TOPIC 7 Haematology and coagulation
Common first tests
Test: Full blood count and peripheral blood smear (PBS)
Indications
How it is done
Interpretation
| Male | Female* | |
|---|---|---|
| Haemoglobin (g/dL) | 13–18.0 | 11.5–16.5 |
| RBCs (×1012/L) | 4.5–6.5 | 4.0–5.8 |
| Hct (%) | 0.40–0.52 | 0.37–0.47 |
| MCV (fL) | 84–96 | 84–96 |
| MCH (pg) | 27.0–32.0 | |
| MCHC (g/dL) | 27.0–32.0 | |
| Platelets (×109/L) | 150–400 | |
| WBCs (×109/L) | 4.0–11.0 | |
| Neutrophils (×109/L) | 2.0–7.5 | |
| Lymphocytes (×109/L) | 1.5–4.0 | |
| Monocytes (×109/L) | 0.2–0.8 | |
| Eosinophils (×109/L) | 0.04–0.4 | |
| Basophils (×109/L) | 0.0–0.1 | |
| Reticulocytes (% or 109/L) | 0.5–2.5 or 20–80 |
* In pregnancy the Hb may fall as low as 9 g/dL in the third trimester. RBCs, red blood cells; Hct, haematocrit; MCV, mean cell volume; MCH, mean cell haemoglobin; MCHC, mean corpuscular haemoglobin concentration; WBC, white blood cell.
Abnormalities
Polycythaemia: Increased haemoglobin/haematocrit
| True polycythaemia | Secondary polycythaemia | Apparent or spurious polycythaemia |
|---|---|---|
| Polycythaemia rubra vera, (PRV) | Inappropriate erythropoietin secretion in benign & malignant renal disorders and by some tumours | Secondary to cigarette smoking, obesity, excess alcohol or hypertension |
Leucopenia: WBC <4.0 × 109/L
| Neutropenia | Lymphopenia | |
|---|---|---|
| Congenital causes | Acquired causes | |
Leucocytosis
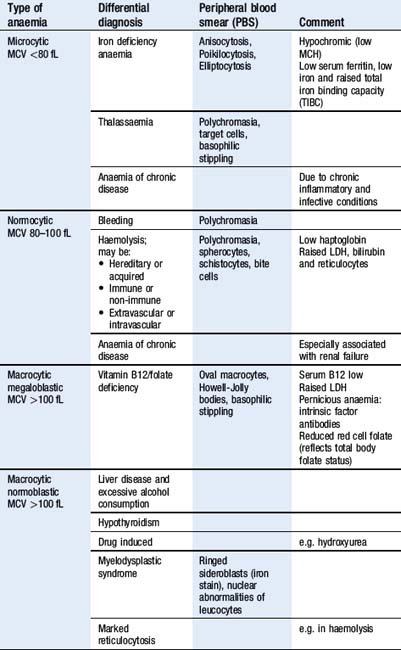
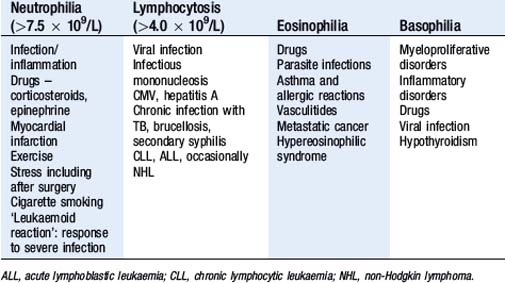
Detection of a leucocytosis by the automated counter needs confirmation with a PBS and manual count. See Table 7.7.
Management principles
Limitations and complications
Test: Group and screen/crossmatch
Indications
How it is done
Interpretation
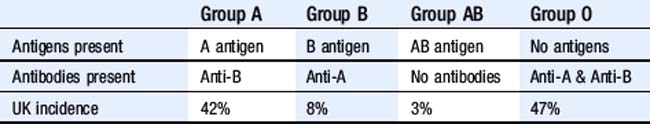
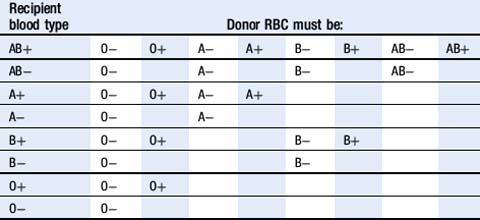
Physiological principles
Management principles
| Recipient blood type | Donor plasma must be: |
|---|---|
| AB | AB |
| A | A or AB |
| B | B or AB |
| O | O, A, B or AB |
Laboratory tests of coagulation
Tests: Prothrombin time (PT)/international normalized ratio (INR), activated partial thromboplastin time (APTT) and thrombin time (TT)
Indications
How it is done
Interpretation
Physiological principles
Abnormalities
| Prolonged INR | Prolonged APTT | Prolonged TT |
|---|---|---|
| Due to deficiency of factor I, II, V, VII or X: |
* Disseminated intravascular coagulopathy: DIC may complicate massive tissue injury, sepsis and some pregnancy-related complications. The normal anticoagulant and fibrinolytic systems are overwhelmed resulting in disseminated microvascular thrombi with consumption of platelets and coagulation factors leading to a haemorrhagic state. The fibrinolytic system is activated to dissolve the fibrin thrombi, resulting in the formation of D-dimers and fibrin degradation products (FDP), which have a further anticoagulant action.
