26 Hair Reduction with Lasers
Since the first FDA-approved laser hair reduction (LHR) device was introduced in 1995, LHR has become one of the most commonly performed cosmetic procedures with over 1 million treatments annually, according to statistics from the American Society for Aesthetic Plastic Surgery.1 Much of the popularity surrounding LHR can be attributed to its efficacy and excellent safety profile, with minimal discomfort and downtime.2
Laser Principles
Laser hair removal is based on the principle of selective photothermolysis, which is the conversion of laser energy to heat, to selectively destroy hair follicles without damaging the surrounding skin tissues. To achieve this effect, laser energy is first absorbed by melanin, the target chromophore in hair. The energy absorbed by melanin is then converted into heat, which subsequently damages the hair growth structures. The surrounding skin, which minimally absorbs energy, remains unaffected.3,4
Several device parameters affect the safety and efficacy of LHR. These parameters include wavelength, fluence, pulse duration, and spot size (see Laser Parameters in Chapter 19, Aesthetic Principles and Consultation).
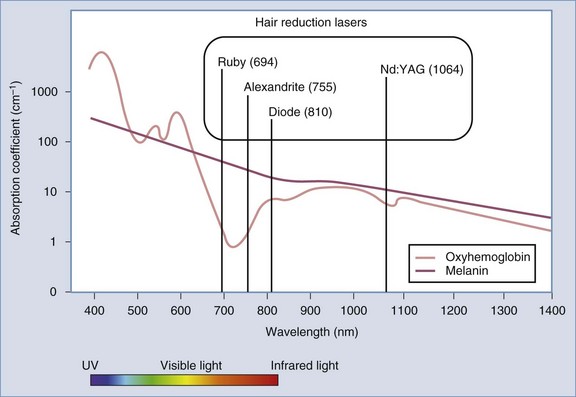
To target the hair follicle, wavelength selection should be specific for melanin, which preferentially absorbs laser energy between 650 and 1100 nm (Figure 26-1). These longer wavelengths also penetrate deeper into the skin to better target the hair follicles and facilitate hair removal. Four main lasers fall within this wavelength spectrum: ruby (694 nm), alexandrite (755 nm), diode (810 nm), and Nd:YAG (1064 nm) (see Figure 26-1). Whereas lasers emit single wavelengths of light energy, intense pulsed light (IPL) devices emit polychromatic light in a broad wavelength spectrum, typically between 400 and 1400 nm. Both lasers and IPL devices (collectively referred to as lasers*) used for hair reduction operate under the principle of selective photothermolysis.5
Pulse duration is the amount of time the laser pulse is applied to the skin (typically in milliseconds). To confine thermal damage due to laser light energy to the desired target hair follicle, the pulse duration must be shorter than or equal to the thermal relaxation time of the follicle, typically between 10 and 100 ms (see Laser Parameters in Chapter 19 for a discussion of thermal relaxation time). Longer pulse durations are used with coarse (i.e., thick), dark hairs and for areas with high hair density. Shorter pulse durations are used for fine (i.e., thin), light hairs and areas with low hair density. Figure 26-2 summarizes the fluences and pulse durations that are used based on hair characteristics. In addition, longer pulse widths penetrate deeper into the skin and are safer for the epidermis. Therefore, darker skin types are treated with longer pulse widths and lighter skin types are treated with shorter pulse widths.
Patient Selection
Proper patient selection based on an individual’s Fitzpatrick skin type, hair color, coarseness, and density is crucial for achieving successful treatments. (Refer to Chapter 19 for a review of Fitzpatrick skin types.) The ideal candidate for LHR possesses fair skin and dark, coarse hair. Fair-skin individuals (Fitzpatrick skin types I to III) have little to no epidermal melanin, which, if present, can serve as a competing target for laser energy. Thus, darker skin types (IV to VI) are at greater risk of epidermal injury with LHR treatments. Patients with Fitzpatrick skin types VI pose the greatest challenge to treatment and have the highest risk of complications, and recommendations for treatment are outside the scope of this chapter. White, light-colored (i.e., gray, blonde), and fine vellus hair lack melanin target in the hair follicle, and patients with these hair characteristics are poor candidates for LHR.
