoactive drug. Doses of 1 to 1.5 µg/kg produce psychedelic effects. The typical dose taken for an acid “trip” is approximately 25 to 100 µg. LSD is sold in tablets (microdots), liquid, powder, gelatin squares (window panes), and “blotter” acid. Sheets of blotting paper are sprayed with LSD, dried, and perforated into small squares. Graphics are incorporated onto the blotting paper in designs that include cartoon characters (e.g., Felix the Cat) and geometric designs (Fig. 156-1). Each sheet is composed of hundreds of squares that are placed sublingually or eaten whole. Massive ingestions are rare.
In addition to synthetic LSD, several plants contain alkaloids similar in structure and action to LSD. These plants include Hawaiian baby woodrose (Argyreia nervosa), Hawaiian woodrose (Merremia tuberosa), morning glory (Ipomoea violacea), and oliliuqui (Rivea corymbosa). Intoxication may result after ingestion of the seeds or an extract.2
Tryptamines
Psilocybin and psilocin are naturally occurring tryptamines found in some species of Psilocybe (Fig. 156-2), Panaeolus, and Conocybe mushrooms.3 Psilocybin remains active even when the mushrooms are dried or cooked. Street psilocybin sold as pills or capsules is usually substituted with phencyclidine (PCP) or LSD. Misidentification of other poisonous species is a danger of consuming mushrooms.

Figure 156-2 Psilocybe cubensis mushroom. (Copyright © 2003 Erowid.org. Accessed at www.erowid.org.)
Naturally occurring tryptamines are found not only in plants and fungi but also in the parotid glands of the Bufo toad species. The venom of the Sonoran Desert or Colorado River toad (Bufo alvarius) contains the hallucinogenic substance 5-MeO-DMT, found in the drink ayahuasca. Smoking of the dried venom results in psychoactive effects similar to those of 5-MeO-DMT.4
In addition to the tryptamines that occur in nature, designer tryptamines have been synthesized and are orally active.5 Included in this group are α-methyltryptamine, diisopropyltryptamine, and diisopropyl-5-methoxytryptamine, which is also known on the streets as “foxy” or “foxy methoxy”.6 The effects of these synthetic derivatives are similar to those of naturally occurring tryptamines.
Principles of Disease: Pharmacology and Pathophysiology
Evidence indicates that these drugs act on serotonergic neurons, particularly the 5-HT2A subtype class of serotonin receptors.1,7 The onset of action of the psychoactive effects of LSD is usually within 30 minutes, with peak effects in 3 or 4 hours. The duration of effects may be approximately 12 hours. During the last half of the 12-hour effect, irritability, increased muscle tension (especially in the face), and paranoia can be present. Psilocybin effects begin within 30 minutes of ingestion, with the psychedelic phase lasting 30 minutes to 2 hours. The effects then wane, with resolution by 4 to 6 hours.
Clinical Features
Massive ingestions may result in a person’s becoming comatose and unresponsive to pain. The person may also be hyperactive with marked auditory and visual hallucinations. Fixed and dilated pupils, diaphoresis, vomiting, bleeding complications, and seizures may result.8
Entactogens
Perspective: Background and Epidemiology
Designer Amphetamines and Cathinones (Bath Salts)
New designer amphetamines appear in drug communities each year. This class of chemicals usually has a structural base of a phenylalkylamine with addition or substitution of side chains or rings. Agents include 3,4-methylenedioxymethamphetamine (MDMA, ecstasy, XTC, or Adam), 3,4-methylenedioxyamphetamine (MDA), 3,4-methylenedioxyethamphetamine (Eve), paramethoxyamphetamine (PMA or death), 4-methyl-2,5-dimethoxyamphetamine (serenity, tranquility, and peace [STP]), 2,5-dimethoxy-4-iodoamphetamine (DOI), 2,5-dimethoxy-4-bromoamphetamine (DOB), and others.9
Entactogens are predominantly used in three main settings: (1) as “psychotherapeutic adjuncts,” (2) recreationally in small groups or by couples, and (3) at dance clubs or “rave” parties. Herbal ecstasy, known as ma huang or ephedra, is sometimes substituted for MDMA at these gatherings when MDMA is scarce. Although this herb contains ephedrine, its effects are not as psychedelic as those of MDMA. Ecstasy tablets may also contain other chemicals, such as amphetamine, methamphetamine, caffeine, and ketamine. MDMA is widely available and is sold in clubs, on the street, and at raves (usually 30-150 mg/pill), with a typical dose of 1 or 2 mg/kg.10 The continuous muscle activity required during these parties in combination with the psychostimulants may produce rhabdomyolysis and hyperthermia. Nine deaths in Canada associated with paramethoxyamphetamine (PMA) were originally reported in 1974, but clusters of multiple deaths in association with PMA exposure have occurred in Europe and Australia.11,12 Signs and symptoms of adrenergic excess occur before death, but whether PMA is more toxic in equipotent dosages than other amphetamines is not known.