Management principles
Limitations and complications
Management principles
Test: D-dimers and fibrin degradation products
Point-of-care tests of coagulation
Test: Activated clotting time (ACT)
Indications
How it is done
Haemoglobinopathies
Test: Sickledex
Interpretation
Physiological principles
Management principles
Viscoelastic measurement of haemostasis
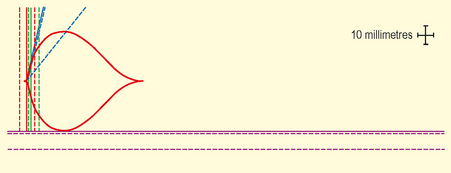
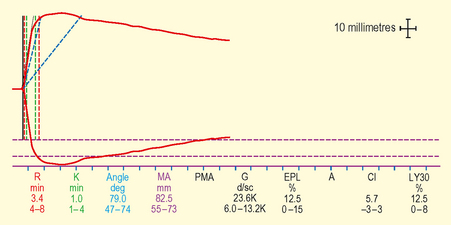
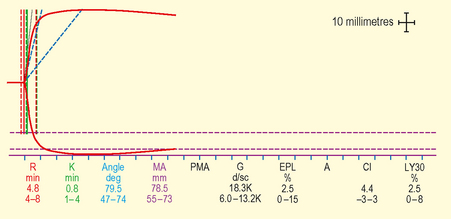
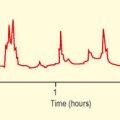
Test: Thromboelastography/thromboelastometry
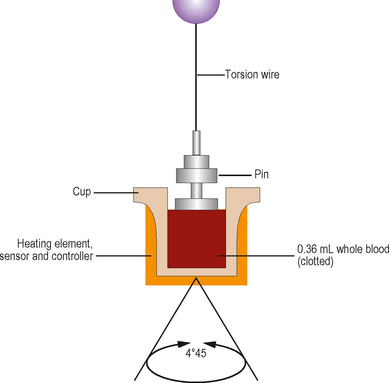
How it is done
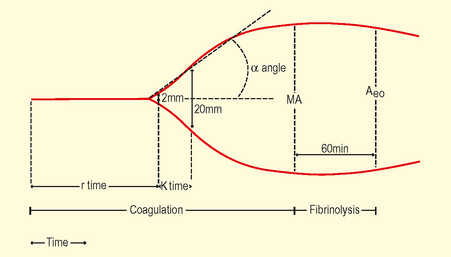
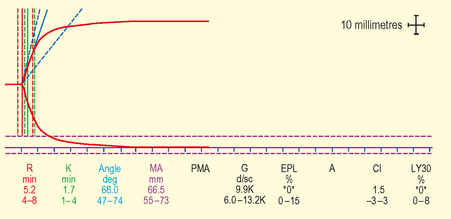
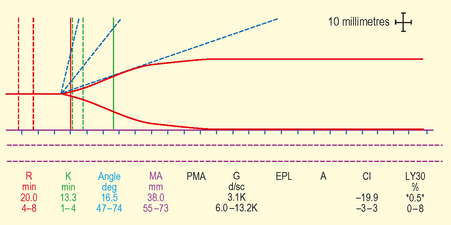
Interpretation
Data presented as
| TEG | ROTEM | |
|---|---|---|
| Measurement period | RT | |
| Clot time-latency time from placing blood in cup until clot starts to form (2 mm amplitude) | Reaction time r | Clotting time (CT) |
| Period from 2 mm to 20 mm Amplitude | K | Clot formation time (CFT) |
| Alpha angle | α | α |
| Maximum angle | Clot formation rate (CFR) | |
| Maximum strength | Maximum amplitude (MA) | Maximum clot firmness (MCF) |
| Time to maximum strength | TMA | MCF-t |
| Amplitude at set time | A30, A60 | A5, A10… |
| Clot elasticity | G | Maximum clot elasticity (MCE) |
| Maximum lysis | Maximum lysis (ML) | |
| Lysis at fixed time | LY30, LY60 | CL30, CL60 |
Physiological principles
Management principles
Laboratory platelet function monitors
Test: Optical light transmission platelet aggregometry (LTA)
How it is done
Point-of-care platelet function monitors
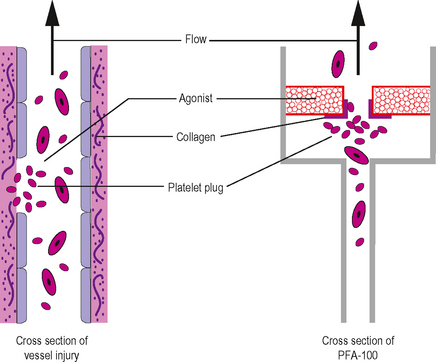
Test: PFA-100
Various point-of-care platelet function monitors are available. The PFA-100 is described in detail.