Haematuria
Haematuria is the passage of red blood cells in the urine. Care must be taken to distinguish it from other causes of discoloration of urine. All patients with haematuria must be fully investigated. If haematuria has initially been diagnosed on dipstick testing, it must always be confirmed by microscopy.
History
Is there pain associated with haematuria to suggest infection or inflammation? Painless haematuria is usually associated with tumour or TB. Total haematuria (throughout the stream) suggests bleeding from the upper urinary tract or bladder. Initial haematuria (at the start of the stream) suggests bleeding from the urethra or the prostate. Terminal haematuria (at the end of the stream) suggests bleeding from the bladder or prostate. Check for a family history of polycystic kidney disease. There may be a history of TB elsewhere. Has there been any recent foreign travel (schistosomiasis)? Is there any pain in the loin to suggest kidney disease, or a history of ureteric colic to suggest passage of a stone or clot down the ureter? Bladder disease may be accompanied by suprapubic pain, frequency and dysuria. Catheter-associated haematuria may occur in patients with long-term indwelling bladder catheters. It is usually self-limiting. Check for symptoms of prostatism, i.e. difficulty in starting, poor stream and nocturia. Urethral injury will normally be apparent. It may occur following pelvic fractures or falling astride an object. Is the patient on anticoagulants? Is there any history of blood dyscrasia? Is there evidence of sickle cell disease or exposure to malaria? Strenuous exercise may cause haematuria. Has there been a recent renal biopsy? Discoloration of urine may be due to a variety of causes. Haemoglobinuria may occur with haemolysis and myoglobinuria following crush injuries or ischaemia of muscle. Check for ingestion of any substance that may change the colour of the urine. Acute intermittent porphyria is extremely rare and is accompanied by abdominal pain. If the urine from a patient is allowed to stand in the light, it will become purplish-red.
Examination
Anaemia, weight loss, signs of chronic renal failure. Abdominal examination may reveal a palpable mass, e.g. hypernephroma, distended bladder. Rectal examination may reveal smooth enlargement of the prostate (benign prostatic hypertrophy) or a hard, craggy prostate (carcinoma). Feel along the course of the urethra, e.g. stone or neoplasm. Examine the chest, e.g. TB, secondary deposits from carcinoma of the kidney. Check for any localised bone tenderness, e.g. secondary deposits from carcinoma of the prostate or hypernephroma.
General Investigations
■ FBC, ESR
Hb ↓ gross haematuria, malignancy. Hb ↑ polycythaemia associated with hypernephroma. WCC ↑ infection. Platelets ↓ blood dyscrasias. ESR ↑ malignancy, TB.
■ Urine microscopy
Red cells (excludes haemoglobinuria and ingestion of substances that cause discoloration of urine). White cells in infection. Organisms in infection. Cytology.
■ Clotting screen
Anticoagulant therapy. Blood dyscrasias.
■ CXR
Metastases (cannonball metastases with hypernephroma). TB.
Specific Investigations
■ Sickling test
Sickle cell disease.
■ US
Cystic versus solid. Stone. Urinary tract obstruction.
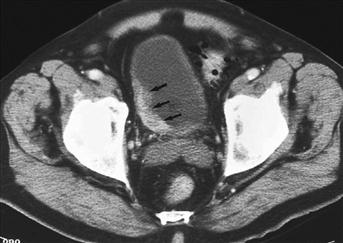
■ CT
Tumour (confirmation and degree of invasion). Cyst. Obstructive uropathy.
■ Cystoscopy
Infection. Tumour. Stone.
■ Ureteroscopy
Tumour. Obstruction.
■ Selective renal angiography
Vascular malformation. Tumour.