Designer cathinones may be advertised and distributed as “bath salts” or “plant food” in packaging that suggests the actual intent of the product even though it might be labeled “not for human consumption.” These synthetic cathinones sold unregulated over the Internet initially contained mephedrone, but their content rapidly changed to include methylone, ethylone, butylone, pyrovalerone, methylenedioxypyrovalerone (MDPV), methcathinone, ethcathinone, and numerous others. These products may be ingested, inhaled, or injected and result in severe agitation, sympathomimetic effects, or even death.13 Detection of these cathinones is more difficult as their structures are dissimilar enough to classic amphetamines and methamphetamines that routine urine drug testing is not able to detect them.
Mescaline
Mescaline is usually consumed in the form of peyote buttons, which are derived from the small blue-green cacti Lophophora williamsii and Lophophora diffusa (Fig. 156-3). The cacti grow in the deserts of the southwestern United States and Mexico. Peyote buttons are the round fleshy tops, which are removed and dried. Mescaline is the active hallucinogenic alkaloid found in the buttons of the cactus.

Figure 156-3 Lophophora williamsii (peyote cactus). (Photo by Christopher B. Copyright © 2000 Erowid.org. Accessed at www.erowid.org.)
Peyote has been used in religious ceremonies for 8000 years. Mescaline is also contained in the San Pedro cactus (Trichocereus pachanoi) of South America and is used ritualistically by Andean Native Americans.1 These cacti contain many other alkaloids, some of which are also psychoactive. The use of peyote is legal for members of the Native American Church in some states. Adverse reactions (e.g., panic) to peyote are rare in this structured religious use. Mescaline has an onset of action of 45 to 60 minutes with a duration of 4 to 8 hours. The central nervous system (CNS) and physiologic effects of mescaline use are similar to those of LSD, but more vivid hallucinations can occur. Nausea and vomiting are pronounced and almost always precede the hallucinogenic effects.
Piperazines
N-Substituted piperazine compounds such as 1-benzylpiperazine (BZP or A2), 1-(trifluoromethylphenyl)piperazine (TFMPP or Molly), and 1-(chlorophenyl)piperazine (CPP) have emerged as drugs of abuse and have been sold as safe, legal alternatives to MDMA; they are referred to as Legal E or Legal X on Internet websites.14,15 Although BZP was originally synthesized as a potential anthelmintic agent, there are currently no therapeutic applications for BZP or its congeners. Both in vitro and animal studies demonstrated that these piperazine compounds stimulate release of serotonin and other monoamines but are less potent in comparison to MDMA.15 In 2002, both BZP and TFMPP were classified as Schedule I drugs because of their potential for abuse and hazard to the public. There are no deaths directly attributed to these piperazines, but fatalities occur in association with their use.14
Nutmeg
Nutmeg is a spice derived from the seed of the nutmeg tree, Myristica fragrans. Use of nutmeg as a natural and legal psychotropic agent was popularized in the 1960s. Despite lack of any in vivo human studies, myristicin and elemicin have been suggested as the agents responsible for intoxication because their chemical structures resemble that of mescaline. Reports of intoxication are uncommon.16,17 Ingestion of 5 to 30 g (1-4 tablespoons) of the spice is said to induce euphoria and hallucinations but is more likely to cause gastroenteritis.
Principles of Disease: Pathophysiology
The psychoactive effects of MDMA and other entactogens are thought to result from alterations in catecholamine neurotransmission at postsynaptic and presynaptic sites, particularly affecting 5-HT. These agents cause a release of serotonin, dopamine, and norepinephrine from nerve terminals as well as inhibit catecholamine reuptake. Release of epinephrine and norepinephrine may produce the cardiovascular effects. MDMA and possibly other entactogens are serotonergic neurotoxins.18,19 When MDMA is administered to nonhuman primates and laboratory animals, serotonin is released initially from serotonergic neurons followed by degradation of 5-HT projections. Magnetic resonance imaging shows significant neurodegeneration.19 These effects may persist for weeks or longer after a single dose.20 The significance of this neurotoxic effect for humans at the doses taken is unknown.21
Psychostimulant-associated hyperthermia is well described in humans. Animal models exposed to entactogens develop hyperthermia in the absence of physical exertion but are less capable of regulating core body temperature in response to environmental hyperthermia.22 In addition, increasing body temperature in the presence of MDMA or other entactogens seems to enhance serotonergic neurotoxicity.23
Hyponatremia resulting in seizures, stupor, and death is another complication of MDMA use not described as commonly with other amphetamines. Two hypotheses suggested for the hyponatremia are (1) excessive intake of free water because users of MDMA are advised to keep well hydrated by drinking lots of water and (2) MDMA-mediated release of antidiuretic hormone.24–26
Clinical Features
Clinical effects expected from the entactogens would be similar to clinical effects of other amphetamine derivatives (see Chapter 154). Use of recreational doses of MDMA at rave parties may result in seizures, hyperthermia, and death. MDMA may precipitate a hypertensive crisis in patients taking monoamine oxidase inhibitors, and it may precipitate serotonin syndrome in combination with other serotonergic agents10 (see Chapter 151). MDMA and its analogues also have contributed to fatal overdoses.27
Diagnostic Strategies
Urine screening with immunoassay techniques can detect entactogens that are similar in structure to the phenylalkylamine structure of amphetamines. Small doses may not be detected, but larger doses may test positive for amphetamine and methamphetamine. As the structure of the designer amphetamine becomes less similar to phenylalkylamine, detection of the drug is less likely. Designer amphetamines, including MDMA, and their metabolites may be detectable with thin-layer chromatography methods.28
Management
Because hyperthermia is a common complication, a core temperature should be obtained. If the patient’s temperature is higher than 40 to 42° C, multiple organ damage often ensues. Active evaporative cooling measures should be instituted to reduce the core temperature because the clinical outcome strongly correlates with the magnitude and duration of the hyperthermia (see Chapter 141). Treatment of hyponatremia should proceed in the usual manner. Antiemetic medications, such as intravenous ondansetron, 4 to 8 mg, may be necessary if nausea and vomiting persist, as typically occurs with peyote and nutmeg ingestions.
