Gynecologic and Obstetric Emergencies
Patterns of Menstrual Bleeding
1. Normal cycle: every 28 days ± 5 days with a duration of 3 to 6 days
2. Normal menstrual flow: 80 mL or three to five pads or tampons per day with a duration of 3 to 5 days
3. Menorrhagia: extended duration
4. Metrorrhagia: continuous duration or with no identifiable pattern
5. Menometrorrhagia: increased quantity and duration
6. Hypermenorrhea: increased quantity
7. Intermenstrual spotting: small amounts of vaginal bleeding that may occur before or after menstruation or midcycle
Vaginal Bleeding Associated with Pregnancy
History
1. Any history of prior ectopic pregnancy, salpingitis, pelvic inflammatory disease, tubal surgery, or use of fertility agents or intrauterine device (IUD) should increase clinical suspicion.
2. Prior bilateral tubal ligation does not exclude the diagnosis.
3. History is usually suggestive of early pregnancy and includes nausea, amenorrhea, and breast tenderness.
4. A prior seemingly normal or abnormal menstrual period is also possible.
Signs and Symptoms
1. An ectopic pregnancy may rupture as early as 5 weeks’ gestation but most commonly ruptures after 7 weeks’ gestation.
2. Ectopic rupture is generally preceded by abnormal vaginal bleeding and unilateral lower abdominal pain.
3. A triad exists of vaginal bleeding, adnexal mass, and lower abdominal pain that is usually unilateral and may radiate to the shoulder.
4. Cervical motion tenderness may be present on pelvic examination.
5. Dizziness, syncope, and unstable vital signs may be present if blood loss is substantial.
6. Rebound tenderness and rigidity are signs of rupture.
7. Any patient with positive pregnancy test results and lower abdominal pain, usually unilateral, should be assumed to have an ectopic pregnancy until proven otherwise.
a. This test is currently sensitive enough to detect levels of urinary β-human chorionic gonadotropin (β-hCG) as low as 20 milliunits/mL from the third to fourth week after the first day of the last menstrual period.
b. This test should be included in remote expedition medical supplies. To ensure adequate performance of the test, use a test with an internal reference.
Spontaneous Abortion
Early pregnancy loss before 20 weeks’ gestation
Signs and Symptoms
1. History suggestive of early pregnancy, including late or missed period and breast tenderness
2. Positive urine pregnancy test results with above signs and symptoms
3. Spontaneous abortion presents as abnormal vaginal bleeding, followed by uterine cramping.
4. Bleeding can vary from dark red spotting to bright red clots.
Treatment
1. Unless a pretrip ultrasound examination has verified an intrauterine pregnancy, immediately evacuate the patient to rule out ectopic pregnancy.
2. Keep the patient at “bed rest” if possible.
3. Direct all field treatment to volume replacement.
4. Evacuation of uterus to prevent further hemorrhage or infection will be necessary once transported to medical facility.
5. Treatment of septic abortion will involve broad-spectrum intravenous antibiotics (see Appendix H).
6. Treat for shock until evacuated (see Chapter 13).
7. Under wilderness conditions, control of significant maternal hemorrhage accompanying miscarriage may be difficult. Once the uterus is empty, uterine involution, spontaneous or aided by uterine massage, is usually sufficient to impede bleeding from the implantation site. In the absence of the ability to perform curettage, treatment with methylergonovine, 0.2 mg PO or IM, can enhance uterine contractions, accelerate expulsion of POC, and promote uterine involution to maintain hemostasis while plans are being made for evacuation of the patient. Methylergonovine should not be used in persons with hypertensive disorders or vascular disease unless the benefits outweigh the risks of generalized vasoconstriction. As an alternative, carboprost tromethamine 250 mcg IM, or misoprostol 100 mcg PO or vaginally, can be administered to stop uterine bleeding with less risk for cardiovascular compromise.
