Haemoptysis
Haemoptysis is the expectoration of blood or bloodstained sputum. With massive haemoptysis, the main priorities are to secure the airway and initiate emergency resuscitative measures before establishing a diagnosis.
History
Onset
Sudden onset of haemoptysis can occur with pulmonary embolism and acute respiratory tract infections; the remaining conditions tend to pursue chronic recurrent courses. Although the amount of blood expectorated is not very useful as a discriminating feature, small amounts of blood sufficient to stain the sputum pink are characteristic of pulmonary oedema.
Acute onset of cough with haemoptysis may occur with respiratory tract infections and pulmonary embolism. Associated sputum production may be purulent and longstanding with chronic bronchitis and bronchiectasis. This is accompanied by flecks of blood when lung carcinoma, TB or mitral stenosis is present.
Dyspnoea
A long history of dyspnoea may be associated with chronic lung disease or mitral stenosis. Acute onset of dyspnoea that occurs with pulmonary embolism may be accompanied by pleuritic chest pain. Dyspnoea that is associated with pulmonary oedema may have a variable speed of onset and is often worse on recumbency.
Weight loss
Progressive weight loss is suggestive of TB or bronchial carcinoma, especially with a background of heavy smoking. Night sweats may be an additional accompanying feature of TB.
Other sites of bleeding
Other bleeding sites should be excluded as haematuria may be due to Goodpasture’s syndrome. Epistaxis and haemoptysis occur together with Wegener’s granulomatosis and hereditary haemorrhagic telangiectasia. Epistaxis per se may occasionally be confused with haemoptysis when expectorated sputum is mixed with blood originating from the nasal passages.
Past medical and drug history
A careful history is taken to identify a generalised coagulation disorder. This may be congenital, such as haemophilia, or acquired, such as with the use of anticoagulant drugs or in DIC. Previous rheumatic fever predisposes an individual to mitral stenosis. Consider Goodpasture’s syndrome and Wegener’s granulomatosis in the presence of co-existing renal disease.
Examination
Inspection
Cachexia is a prominent feature of carcinoma, TB and chronic lung disease. Loss of the nasal bridge and saddling of the nose may be apparent in patients with Wegener’s granulomatosis. The presence of clubbing (p. 64) is associated with bronchial carcinoma, chronic bronchitis and bronchiectasis. The malar flush characteristic of mitral facies may be present with mitral stenosis. Small dilated blood vessels present on the mucous membranes are features of hereditary haemorrhagic telangiectasia. The JVP may be elevated with a large pulmonary embolus or accompanying congestive cardiac failure secondary to mitral stenosis. The chest may be hyperexpanded with decreased inspiratory movement in chronic bronchitis.
Palpation
During an acute episode, tachycardia is very common. This may be due to the effort of coughing, anxiety or blood loss. The presence of an irregular heartbeat of atrial fibrillation is associated with mitral stenosis. Moreover, patients with atrial fibrillation are usually on anticoagulant therapy. Supraclavicular lymphadenopathy may be present with pulmonary infections or carcinoma. The calves should be palpated and measured for tenderness and increased girth from deep venous thrombosis, which may give rise to pulmonary emboli.
Percussion and auscultation
Localised crepitations and bronchial breathing may be audible with lobar pneumonia. Generalised coarse crepitations are suggestive of bronchiectasis, pulmonary oedema and chronic bronchitis. Breath sounds tend to be decreased in intensity with chronic bronchitis. Patients with bronchial carcinoma may present with a number of clinical features from the primary tumour, such as wheezing due to large airway obstruction, pulmonary collapse, pleural effusion and superior vena cava obstruction. On auscultation of the mitral area, the loud first heart sound and mid-diastolic rumbling murmur of mitral stenosis is accentuated on expiration with the patient in a left lateral position.
General Investigations
■ Sputum analysis
Sputum should be collected for microscopy, culture and cytology. Infective organisms may be isolated or cytological features of malignancy may be present. When TB is suspected, serial cultures should be taken from sputum, urine, bronchial washings or lung biopsy specimens during bronchoscopy. Polymerase chain reaction amplification techniques may also be performed on cultured specimens to provide a more rapid diagnosis.