Dissociative Agents
Perspective: Background and Epidemiology
Dextromethorphan
Dextromethorphan is not truly a dissociative agent but does share a similarity in structure to PCP and its binding to the PCP site of the N-methyl-D-aspartate (NMDA) receptor. With the availability of concentrated pill formulations, abusers of dextromethorphan are able to ingest large doses without having to drink large volumes of the less palatable cough syrup formulation. Particularly popular in the adolescent community, dextromethorphan is known as “DXM,” “robo,” “skittles,” triple C,” and “red hots.”29
Principles of Disease: Pharmacology and Pathophysiology
Despite being simple molecules, PCP and ketamine have a complex pharmacology, including the NMDA receptor, dopamine-norepinephrine-serotonin reuptake pump, sigma opioid receptor, and cholinergic receptors.30 PCP is well absorbed from any oral, nasal, or rectal mucous membrane and can be insufflated or smoked. It can be injected intramuscularly, subcutaneously, or intravenously. Ingested PCP is well absorbed with onset between 15 and 60 minutes. When it is smoked, PCP produces symptoms within 5 minutes, with peak activity in 15 minutes.31 Intoxication with PCP usually lasts 8 to 16 hours, but it can be prolonged in chronic users. Although enterohepatic recirculation has been proposed, a more likely cause is either gastrointestinal concretion or delayed release from lipid stores.32
Ketamine is only approximately one tenth as potent as PCP.30 With ketamine, the intensity of intoxication is less pronounced, although in larger doses the effects may parallel those of PCP. Duration of action of ketamine is typically shorter, with symptoms lasting approximately 1 hour after insufflation but up to 4 to 8 hours after an oral dose. PCP and ketamine are highly lipid-soluble agents that undergo extensive metabolism in the liver and are eventually excreted in the urine.
Although dextromethorphan is typically classified as an opioid, it has a complex pharmacology. Dextromethorphan is the dextrorotatory isomer of the synthetic opioid levorphanol. At high dosages, dextromethorphan is an agonist at the sigma opiate receptor, and naloxone has been reported to reverse intoxication.33 Dextromethorphan antagonizes the NMDA receptor, which results in its dissociative effects. It also inhibits the uptake of serotonin, and drug interactions with selective serotonin reuptake inhibitors and monoamine oxidase inhibitors are reported.29
Clinical Features
Patients with PCP intoxication have a wide spectrum of findings, with autonomic signs and symptoms similar to those with other sympathomimetic agents. Behavior may be bizarre, lethargic, agitated, confused, or violent. A blank or catatonic stare is common. Vertical, horizontal, and rotatory nystagmus is often present. Moderate hypertension and tachycardia may be present. Pupils usually are midsized and reactive, although there may be miosis or mydriasis. Bizarre posturing, grimacing, and writhing may be seen.34
Other variable findings include ataxia, muscle rigidity, increased deep tendon reflexes, increased secretions, bronchospasm, hyperthermia, and seizures. The percentage of violent patients ranges from 10 to 40% for PCP, and control of these patients may be the most challenging problem in the emergency department. “Superhuman” strength is possible because of the dissociative action of PCP. Although mild hypertension in PCP intoxication is common, hypertension requiring antihypertensive treatment is rare. Severe hypertension with PCP overdose has caused intracerebral hemorrhage but less often than with cocaine or amphetamine.35
Hyperthermia can range from mild to life-threatening. Core temperatures of PCP victims can exceed 40° C and often go undetected for prolonged periods in the emergency department. Severe hyperthermia with temperatures above 42° C resembles heatstroke and is often associated with multiple organ damage.36 High-output congestive heart failure has been reported. Rhabdomyolysis and acute myoglobinuric renal failure are the most common serious medical complications. The presumed mechanism is muscle damage from seizures, extreme muscle activity such as struggling against restraints, or prolonged immobility. Renal function returns after several weeks in most cases. Among the most lethal complications of PCP are respiratory depression, apnea, and cardiac arrest.34
Although dextromethorphan has activity at opioid receptors, the typical triad of opioid intoxication (miosis, respiratory depression, and mental status depression) is not generally encountered.37 Similar to meperidine, dextromethorphan may result in mydriasis through paralysis of the ciliary body with intoxication.38 More typical clinical findings are lethargy, agitation, slurred speech, ataxia, diaphoresis, hypertension, and nystagmus. With larger doses, nausea and vomiting are common, and intoxication resembles that of LSD with euphoria and hallucinations.
