chapter 18 Gynecologic Assessment
Approach to the Physical Examination
An infant or very young child can be examined most easily while she is semirecumbent on her mother’s lap with her hips flexed and abducted. Put lateral and downward pressure on the labia majora so that you can visualize the introitus, hymen, and lower third of the vagina (Fig. 18–1). An alternative, equally effective technique is to hold the labia majora gently between your thumbs and forefingers and gently draw them forward (Figs. 18–2 and 18–3).

FIGURE 18–1 Lateral retraction of the labia majora while a prepubertal girl lies in a frog-legged position.
Examination of external genitalia
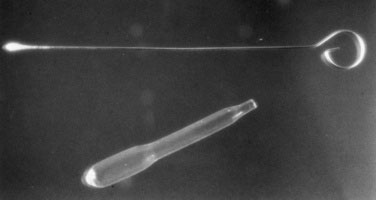
Variations in normal hymenal configuration have been well described (Figs. 18-4 to 18-6). Fimbriated hymens are characterized by redundant folds of hymenal tissue with scalloped rims that circumscribe the vaginal introitus. Annular or circumferential hymens are smooth, uniform skirts of hymenal tissue that completely surround the vaginal introitus. Posterior rim or crescentic hymens appear as smooth folds of tissue arranged from 2 o’clock through 11 o’clock around the introitus, with minimal or no hymenal tissue present inferiorly under the urethra.

FIGURE 18–4 Posterior rim hymen.
(From Pokorny S: Physical examination of the reproductive systems of female children and adolescents. Curr Probl Obstet Gynecol Fertil 8:202, 1990.)
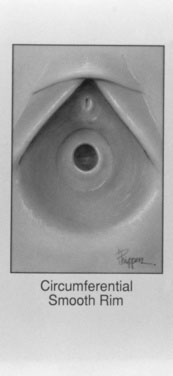
FIGURE 18–5 Circumferential hymen.
(From Pokorny S: Physical examination of the reproductive systems of female children and adolescents. Curr Probl Obstet Gynecol Fertil 8:202, 1990.)
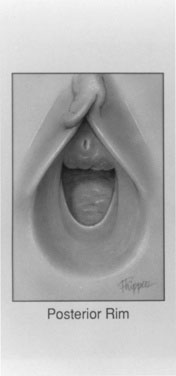
FIGURE 18–6 Fimbriated hymen.
(From Pokorny S: Physical examination of the reproductive systems of female children and adolescents. Curr Probl Obstet Gynecol Fertil 8:202, 1990.)
The appearance of the labia and perihymenal tissues may suggest that the child has been exposed to endogenous (or possibly exogenous) estrogen. The labia and perihymenal tissues of an unestrogenized prepubertal girl are poorly developed and appear red. Labial agglutination (Fig. 18–7) and chronic skin changes, such as increased pigmentation, may suggest a chronic inflammatory process. Document the presence of a purulent discharge, smegma, or leukorrhea. A thicker, lesser fusion of the posterior aspect of the labia minora may suggest excessive androgen stimulation due to congenital adrenal hyperplasia, especially if the labial fusion is associated with clitoral enlargement. If clitoromegaly is present, measure the clitoris glans in both transverse and longitudinal diameters. Normal values for clitoral size at various ages and stages of sexual development are available in pediatric gynecologic references.
Indications for vaginoscopy
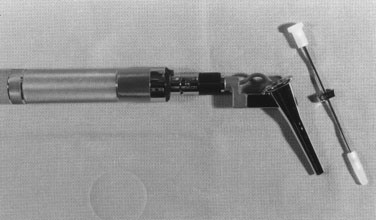
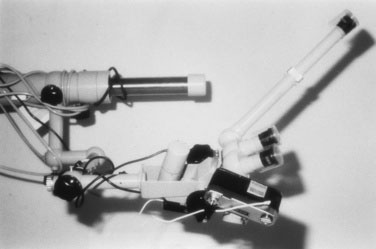
Instrumentation of the vagina is rarely required in the evaluation of prepubertal girls. Indications for vaginoscopy include undiagnosed vaginal bleeding, refractory vaginal discharge, and suspicion of intravaginal foreign body. Before beginning vaginoscopy, show the child all the instruments, and let her touch them (Fig. 18–8). If you intend to obtain cytologic and bacteriologic specimens during vaginoscopy, use only water as a lubricant. Cystoscopes, hysteroscopes, and anoscopes have all been used for vaginoscopy.