Placental Abruption
1. Rupture of the placenta from the wall of the uterus
2. Separation partial to complete
3. History of painful bleeding in late pregnancy or after trauma
Bleeding Not Associated With Pregnancy
Abnormal Uterine Bleeding in a Nonpregnant Woman
1. Includes bleeding between normal menstrual cycles, change in normal pattern of menstrual cycle, increased or decreased amount of menstrual bleeding
2. Consider other systemic or structural processes:
a. Complications of pregnancy: threatened, incomplete, or spontaneous abortion; ectopic or molar pregnancy
b. Infectious: vaginitis, cervicitis, pelvic inflammatory disease (PID)
d. Medications: aspirin, warfarin, oral contraceptives, tricyclic antidepressants, and major tranquilizers
e. Systemic illness: hepatic, thyroid, and adrenal dysfunction
f. Polycystic ovary syndrome and other endocrinopathies
g. Anatomic lesions: fibroids, polyps, ovarian cysts, endometriosis, endometrial hyperplasia, neoplasm
k. Common in perimenopausal women
l. Common in adolescence secondary to immaturity of the hypothalamic-pituitary-ovarian axis
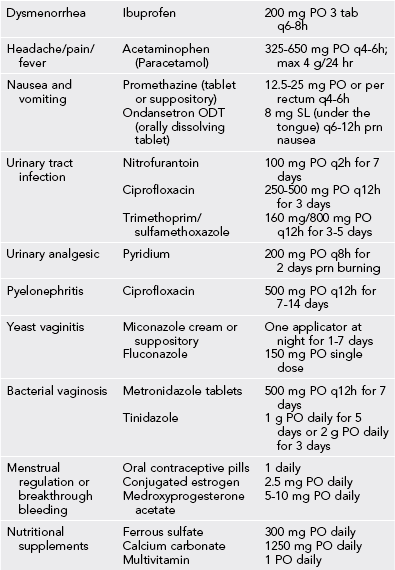
Treatment
1. Perform a urine pregnancy test to rule out pregnancy.
2. In the wilderness, modern, low-dose oral contraceptive pills can be safely used whether the bleeding is caused by estrogen or progestin deficiency or excess.
3. High doses of oral contraceptive pills of the combination monophasic type, such as Lo/Ovral (norgestrel, 0.3 mg, and ethinyl estradiol, 30 mcg), are usually effective.
4. The usual dose for this purpose is three pills per day for 7 days (i.e., one complete pack over a single-week course).
5. Other options include conjugated estrogen or medroxyprogesterone acetate (Table 31-1).
6. Bleeding is typically controlled within 12 to 36 hours.
7. Side effects such as nausea, headache, fluid retention, and depression sometimes occur.
8. After completion of the oral contraceptive pills (i.e., after 7 days), expect significant withdrawal bleeding.
9. A nonsteroidal antiinflammatory agent may be started for pain management.
10. If abdominal or pelvic pain develops or if heavy bleeding persists, arrange for immediate evacuation of the patient. It is highly unusual for the bleeding to progress to massive hemorrhage.
11. Note that any patient with DUB in the field should seek definitive follow-up as soon as is practical.
Vaginal Discharge
Normal vaginal discharge is usually odorless, nonirritating, and white to transparent.
Bacterial Vaginosis
Treatment
1. Metronidazole 2 g PO once. Single-dose oral treatment is practical in the wilderness setting.
2. Metronidazole 500 mg PO q12h or q8h for 5 to 7 days is more effective.
3. Metronidazole 250 mg PO q8h for 7 days in second and third trimester of pregnancy. Avoid in the first trimester of pregnancy.
4. Consider clindamycin 300 to 600 mg PO q12h for 7 days as an alternative. Clindamycin may also be administered as 2% vaginal gel once daily for 7 days.
Candida Vulvovaginitis
Candida albicans is the most common pathogen, responsible for 80% to 90% cases.