Diagnostic Strategies
Most hospital laboratories use radioimmunoassays that can detect urinary PCP with a detection limit of 5 ng/mL. Urine may be positive for PCP for 2 to 4 days after use, but it can be positive for more than 1 week after chronic exposure. Serum screening for PCP is of little clinical benefit because levels correlate poorly with symptoms. Several substances, including dextromethorphan, may cross-react with urine screens for PCP because of their structural similarities. Chlorpromazine, methadone, mesoridazine, ketamine, diphenhydramine, venlafaxine, meperidine, and tramadol may also cross-react with some assays.39 Because dextromethorphan is typically formulated as a hydrobromide salt, chronic use may result in spurious hyperchloremia with a low or negative anion gap due to interference of chloride analysis by the bromide ion in the laboratory autoanalyzer.40
Management
Emergency Department
Patients with PCP toxicity can have unpredictable, violent behavior. Sudden complications, such as cardiac arrest and seizures, may occur but are not common. Violent behavior, although possible, is less common with ketamine. Most patients with minor intoxication are alert, oriented, and neurologically normal after 4 to 6 hours.35 All patients with signs of trauma or struggle should be evaluated for injuries. Reliable assessments of these individuals are difficult, and sedation and restraint are often necessary before diagnostic tests or examinations can be performed.
Comatose patients or patients with a questionable airway should be intubated to ensure adequate ventilation. Although PCP intoxication can cause mild hypotension, profound hypotension is unusual and represents blood loss from trauma, a mixed-drug ingestion, or another underlying medical problem, and the patient should be resuscitated with fluids as evaluation ensues. Seizures should be treated with intravenous benzodiazepines (see Chapter 102). Tachycardia does not require additional treatment except for sedation.
Hyperthermia (temperature of 40° C) is common in severe cases of PCP poisoning. All patients with significant symptoms, psychosis, or history of violent behavior should have core temperatures measured. Individuals with hyperthermia should be treated with active, evaporative cooling measures (see Chapter 141).
Marijuana and Miscellaneous Plants and Fungi
Marijuana and Synthetic Cannabinoids
Principles of Disease: Pharmacology and Pathophysiology
Δ9-Tetrahydrocannabinol (THC) is the main active agent of the more than 61 cannabinol compounds and approximately 300 other substances present in the cannabis plant. Marijuana smoke also contains carbon monoxide, cyanide, acetone, and phenol but not nicotine.41 The most efficient route of THC delivery is by inhalation. Fifty percent of smoked THC is absorbed compared with 6% by ingestion. Experienced users may be able to absorb larger doses with breath-holding techniques. Peak blood levels occur within 8 minutes of inhalation, with rapid distribution into tissues, especially tissues with high lipid content.42 The duration of perceived effects is usually 2 to 4 hours when it is smoked and 6 to 12 hours when it is ingested.
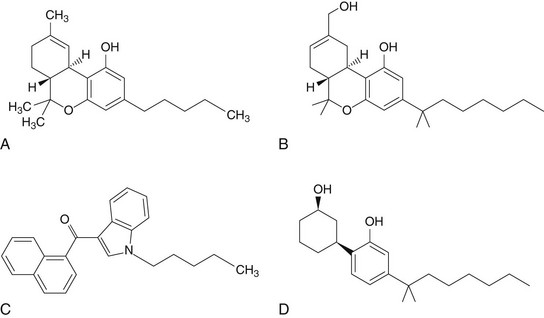
Since the turn of the 21st century, various products containing synthetic “designer” cannabinoids have been gradually emerging and are collectively known as spice. These products are marketed as novelty herbal incense and labeled “not for human consumption.” They typically come in 1- to 3-g resealable foil packages and contain various plant leaves sprayed with a solvent mixture of one to several synthetic cannabinoid compounds. Examples of products include Spice (Diamond, Gold, Silver), K2 Summit, Banana Cream Nuke, Yucatan Fire, Genie, and many others. Because these products are also marketed with an emphasis on being “legal highs,” the DEA issued an order in March 2011 to list five synthetic cannabinoids (JWH-018, JWH-073, JWH-200, CP-47,497, and cannabicyclohexanol) into Schedule I of the Controlled Substances Act (CSA) to avoid an imminent hazard to the public safety.43 Previously, only one synthetic cannabinoid (HU-210), a structural analogue of THC, was listed as such. Because numerous synthetic cannabinoids are available, producers of spice products can simply replace a scheduled cannabinoid with others that remain “legal,” which minimizes the impact of scheduling by the DEA on long-term availability because the demand for the spice products remains high.
Until the first cannabinoid receptor (CB1R) was isolated and cloned in the late 1980s, the effects of cannabis were not thought to be receptor mediated. Subsequently, a second cannabinoid receptor (CB2R) was identified in the early 1990s. Interestingly, CB2Rs are primarily expressed in immune cells peripherally, whereas CB1Rs are found mostly in the CNS in densities similar to γ-aminobutyric acid (GABA) receptors. Because very few CB1Rs are located in the brain stem, which governs basic physiologic functions, the toxicity of THC and synthetic cannabinoids seems to be relatively low with typical recreational use. Discovery of these cannabinoid receptors has renewed interest in further exploration of the therapeutic potential of cannabinoids44 (Fig. 156-4).