Patient Expectations
Candidates for LHR should expect to undergo several treatments in order to achieve optimal results. Because hair growth is asynchronous and LHR is most effective for hair follicles in the anagen phase (see below), patients can expect, on average, 20% to 30% permanent hair reduction after one treatment and up to 60% to 90% reduction after completing a treatment series.6 Typically, individuals with Fitzpatrick skin types I to III require a series of six sessions, whereas skin types IV and V require eight sessions or more because treatment fluences are increased more slowly and conservatively over time with darker skin types to minimize the risk of complications.7
Products Currently Available
A wide selection of hair removal lasers and IPL devices are available and vary by their emitted wavelengths, peak fluences, pulse durations, spot size, and cooling methods (see the Resources section at the end of the chapter for a list of suppliers).
Alexandrite lasers (755 nm) for hair reduction are commonly used for lighter skin types (I through III).8 Relative to ruby lasers, this wavelength is safer, because it is less strongly absorbed by melanin and penetrates deeper into the epidermis. However, it is still a shorter wavelength than others used for LHR and complications such as postinflammatory hyperpigmentation can occur with darker skin types. Alexandrite devices have the advantage of being easy to use with flexible fiber-optic arms. These devices typically use cryogen spray or cool air as a means of cooling the epidermis.
Diode lasers (810 nm) are popular LHR devices that are highly effective on coarse dark hair. Darker skin types can be treated more safely than with alexandrite lasers due to the longer wavelength with deeper penetration, longer pulse widths and contact cooling of the laser tip.6 These devices also have the advantage of not having disposable parts and are small enough to sit on a tabletop.
Neodymium-doped yttrium aluminum garnet or Nd:YAG lasers (1064 nm) can be used for LHR in all skin types and are the safest devices for darker skin types (V and VI). This long wavelength is deeply penetrating, which aids in hair reduction. It has relatively poor melanin absorption and, while this protects the skin from epidermal injury, reduced melanin absorption is a disadvantage for LHR treatments. This can be overcome with the use of high fluences, coupled with intense epidermal cooling, to adequately damage hair growth structures.9
Q-switched Nd:YAG lasers, previously thought to provide only for temporary hair reduction, have recently been found to achieve permanent reduction of fine dark hair.10 The short pulse widths of these lasers (in the nanosecond range) cause mechanical oscillation of the target, also known as photoacoustic vibration. Damage to the hair follicle results from both photothermolysis and photoacoustic vibration. These lasers are most useful for the treatment of fine dark hairs, particularly on the face, and can be used with all skin types.
Intense pulsed light devices emit noncoherent, multiwavelength light ranging from 400 to 1200 nm. Cutoff filters are used to eliminate short wavelengths and allow for peaks of emission at certain desired wavelengths. For example, IPLs used for hair reduction will often use a filter that cuts off all wavelengths below 590 nm and allows for a wavelength peak between 600 and 800 nm. In this way, IPL devices can target the melanin chromophore and penetrate deeply into the skin.11 IPL devices have either single or multipulse modes (see Chapter 19). One head-to-head study showed similar clinical efficacy in hair reduction with diode, alexandrite, and IPL devices.12 Some devices are now available that combine IPL and 1064 nm to allow for treatment of a wide spectrum of skin types and hair characteristics.
Contraindications
General Laser Contraindications
The following contraindications apply to LHR and the laser treatments discussed in Chapters 27 through 30:
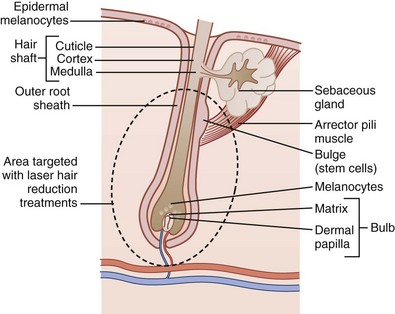
Anatomy
Hair follicles are composed of the bulb (which consists of the matrix and dermal papilla), outer root sheath, bulge, and hair shaft (Figure 26-3). The hair matrix depth in the skin ranges from 2 to 7 mm, depending on the body location, and the hair bulge is approximately 1.5 mm. Hair growth occurs in three phases with distinct changes below the skin in the hair bulb: (1) anagen, the active growth phase during which the hair bulb is most darkly pigmented; (2) catagen, the regression phase when cell division ceases and the follicle begins to involute; and (3) telogen, the resting phase during which the hair bulb is minimally pigmented (Figure 26-4). The hair shaft visible on the surface of the skin, however, is indistinguishable throughout these phases.