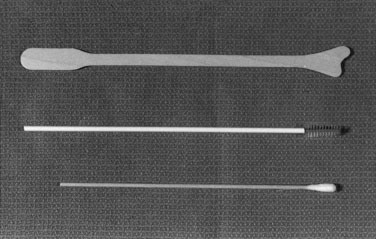
Bacteriologic cultures
It is important to premoisten culture swabs with nonbacteriostatic saline solution or sterile water. Use appropriately sized swabs for culturing, always choosing the smallest swab available (Fig. 18–9). Prior to collecting bacteriologic or viral specimens from the prepubertal child’s vagina, it may be prudent to discuss your needs with your local laboratory or microbiologist because the availability of testing methods will vary among facilities. Diagnostic modalities could range from culture, microscopy, antigen detection tests, nucleic acid detection test, or serology. The sensitivity and specificity of tests will vary according to the specimen type and the organism assayed. So seek an expert opinion first to ensure that you do the most appropriate test because children do not like vaginal sampling.
Obtaining the History
A complete gynecologic history can indicate whether gynecologic disease is present. Document the age of onset and progress of pubertal change (thelarche, adrenarche; see Chapter 16). The mother’s age at menarche is often a good predictor of when her daughter will experience her first menstrual period. Menarche commonly occurs 2 years after thelarche, when breast development reaches Tanner stage 4.
Menses can be characterized in terms of duration of flow, amount of flow, and interval between menses (Fig. 18–10). The normal duration of flow varies from 3 to 7 days. Persistence of menses for longer than 10 days warrants evaluation. When asking about the cycle interval, make sure that the days of menstrual flow are included in the estimate. Day 1 of the menstrual cycle is the first day of the menstrual flow. A range of 25 to 35 days should be accepted as falling within the range of normal; shorter or longer intervals may require evaluation and treatment. Cycles can remain anovulatory for 2 to 4 years after menarche. Therefore, early cycle irregularity may reflect immaturity of the hypothalamic-pituitary-ovarian axis rather than gynecologic disease.
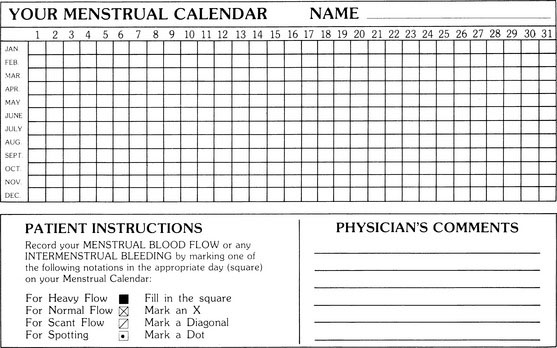
FIGURE 18–10 The menstrual calendar is a useful tool for prospectively recording menses.
(Courtesy of Dr. JEH Spence, Ottawa Civic Hospital, Ottawa, Ontario, Canada.)
Approach to the Pelvic Examination
Always precede a pelvic examination with a general physical examination. This more familiar examination gives your patient time to become comfortable with you and helps relieve some anxiety. Appraise and stage the secondary sexual characteristics and look for evidence of an underlying endocrinopathy. Breast and pubic hair development can be staged according to the Tanner classification (see Chapter 3). Note the presence of axillary hair or of adult sweat odor. Thyroid gland enlargement, galactorrhea, and signs of androgen excess, such as acne, oiliness of the skin, and hirsutism, are all important findings. In the course of the general physical examination, you can give the patient much useful information about the changes that she may be noticing in her body.