Clinical Features: Acute Signs and Symptoms
Smoking of marijuana leads to rapid and predictable signs and symptoms. Ingestion can cause delayed and sometimes unpredictable effects. The most common effects from smoking of marijuana include alteration of mood and usually relaxation and euphoria. The only reliable physiologic effects are a mild increase in heart rate and conjunctival injection. Pupillary changes usually do not occur. Other acute peripheral changes include urinary retention, decreased testosterone levels, and decreased intraocular pressure.45 Short-term memory is impaired, and the ability to perform complex tasks may be adversely affected. Many users report excessive appetite after marijuana use.
Even when “high-potency” marijuana is smoked continuously for hours, adverse effects are rarely seen. Users become more sedated as they continue to smoke but do not become unarousable. No deaths have been solely attributed to marijuana. Pediatric exposures to marijuana may lead to hypothermia, ataxia, nystagmus, tremor, tachycardia, injected conjunctiva, and labile affect.46,47 Oral ingestion of potent marijuana in children can produce rapid onset of drowsiness, hypotonia, and lethargy, which can lead to coma and airway obstruction.46,48
Whereas intoxications with marijuana and spice compounds may be similar in some respects, significant differences have been described.49 The most common adverse reactions include anxiety, panic, paranoia, and acute psychosis, particularly with novice users or individuals with preexisting psychiatric disease. These episodes are unusual and transient with marijuana but may be more common and pronounced with the synthetic cannabinoids. Nausea and vomiting, which are not typical with marijuana, have been reported with a synthetic JWH-018–containing product.
Diagnostic Strategies
Marijuana screening is not helpful in the emergency department. Urinary metabolites of THC are detectable within 1 hour after smoking of marijuana, but a positive urine test result does not correlate with acute intoxication. A single marijuana cigarette can be detected for 72 hours when a cutoff level of 100 ng/mL is used, and positive urine levels may persist for 3 months after chronic marijuana use.50 Inadvertent or passive exposure to marijuana may produce positive urine test results, depending on cutoff levels used.51 False-positive urine screen results may be produced by efavirenz, ibuprofen, and naproxen.52
Differential Considerations
The presentation that most closely resembles marijuana and spice intoxication is acute psychosis. Some individuals with underlying and preexisting psychiatric disorders may progress to overt psychosis after heavy or first-time marijuana use. Because marijuana is so readily available, it is commonly a cointoxicant used with ethanol and other psychotropic agents. Rarely, marijuana can be adulterated with other substances, such as lead.53
Salvia
Salvia divinorum, a perennial herb cultivated well outdoors in mild climates, is a member of the mint (Lamiaceae) family.54 Common names for S. divinorum are diviner’s sage, mystic sage, magic mint, sage of the seers, Sally-D, and ska Maria Pastora. Although the plant has been used for divination and shamanism by the Mazatec Indians of Oaxaca, Mexico, S. divinorum has become popular in the past decade for recreational purposes because of its recognized hallucinogenic properties; it continues to be sold legally by online vendors and “smoke” or “head” shops. In 2004, the DEA listed S. divinorum as a “drug of concern,” but to date, it remains unscheduled under the CSA. Several states, however, have instituted or are considering legislation making possession, cultivation, and use of S. divinorum or its extracts illegal. Internationally, regulatory controls have been implemented in Australia and a number of European countries; however, S. divinorum and salvinorin A are not currently controlled under the CSA in the United States.55 Although many states have decided to independently enact legislation with varying degrees of restriction, Salvia remains readily available.
The active ingredient in S. divinorum is salvinorin A (also known as divinorin A), a neoclerodane diterpene with selective agonist activity for kappa opioid receptors, but it does not bind to delta or mu opioid receptors. Salvinorin A is the first naturally occurring non-nitrogenous kappa opioid receptor agonist with psychotropic properties and is the most potent plant hallucinogen discovered to date. The threshold dose of salvinorin A to produce hallucinations is comparable to that of synthetic LSD and 4-bromo-2,5-dimethoxyphenylisopropylamine. Stimulation of kappa opioid receptors in the brain and spinal cord produces psychomimetic and analgesic effects, respectively. However, salvinorin A is distinct from more traditional hallucinogens because it does not bind to the 5-HT2A serotonin receptors, as is the case with LSD.56
Salvinorin A is not detected and is not known to cause interference with routine drug screens used in the clinical setting. Management of intoxication from S. divinorum is mainly supportive with emphasis on injury prevention. Use of naloxone, a nonspecific opioid-receptor antagonist, may theoretically be helpful in reversal of psychotropic manifestations.57
Kratom
Mitragyna speciosa Korth., or kratom, is a tree indigenous to Thailand but is also found in tropical and subtropical regions of Asia and Africa. Its extracts have been used in Thailand and Malaysia for their euphoric effect as a substitute for opium or to moderate opium use by addicts.58 The popularity of kratom has grown because of reports of its successful use to attenuate symptoms of opioid withdrawal. Because kratom remains easily obtainable from Internet sources, individuals are able to self-administer the perceived remedy, obviating the need for physician supervision.59 The safety of such practice is unknown.