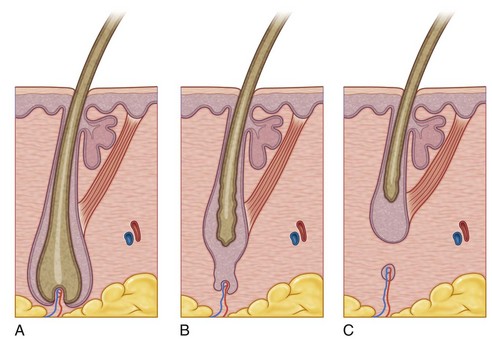
FIGURE 26-4 Three phases of hair growth: (A) anagen, (B) catagen, and (C) telogen.
(From Robinson J, Hanke W, Sengelmann R, Siegel D. Surgery of the Skin: Procedural Dermatology, 2nd ed. Philadelphia: Mosby; 2010.)
Hair growth is initiated by epithelial stem cells located in the “bulge,” a protrusion near the attachment of the arrector pili muscle, and also occurs from the rapidly dividing matrix cells of the hair bulb. Hairs are most susceptible to laser treatment during the early anagen phase when the melanin content of the matrix is greatest. The percentage of hairs in anagen varies for different parts of the body (Table 26-1), and those areas with the greatest percentage in anagen, such as the scalp, respond most rapidly to laser treatments. The duration of the telogen phase serves as a rough guideline for the interval between treatments. For example, the lower legs, which have a long telogen phase, require intervals of approximately 3 months between treatments, whereas the upper lip, which has a short telogen phase, requires approximately 1 month between treatments (Table 26-1).
TABLE 26-1 Percentage of Hairs in Anagen and Duration of Telogen Phase for Different Body Areas
|
Body Area |
Anagen Hair (%) |
Telogen Duration (months) |
|---|---|---|
| Scalp | 85 | 3 to 4 |
| Beard | 70 | 2.5 |
| Upper lip | 65 | 1.5 |
| Axillae | 30 | 3 |
| Pubic area | 30 | 3 |
| Arms | 20 | 4.5 |
| Lower legs | 20 | 6 |
Procedure Preparation
Laser Hair Reduction: Steps and Principles7
General Treatment Technique
Planning and Designing
A grid pattern may be drawn on the skin using a soft white pencil to help ensure complete coverage of the treatment area (Figure 26-5). This is particularly useful when treating large areas such as the leg and back.
Anesthesia
Discomfort associated with LHR treatment is usually likened to the snap of a rubber band. Because of the rich sensory nerve supply around hair follicles, LHR treatments are rarely free from pain. Anesthesia requirements vary according to the equipment used, patients’ tolerance, and treatment area. Many LHR devices have built-in cooling mechanisms, such as a cooled sapphire window, that maintain the tip of the laser at a constant temperature. This provides epidermal contact cooling, which increases safety and provides some anesthesia. Some patients may require a topical anesthetic such as EMLA (prilocaine 21/2%:lidocaine 21/2%), ELA-Max (lidocaine 4%), or BLT (benzocaine 20%:lidocaine 6%:tetracaine 4%) (see Chapter 3, Anesthesia, and Chapter 20, Anesthesia for Cosmetic Procedures). All topical anesthetics are applied in the office for safety reasons.
The use of ice or cold packs is an excellent method of anesthesia and may be used for pretreatment and post-treatment cooling. A cryogen cooling spray or forced cool air is used by some devices for epidermal cooling during treatment, and these may also provide some pain reduction. Pneumatic skin flattening is a newer method of anesthesia whereby the tip of the laser compresses the skin using vacuum pressure, thereby reducing pain sensation (see Chapter 20).
Performing Laser Hair Reduction

FIGURE 26-6 Laser hair treatment clinical endpoints of erythema and singed hair.
(Copyright Rebecca Small, MD.)
Results
The greatest efficacy with permanent hair reduction is achieved with use of high fluences, a greater number of treatments, and adequately long intervals between treatments that approximate the telogen phase for the treatment area.6
Figure 26-9 shows hair reduction results for the anterior neck and chin (A) before and (B) after six treatments using an IPL (Starlux, Palomar).
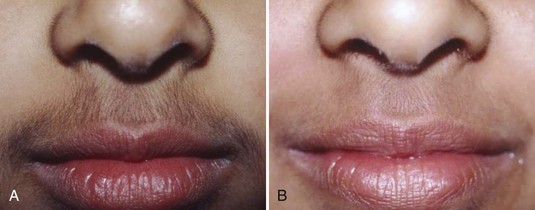
Figure 26-10 shows hair reduction results for fine dark upper lip hair in a darker Fitzpatrick skin type (A) before and (B) after a series of treatments using a Q-switched 1064 nm laser. This is one of the only laser devices that can reduce fine hairs (RevLite, HOYA ConBio).