Various specula are available to facilitate the examination (Fig. 18–11). The Pederson and Huffman specula are best in pediatric practice because they are much narrower than the Graves speculum, a more appropriate instrument for the examination of multiparous women. Before performing a speculum examination, show the patient the instrument and explain how you will use it. It is easiest to examine adolescent girls when they are placed in the lithotomy position and properly positioned at the end of the examination table. Take the time to encourage the patient to breathe quietly and deeply during the examination and to relax the abdomen and buttocks. The patient should allow her knees to fall loosely open, effecting a further relaxation of the perineal muscles. Warm the speculum under warm (not hot) water; use only water for lubrication to facilitate insertion of the speculum into the vagina. Before inserting the speculum, gently retract the labia laterally with a gloved hand, bringing the hymenal opening into view and preventing inadvertent pinching of the labia when you insert the speculum.
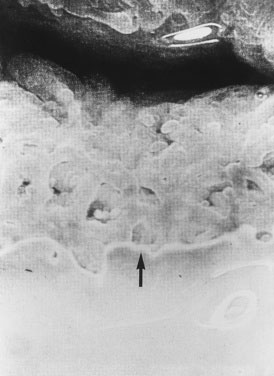
As you insert the speculum, exert gentle pressure posteriorly, because any anterior pressure compresses the sensitive urethra. Next, open the blades of the speculum to bring the cervix into view. Gently swab away the mucus covering the exocervix, and inspect the cervix for any plaques, areas of whiteness, ulcers, or polyps. Nabothian cysts are not abnormal findings (Fig. 18–12). Note the transitional zone at the junction of the columnar and squamous epithelia (Fig. 18–13). It is the transitional zone that must be sampled when you obtain a Pap smear. In adolescents, it is not uncommon to see red-looking columnar epithelium on the exocervix. Do not mistake this finding as an indication of cervicitis.

FIGURE 18–12 Cervix visualized with the aid of a speculum. The arrow points to a benign nabothian cyst.
Always obtain specimens in the following sequence:
Adolescent Contraception
It is useful, when discussing various contraceptive methods, to have both concise information pamphlets and samples of the methods available for scrutiny—oral contraceptive pills (OCPs), intrauterine contraceptive devices, spermicidal creams, condoms, sponges, and diaphragms (Fig. 18–16).
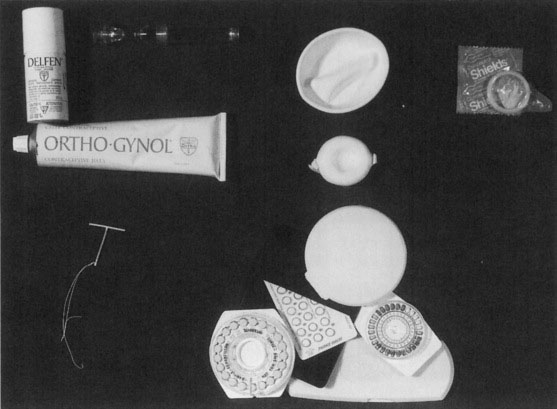
FIGURE 18–16 Counseling about contraceptive choices is facilitated by a complete kit of available devices.
Canadian Consensus Guideline on Continuous and Extended Hormonal Contraception. J Obstet Gynaecol Can. 2007;29:S1-S32.
Canadian Contraception Consensus (3 parts). J Obstet Gynaecol Can. 2004;26(3,4):347-387. 389–436
Canadian Contraception Consensus—Update on Depot Medroxypro gesterone Acetate (DMPA). J Obstet Gynaecol Can. 2006;28:305-313.
Canadian Guidelines on Sexually Transmitted Infections. Public Health Agency of Canada, January 2008.
Delisi K., Gold M. The initial adolescent preventive care visit. Clin Obstet Gynecol. 2008;51:190-204.
Lara-Torre E. The physical examination in pediatric and adolescent patients. Clin Obstet Gynecol. 2008;51:205-213.
Muram D., Simmons K. Pattern recognition in pediatric and adolescent gynecology. J Pediatr Adolesc Gynecol. 2008;21:103-108. (Excellent illustrations.)
Pokorny S., Kozinetz C. Configuration and other anatomic details of the prepubertal hymen. Adolesc Pediatr Gynecol. 1988;1:97-103. (Excellent illustrations.)
Racz J., Srikanthan A., Hahn P., et al. Gender preference for a female physician diminishes as women have increased experience with intimate examinations. J Obstet Gynaecol Can. 2008;30:910-917.