Although kratom extract contains more than 25 alkaloids, mitragynine is the most abundantly found in the plant. Mitragynine is an indole alkaloid with structural analogy to yohimbine and has agonist activity at mu and delta opioid receptors, producing euphoric, analgesic, and respiratory depressant effects. Despite its structural similarity to yohimbine, a selective antagonist of presynaptic alpha2-adrenergic receptors, animal studies suggest that mitragynine is also an agonist at postsynaptic alpha2-adrenergic receptors and blocks 5-HT2A receptors.57
Typically, kratom leaves are chewed, smoked, or brewed into a tea. Psychotomimetic effects occur within 5 to 10 minutes of use and may persist for 1 hour, with stimulatory effects at lower doses and opioid effects at higher doses. Opioid properties include analgesic, antitussive, antidiarrheal, and emetogenic effects. Reports in the medical literature include intrahepatic cholestasis after abuse for 2 weeks.60,61
Currently, there are no diagnostic tests available to detect the presence of kratom alkaloids. Treatment of intoxication is supportive. Although opioid activity has been demonstrated with kratom, the effectiveness of opioid antagonists in reversing effects is inconsistent. A withdrawal syndrome characterized by anxiety, restlessness, and nausea treated with an opioid agonist and lofexidine (an alpha2-agonist related to clonidine) has also been reported.62
Iboga
Although iboga in Western culture is used to ease opioid withdrawal and to diminish craving of other abused drugs, the potential for abuse is high because the hallucinogenic effect is extremely vivid. The intensity of visual hallucinations from ingestion of iboga, in contrast to other hallucinogens, is described to be pronounced with closed eyes.63 There are no clinical tests, and diagnosis is dependent on a history of exposure because clinical findings are largely nonspecific and management is principally supportive. Since the first report in 1990, there have been 11 reported fatalities within 72 hours of ibogaine use with a hypothesized cardiac etiology.63
Absinthe
In addition to ethanol, the active ingredient of absinthe is thought to be thujone, an aromatic terpenoid related to camphor and turpentine. Although the mechanism is not clear, thujone is thought to antagonize the inhibitory GABAA receptor, which may explain the clinical effects observed with absinthe.64 The acute clinical effects of absinthe are reported to be beyond those of ethanol alone and include confusion, delirium, euphoria, and hallucinations (auditory and visual). However, some doubt the plausibility of consuming a dose of thujone adequate to achieve the aforementioned neurotoxic effects given the low concentrations of the toxin present in spirits.65 Nonetheless, thujone is a known proconvulsant in animals and may cause generalized clonic followed by tonic seizure activity. Ingestion of an essential oil of wormwood has been reported to cause seizures complicated with renal failure secondary to rhabdomyolysis.66 Treatment is supportive.
Isoxazole Mushrooms
Isoxazole-containing mushrooms include Amanita muscaria, Amanita pantherina, Amanita gemmata, and Amanita cothurnata. A. muscaria has a red or yellow cap with white warty structures on its surface and grows in forests of aspen, birch, fir, or pine trees (Fig. 156-5). It has been used by Siberians for centuries and is often described in folklore and fairy tales. Pharmacolinguistic evidence indicates that several modern religions began as A. muscaria cults.

Figure 156-5 Amanita muscaria mushroom. (Photo by Mark Shubert. Copyright © 2004 Erowid.org. Accessed at www.erowid.org.)
The active ingredients are the isoxazole derivatives ibotenic acid and its decarboxylation product, muscimol, which are structural analogues of the endogenous neurotransmitters glutamic acid (excitatory) and GABA (inhibitory) and thought to act at these respective receptor sites.67 The excitatory effects characterized by elation, giddiness, hyperactivity, muscle tremors, and distortion of space-time begin approximately 30 minutes to 2 hours after ingestion and are likely to be mediated by ibotenic acid. Following is a phase of tiredness and deep “sleep,” in which it may be difficult to arouse the patient. During this phase, vivid hallucinations and manic excitement may oscillate with periods of deep sleep. The duration of effect is up to 12 hours. Management of the excitatory phase is similar to that of other hallucinogens previously described in this chapter. Prolonged sleep with A. muscaria ingestion requires only observation or supportive care. Tonic-clonic seizures are reported, but occurrences are rare.68
References
1. Nichols, DE. Hallucinogens. Pharmacol Ther. 2004;101:131.
2. Gertsch, JH, Wood, C. Case report: An ingestion of Hawaiian Baby Woodrose seeds associated with acute psychosis. Hawaii Med J. 2003;62:127.
3. Schwartz, RH, Smith, DE. Hallucinogenic mushrooms. Clin Pediatr. 1988;27:70.
4. Weil, AT, Davis, W. Bufo alvarius: A potent hallucinogen of animal origin. J Ethnopharmacol. 1994;41:1.
5. Shulgin, AT. N,N-Diisopropyltryptamine (DIPT) and 5-methoxy-N,N-diisopropyltryptamine (5-MeO-DIPT): Two orally active tryptamine analogs with CNS activity. Commun Psychopharmacol. 1980;4:363.
6. Meatherall, R. Foxy, a designer tryptamine hallucinogen. J Anal Toxicol. 2003;27:313.
7. Glennon, RA. Do classical hallucinogens act as 5-HT2 agonists or antagonists? Neuropsychopharmacology. 1990;3:509.
8. Klock, JC, et al. Coma, hyperthermia and bleeding associated with massive LSD overdose: A report of eight cases. J Toxicol Clin Toxicol. 1975;8:191.