Figure 26-11 shows hair reduction results for the jawline and sideburns (A) before and (B) after completion of a series of treatments using a 755 nm laser (GentleLase, Candela).
Figure 26-12 shows hair reduction results for the axilla (A) before and (B) after completion of a series of treatments using a 755 nm laser (GentleLase, Candela).
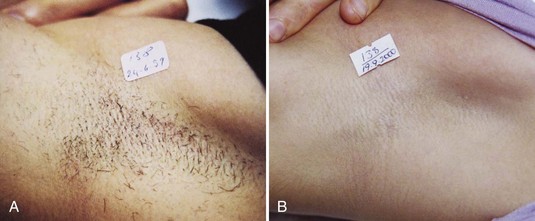
FIGURE 26-12 Axilla hair (A) before and (B) after completion of a series of hair reduction treatments with a 755 nm laser.
(Courtesy of Candela, Wayland, MA; M. Ercan, MD, using laser.)
Figure 26-13 shows hair reduction results for pseudofolliculitis barbae in a patient with Fitzpatrick skin type VI (A) before and (B) after a series of treatments using a 1064 nm long-pulse laser (ClearScan YAG, Sciton).
Complications
Rare and Idiosyncratic Complications
Pigmentary complications are most commonly seen in darker Fitzpatrick skin types (IV and V) and in patients with a recent tan. These complications typically occur with short pulse widths and/or high fluences and poor epidermal cooling. Hyperpigmentation and hypopigmentation are usually transient, lasting on the order of months, and rarely may be permanent. The use of a lightening agent such as hydroquinone for 1 month prior to treatment and after treatment may reduce hyperpigmentation, particularly in darker skinned patients (see Chapter 24, Skin Care Products, for additional information).
A burn can result from aggressive treatment parameters of short pulse widths and high fluences with inadequate epidermal cooling. Figure 26-14 shows an erythematous area with crusting on the back 1 week after a laser hair reduction treatment. Routine moist wound care is performed with application of an antibiotic ointment and bandage until healed. Scarring is highly unlikely, but may occur with overaggressive treatments and with treatments complicated by infection.
Herpes simplex and varicella zoster may be reactivated in the treatment area, and pretreatment prophylactic antiviral medication can reduce this risk (see the Procedure Preparation section above). Impetigo may occur, particularly with treatments around the mouth. Folliculitis may also occur, particularly after vigorous exercise, swimming or hot tub use immediately after treatments (Figure 26-15).
Hair grows at an angle to the skin and it is possible to unintentionally reduce hair growth adjacent to the treated area. Providers are cautioned against treating near the eyebrows for this reason. Paradoxical hair growth has been described, whereby LHR treatments stimulate hair growth. In this case, LHR may cause conversion of vellus hairs to coarse terminal hairs in the treatment area, or stimulate fine hair growth adjacent to the treatment area. Most cases are reported in skin types IV through VI, particularly with treatment of fine hairs in the lateral face.14 One study found that immediate application of ice around the treatment area and two passes of the laser in the treatment area reduced the risk of paradoxical hair growth.15
Erythema ab igne and livedo reticularis are extremely rare, as is bruising, pruritus, and urticaria.
Special Populations
Current Developments
Some of the newer laser hair reduction devices have larger treatment heads to shorten treatment times. Analgesic devices, such as pneumatic skin-flattening tips are available for LHR devices to reduce the discomfort associated with treatment16 (see Chapter 20, Anesthesia for Cosmetic Procedures). Recently, laser hair reduction devices have become available for use at home. One such device, Tria (by TriaBeauty), is a diode laser (810 nm) that has a long pulse width of 400 ms and low fluences of 7 to 20 J/cm2. Another device, Silk’n (by Home Skinovations), is an IPL with a pulsewidth of less than 1 ms and low fluences of 3-5 J/cm2. Data is limited on these devices and they will likely provide temporary hair reduction given their limited treatment parameters.
Financial Considerations
LHR is not reimbursable by insurance. The charges for treatments are usually based on the size of the treatment area and are largely determined by local prices. Patients may pay for individual treatments. However, because LHR is only effective with a series of treatments, packages of treatments (usually six) may be offered so that patients achieve the best possible results and have the greatest satisfaction. Box 26-1 lists applicable codes for LHR procedures.