■ ECG
Sinus tachycardia may be noted with violent coughing, anxiety and blood loss. S1Q3T3 is indicative of right heart strain with pulmonary embolism, although non-specific ST abnormalities are more common.
■ FBC
Hb ↓ with chronic haemoptysis resulting in iron deficiency anaemia. Acute bleeding may not be associated with changes in the blood count until 24 hours later. WCC ↑ may be due to acute bleeding or respiratory tract infection. Monocytosis may be a feature of TB. Platelets ↓ with blood dyscrasias.
■ U&Es
The presence of impaired renal function with deranged urea and creatinine estimations may be due to glomerulonephritis from Goodpasture’s syndrome or Wegener’s granulomatosis. However, pre-renal failure may also be precipitated by acute blood loss and volume depletion.
■ Clotting screen
A clotting screen is performed to identify any impairment that may prolong the PT or APTT.
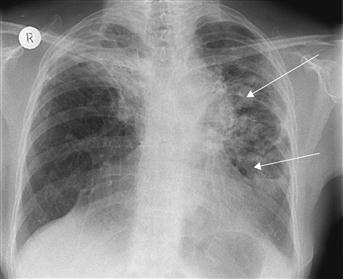
■ CXR
Bilateral patchy areas of consolidation may be seen on a chest film with bronchopneumonia and pulmonary oedema. Opacification of an entire lobe suggests lobar pneumonia, although pulmonary emboli may have a similar appearance due to the wedge-shaped shadowing of a pulmonary infarct. Recurrent fluffy shadowing may be seen with Goodpasture’s syndrome and Wegener’s granulomatosis, due to repeated intra-alveolar haemorrhage. The primary focus of tuberculous infection is usually in the middle to upper zones of the lung. This may resolve, with variable amounts of calcification, whereas post-primary TB tends to present with the classical apical shadow. The chest film may be normal with uncomplicated chronic bronchitis; however, with bronchiectasis, visibly dilated bronchi with persistent consolidation may be prominent. With bronchial carcinoma, numerous features may be seen on a chest radiograph, such as a peripheral mass, a hilar mass, collapse of a lobe or pleural effusion. The double right heart border and tenting of the left heart border are all features of enlargement of the left atrium with mitral stenosis. When pulmonary hypertension is present, there may be dilatation of the central pulmonary arteries with right ventricular enlargement.
■ Bronchoscopy
Fibreoptic bronchoscopy is useful for locating the site of bleeding. In addition, biopsies of the bleeding site may be sampled for pathological analysis. Multiple arteriovenous malformations will be visible with hereditary haemorrhagic telangiectasia.
Specific Investigations
■ Mantoux test
When TB is suspected, an initial dilute Mantoux test (1 in 10 000) may be performed in individuals who have not received BCG immunisation.
■ Urinalysis
May reveal the presence of protein and red cell casts with glomerulonephritis due to Goodpasture’s syndrome and Wegener’s granulomatosis.
■ Antiglomerular basement antibodies
Characterises Goodpasture’s syndrome.
■ c-ANCA
Wegener’s granulomatosis is associated with elevated levels.
■ Renal biopsy
Will aid in confirming the diagnosis in both Goodpasture’s syndrome and Wegener’s granulomatosis.
■ Tissue biopsies
Majority of lung cancers are diagnosed on CXR; a smaller proportion are diagnosed by cytology. Definitive tissue diagnosis can be made by biopsies from bronchoscopy, mediastinoscopy, CT-guided biopsy or surgical resection.
■ CT thorax/pulmonary angiogram
Very useful adjunct to the diagnosis of bronchiectasis in cases where the diagnosis cannot confidently be made on the clinical grounds and a chest film. It may also be useful in the staging of lung carcinomas. The CT pulmonary angiogram is currently the investigation of choice to screen for pulmonary embolism.
■ Echocardiography
Allows assessment of left ventricular function with pulmonary oedema. It may also aid in the diagnosis of pulmonary embolism, as right heart failure can occur with large emboli. The integrity of the cardiac valves can be assessed, and valve stenosis with restriction of movement of the mitral valve leaflets can be visualised in mitral stenosis.