9. Hill, SL, Thomas, SH. Clinical toxicology of newer recreational drugs. Clin Toxicol (Phila). 2011;49:705.
10. Hall, AP, Henry, JA. Acute toxic effects of “Ecstasy” (MDMA) and related compounds: Overview of the pathophysiology and clinical management. Br J Anaesth. 2006;96:678.
11. Voorspoels, S, et al. Resurgence of a lethal drug: Paramethoxyamphetamine deaths in Belgium. J Toxicol Clin Toxicol. 2002;40:203.
12. Byard, RW, et al. Death and paramethoxyamphetamine—an evolving problem. Med J Aust. 2002;176:496.
13. Prosser, JM, Nelson, LS. The toxicology of bath salts: a review of synthetic cathinones. J Med Toxicol. 2012;8:33–42.
14. Elliott, S, Smith, C. Investigation of the first deaths in the United Kingdom involving the detection and quantitation of the piperazines BZP and 3-TFMPP. J Anal Toxicol. 2008;32:172.
15. Baumann, MH, et al. N-Substituted piperazines abused by humans mimic the molecular mechanism of 3,4-methylenedioxymethamphetamine (MDMA, or “Ecstasy”). Neuropsychopharmacology. 2005;30:550.
16. McKenna, A, Nordt, SP, Ryan, J. Acute nutmeg poisoning. Eur J Emerg Med. 2004;11:240.
17. Forrester, MB. Nutmeg intoxication in Texas, 1998-2004. Hum Exp Toxicol. 2005;24:563.
18. Easton, N, Marsden, CA. Ecstasy: Are animal data consistent between species and can they translate to humans? J Psychopharmacol. 2006;20:194.
19. Ricaurte, GA, et al. (+/−)3,4-Methylenedioxymethamphetamine selectively damages serotonergic neurons in nonhuman primates. JAMA. 1988;260:51.
20. Ricaurte, GA, et al. Toxic effects of MDMA on central serotonergic neurons in the primate: Importance of route and frequency of drug administration. Brain Res. 1988;446:165.
21. Gouzoulis-Mayfrank, E, Daumann, J. Neurotoxicity of methylenedioxyamphetamines (MDMA; ecstasy) in humans: How strong is the evidence for persistent brain damage? Addiction. 2006;101:348.
22. Malberg, JE, Seiden, LS. Small changes in ambient temperature cause large changes in 3,4-methylenedioxymethamphetamine (MDMA)–induced serotonin neurotoxicity and core body temperature in the rat. J Neurosci. 1998;18:5086.
23. Farfel, GM, Seiden, LS. Role of hyperthermia in the mechanism of protection against serotonergic toxicity: II. Experiments with methamphetamine, p-chloroamphetamine, fenfluramine, dizocilpine and dextromethorphan. J Pharmacol Exp Ther. 1995;272:868.
24. Hartung, TK, et al. Hyponatraemic states following 3,4-methylenedioxymethamphetamine (MDMA, “ecstasy”) ingestion. QJM. 2002;95:431.
25. Henry, JA, et al. Low-dose MDMA (“ecstasy”) induces vasopressin secretion. Lancet. 1998;351:1784.
26. Holden, R, Jackson, MA. Near-fatal hyponatraemic coma due to vasopressin over-secretion after “ecstasy” (3,4-MDMA). Lancet. 1996;347:1052.
27. Randall, T. Ecstasy-fueled “rave” parties become dances of death for English youths. JAMA. 1992;268:1505.
28. Zhao, H, et al. Profiles of urine samples taken from Ecstasy users at rave parties: Analysis by immunoassays, HPLC, and GC-MS. J Anal Toxicol. 2001;25:258.
29. Boyer, EW. Dextromethorphan abuse. Pediatr Emerg Care. 2004;20:858.
30. Javitt, DC, Zukin, SR. Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry. 1991;148:1301.
31. Cook, CE, et al. Phencyclidine and phenylcyclohexane disposition after smoking phencyclidine. Clin Pharmacol Ther. 1982;31:635.
32. Young, JD, Crapo, LM. Protracted phencyclidine coma from an intestinal deposit. Arch Intern Med. 1992;152:859.
33. Schneider, SM, et al. Dextromethorphan poisoning reversed by naloxone. Am J Emerg Med. 1991;9:237.
34. McCarron, MM, et al. Acute phencyclidine intoxication: Incidence of clinical findings in 1,000 cases. Ann Emerg Med. 1981;10:237.
35. McCarron, MM. Phencyclidine intoxication. Dig Emerg Med Care. 1985;5:4.
36. Barton, CH, et al. Rhabdomyolysis and acute renal failure associated with phencyclidine intoxication. Arch Intern Med. 1980;140:568.
37. Wolfe, TR, Caravati, EM. Massive dextromethorphan ingestion and abuse. Am J Emerg Med. 1995;13:174.
38. Pender, ES, Parks, BR. Toxicity with dextromethorphan-containing preparations: A literature review and report of two additional cases. Pediatr Emerg Care. 1991;7:163.