Resources
See the Aesthetics Buyers Guide (www.miinews.com/productcharts.php) for specific laser technologies made by laser companies.
1. Cosmetic Surgery National Data Bank 2010 Statistics. American Society for Aesthetic Plastic Surgery; 2010.
2. Small R. Aesthetic procedures in office practice. Am Fam Physician. 2009;80(11):1231-1237.
3. Altschuler GB, Anderson RR, Manstein D, et al. Extended theory of selective photothermolysis. Lasers Surg Med. 2001;29:416-432.
4. Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983;220(4596):524-527.
5. Dierickx CC. Hair removal by lasers and intense pulsed light sources. Semin Cutan Med Surg. 2000;19(4):267-275.
6. Lou WW, Quintana AT, Geronemus RG, et al. Prospective study of hair reduction by diode laser (800 nm) with long-term follow-up. Dermatol Surg. 2000;26(5):428-432.
7. Small R. Laser hair removal. In: Mayeaux E, editor. The Essential Guide to Primary Care Procedures. Philadelphia: Lippincott Williams & Wilkins; 2009:234-248.
8. Gorgu M, Aslan G, Akoz T, et al. Comparison of alexandrite laser and electrolysis for hair removal. Dermatol Surg. 2000;26:37-41.
9. Battle EF, Hobbs LM. Laser-assisted hair removal for darker skin types. Dermatol Ther. 2004;17:177-183.
10. Bakus AD, Garden JM, Yaghmai D, Massa MC. Long-term fine caliber hair removal with an electro-optic Q-switched Nd:YAG Laser. Laser Surg Med. 2010;42:706-711.
11. Gold MH, Bell MW, Foster TD, et al. One-year follow-up using an intense pulsed light source for long-term hair removal. J Cutan Laser Ther. 1999;1(3):167-171.
12. Amin SP, Goldberg DJ. Clinical comparison of four hair removal lasers and light sources. J Cosmet Laser Ther. 2006;8(2):65-68.
13. Small R. Aesthetic procedures introduction. In: Mayeaux E, editor. The Essential Guide to Primary Care Procedures. Philadelphia: Lippincott Williams & Wilkins; 2009:195-199.
14. Alajlan A, Shapiro J, Rivens J, et al. Paradoxical hypertrichosis after laser epilation. J Am Acad Dermatol. 2005;53:85-88.
15. Willey A, Torrontegui J, Azpiazu J, et al. Hair stimulation following laser and intense pulsed light photo-epilation: review of 543 cases and ways to manage it. Lasers Surg Med. 2007;39:297-301.
16. Bernstein EF. Pneumatic skin flattening reduced pain during laser hair reduction. Lasers Surg Med. 2008;40:183-187.
Page G. Lasers and pulsed-light devices: hair removal. In Pfenninger JL, Fowler GC, editors: Pfenninger and Fowler’s Procedures for Primary Care, 3rd ed, Philadelphia: Mosby/Elsevier, 2011.
Small R. Laser hair reduction. In: Small R, editor. A Practical Guide to Cosmetic Lasers. Philadelphia: Lippincott Williams & Wilkins, 2012.








 % hydrocortisone cream two to three times per day for 3 to 4 days or until resolved. Singed hairs may be evident immediately after treatment, and treated hairs may extrude 1 to 2 weeks after treatment. A washcloth may be used to wipe these hairs off in the direction of the hair follicles. Postinflammatory hyperpigmentation can occur with prolonged erythema, and patients are instructed to contact their provider if erythema persists for more than 5 days. Daily use of a full-spectrum sunscreen (SPF 30 with zinc or titanium) and sun avoidance for 4 weeks after treatment helps minimize the risk of pigmentary changes. If blistering and/or crusting occur, manage with moist wound care using bacitracin and a bandage until healed.
% hydrocortisone cream two to three times per day for 3 to 4 days or until resolved. Singed hairs may be evident immediately after treatment, and treated hairs may extrude 1 to 2 weeks after treatment. A washcloth may be used to wipe these hairs off in the direction of the hair follicles. Postinflammatory hyperpigmentation can occur with prolonged erythema, and patients are instructed to contact their provider if erythema persists for more than 5 days. Daily use of a full-spectrum sunscreen (SPF 30 with zinc or titanium) and sun avoidance for 4 weeks after treatment helps minimize the risk of pigmentary changes. If blistering and/or crusting occur, manage with moist wound care using bacitracin and a bandage until healed.