Treatment
1. Fluconazole (Diflucan) 150 mg single oral dose
2. Alternatives: azole derivatives (clotrimazole, miconazole, butoconazole, tioconazole, or terconazole) available as intravaginal creams, tablets, and suppositories; treatment of at least 3 days has been found to have lower immediate recurrence rates (e.g., clotrimazole, 200 mg intravaginally for 3 days or 100 mg for 7 days)
3. Prophylactic suppressive therapy with clotrimazole 500-mg vaginal tablet weekly or fluconazole 100-mg oral tablet weekly
Trichomonas Vaginitis
This is a sexually transmitted disease caused by Trichomonas vaginalis.
Treatment
1. Metronidazole 2 g as a single oral dose or 500 mg q12h for 7 days. Alternatively, tinidazole 2 g as a single oral dose may also be used. Avoid in the first trimester of pregnancy. Metronidazole 0.75% vaginal gel is not appropriate for treatment.
2. Take with plenty of water and avoid alcohol to minimize gastrointestinal side effects.
Pain: Vulvar/Vaginal
Vulvovaginal Abscess and Cellulitis/Bartholin’s Abscess
Treatment
1. Perform incision and drainage if adequate equipment is available.
2. Make the incision over the medial aspect of the mucosa, at the point of maximal fluctuance.
3. Insert a hemostat through the mucosal incision, and spread the tips into the deeper tissue. Ensure that there is entrance into a true cavity.
4. Irrigate with a syringe-and-catheter technique.
5. Apply gauze packing to maintain drainage for 24 to 48 hours.
6. With evidence of cellulitis, administer cephalexin (see Appendix H) until resolved.
7. If the availability of water and conditions permit, arrange for a sitz bath daily.
8. Change the dressing once to twice daily until the wound is well healed without drainage.
9. Recurrence is common after simple incision and drainage, warranting follow-up treatment on return.
Pain: Pelvic/Lower Abdominal
Treatment
1. Differential diagnosis includes appendicitis, septic abortion, pyelonephritis, as well as other entities in this category.
2. Pregnancy test to rule out ectopic pregnancy
3. If available, test for gonorrhea and chlamydia infection.
4. For severe symptoms treat with ceftriaxone 250 mg IM single dose, followed by doxycycline 100 mg PO q12h for 10 to 14 days.
5. Alternative treatment: ofloxacin 400 mg PO q12h with metronidazole 500 mg PO q12h for 14 days
6. Evacuate immediately if there are positive pregnancy test results, adnexal mass, peritoneal signs, toxic appearance, presence of an IUD, or fever greater than 102.2° F (39° C).
Mittelschmerz
Pain associated with ovulation
Signs and Symptoms
1. Sudden onset of right lower quadrant (RLQ) or left lower quadrant (LLQ) abdominal pain occurring midcycle (between days 12 and 16) in a reproductive woman at the time of ovulation
2. The presentation is not associated with marked gastrointestinal, genitourinary, or systemic symptoms.
3. Symptoms usually last less than 8 hours.
4. Not associated with vaginal bleeding or spotting
5. Associated with mild referred pain and rebound tenderness
6. Pelvic examination to rule out PID (often less adnexal tenderness than with PID)
Ovarian Torsion
Signs and Symptoms
1. RLQ or LLQ pain that is sharp, localized, and sudden in onset
2. Pain is usually intermittent and may be accompanied by low-grade fever, nausea, and vomiting.
3. Unilateral adnexal tenderness, which may or may not be accompanied by a palpable mass
4. Consider appendicitis if pain is right sided.
5. Negative or positive pregnancy test results, depending on the cause of the torsion
Ovarian Cyst
Emergency Wilderness Childbirth
1. To the extent possible, a clean, comfortable, and quiet site should be prepared for the delivery. Clean and sterile supplies and medications, if available, should be collected and inventoried. Otherwise, clean towels, clothing, bedding, soap, and water should be made readily accessible.
2. Any pregnancy with a fundal height at or above the umbilicus should be considered potentially viable.
3. If in the early stages of labor with rupture of membranes but no strong, regular contractions, oral fluids and small mealsshould be encouraged. Only small sips of clear fluids are recommended when strong contractions begin.