39. Ly, BT, Thornton, SL, Buono, C, Stone, JA, Wu, AH. False-positive urine phencyclidine immunoassay screen result caused by interference by tramadol and its metabolites. Ann Emerg Med. 2012;59:545.
40. Ng, YY, et al. Spurious hyperchloremia and decreased anion gap in a patient with dextromethorphan bromide. Am J Nephrol. 1992;12:268.
41. Nahas, GG. Cannabis: Toxicological properties and epidemiological aspects. Med J Aust. 1986;145:82.
42. Wall, ME, et al. Metabolism, disposition, and kinetics of delta-9-tetrahydrocannabinol in men and women. Clin Pharmacol Ther. 1983;34:352.
43. Rules and regulations. Fed Regist. 2011;76(40):11075–11078.
44. Seely, KA, Prather, PL, James, LP, Moran, JH. Marijuana-based drugs: Innovative therapeutics or designer drugs of abuse? Mol Interv. 2011;22:36.
45. Heishman, SJ, et al. Acute and residual effects of marijuana: Profiles of plasma TCH levels, physiological, subjective and performance measures. Pharmacol Biochem Behav. 1990;37:561.
46. Renier, S, Messi, G, Orel, P. Acute cannabis poisoning in a female child. Minerva Pediatr. 1994;46:335.
47. Weinberg, D, Lande, A, Hilton, N. Intoxication from accidental marijuana ingestion. Pediatrics. 1983;71:848.
48. Macnab, A, Anderson, E, Susak, L. Ingestion of cannabis: A cause of coma in children. Pediatr Emerg Care. 1989;5:238.
49. Schneir, AB, Cullen, J, Ly, BT. Spice girls: Synthetic cannabinoid intoxication. J Emerg Med. 2011;40:296.
50. Ellis, GM, et al. Excretion patterns of cannabinoid metabolites after last use in a group of chronic uses. Clin Pharmacol Ther. 1985;38:572.
51. Cone, EJ, et al. Passive inhalation of marijuana smoke: Urinalysis and room air levels of delta-9-tetrahydrocannabinol. J Anal Toxicol. 1987;11:89.
52. Rossi, S, et al. Characterization of interference with 6 commercial Δ9-tetrahydrocannabinol immunoassays by efavirenz (glucuronide) in urine. Clin Chem. 2006;52:896.
53. Busse, F, et al. Lead poisoning due to adulterated marijuana. N Engl J Med. 2008;358:1641.
54. Valdes, LJ. Salvia divinorum and the unique diterpene hallucinogen, Salvinorin (divinorin) A. J Psychoactive Drugs. 1994;26:277.
55. Salvia divinorum. www.justice.gov/dea/concern/salvia_divinorum.html.
56. Cunningham, CW, Rothman, RB, Prisinzano, TE. Neuropharmacology of the naturally occurring K-opioid hallucinogen Salvinorin A. Pharmacol Rev. 2011;63:316.
57. Babu, KM, McCurdy, CR, Boyer, EW. Opioid receptors and legal highs: Salvia divinorum and Kratom. Clin Toxicol (Phila). 2008;46:146.
58. Chittrakarn, S, et al. Inhibitory effects of kratom leaf extract (Mitragyna speciosa Korth.) on the rat gastrointestinal tract. J Ethnopharmacol. 2008;116:173.
59. Boyer, EW, Babu, KM, Macalino, GE. Self-treatment of opioid withdrawal with a dietary supplement, Kratom. Am J Addict. 2007;16:352.
60. Kapp, FG, Maurer, HH, Auwarter, V, Winkelmann, M, Hermanns-Clausen, M. Intrahepatic cholestasis following abuse of powdered Kratom (Mitragyna speciosa). J Med Toxicol. 2011;7:227.
61. Nelsen, JL, Lapoint, J, Hodgman, MJ, Aldous, KM. Seizure and coma following Kratom (Mitragyna speciosa Korth) exposure. J Med Toxicol. 2010;6:424.
62. McWhirter, L, Morris, S. A case report of inpatient detoxification after Kratom (Mitragyna speciosa) dependence. Eur Addict Res. 2010;16:229.
63. Alper, KR, Lotsof, HS, Kaplan, CD. The ibogaine medical subculture. J Ethnopharmacol. 2008;115:9.
64. Höld, KM, Sirisoma, NS, Ikeda, T, Narahashi, T, Casida, JE. α-Thujone (the active component of absinthe): γ-Aminobutyric acid type A receptor modulation and metabolic detoxification. Proc Natl Acad Sci U S A. 2000;97:3826.
65. Padosch, SA, Lachenmeier, DW, Kröner, LU. Absinthism: A fictitious 19th century syndrome with present impact. Subst Abuse Treat Prev Policy. 2006;1:14.
66. Weisbord, SD, Soule, JB, Kimmel, PL. Poison online—acute renal failure caused by oil of wormwood purchased through the Internet. N Engl J Med. 1997;337:825.
67. Michelot, D, Melendez-Howell, LM. Amanita muscaria: Chemistry, biology, toxicology, and ethnomycology. Mycol Res. 2003;107:131.
68. Berger, KJ, Guss, DA. Mycotoxins revisited: Part II. J Emerg Med. 2005;28:175.