4. Fetal position should be assessed by palpation of the pregnancy and location of the fetal head and buttock to anticipate a nonvertex delivery.
5. Digital examination of the cervix should be avoided in the wilderness unless sterility can be ensured, because of risk for infection.
6. By necessity and practicality, delivery in the wilderness is a laissez-faire approach, and excessive interventions (e.g., repeated cervical examination, artificial rupture of membranes, augmentation of uterine contractions, manual cervical dilation) are neither warranted nor appropriate because they increase fetal and maternal risk.
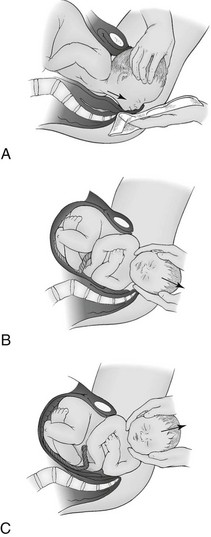
Vertex Delivery (Fig. 31-1)
1. When the perineum begins to distend, instruct the woman to bear down with each contraction.
2. Support the perineum between the rectum and introitus, using your index finger and thumb.
3. Control the delivery of the head, keeping it in flexion until it clears the symphysis pubis.
4. Once the head is cleared, ask the woman to stop pushing.
5. Exert steady inward and upward pressure at the perineum, against the chin with countertraction on the occiput. Allow for controlled extension of the head.
6. Once delivered, the head will automatically rotate laterally to align itself with the shoulders.
7. Suction the nose and mouth, using gauze or a cloth if a suction bulb is not available.
8. Palpate the fetal neck for a nuchal cord. If present, undo the nuchal cord by slipping it over the fetal head. The cord may also be clamped twice and cut if a nuchal cord cannot be reduced.
9. Instruct the woman to resume bearing down steadily, and cup both sides of the fetal head.
10. Apply gentle downward pressure on the head, until the anterior shoulder is visible.
11. Apply upward traction, until the posterior shoulder is delivered. The rest of the body will quickly follow.
12. Hold the baby below the perineum. Towel dry, and suction the oropharynx.
13. Clamp or tie the umbilical cord twice, and sever between the clamps or ties.
14. After a wilderness delivery, administer a broad-spectrum antibiotic to the mother for 24 to 48 hours (see Appendix H).
15. If the mother is Rh negative and the baby’s blood type is Rh positive or unknown, administer Rh immune globulin, 300 mcg IM, to the mother.
Breech Delivery (Fig. 31-2)
1. Breech babies come in many forms: frank breech (hips flexed, knees extended, buttocks presenting); complete breech (both hips and both knees flexed, buttocks and feet presenting); incomplete breech (one hip flexed, one hip partially extended, both knees flexed, buttocks and feet presenting); and footling breech (hips and knees extended, feet presenting).
2. The approach in a wilderness setting demands patience. No effort should be made to deliver a breech baby until the presenting part is visible at the introitus and the cervix is completely dilated.
3. Membranes should not be artificially ruptured in breech presentations.
4. When the cervix is completely dilated, the woman is instructed to push.
5. Regardless of the type of breech presentation, the safest course is to allow the body to be extruded to at least the level of the umbilicus by maternal efforts alone.
6. A baby in a frank or complete breech lie should have the posterior leg delivered by gently grasping the thigh and flexing the leg at the knee as it is rotated medially and toward the introitus.
7. The baby should then be rotated to the sacrum anterior position, then another 45 degrees in the same direction to facilitate delivery of the other leg using the technique described for the first.
8. The legs and buttocks can be wrapped in a clean towel to provide a firmer grip and decrease trauma to the baby.
9. The delivery from this point is the same as for footling breech presentations. The upper legs should be grasped on each side with the index fingers crossing the infant’s pelvic girdle and both thumbs positioned just above the crease of the buttocks.
10. Using gentle side-to-side rotational motion over an arc of 90 degrees outward and downward, traction should be applied while the mother pushes, until the upper portion of a scapula is visible at the introitus.
11. With the baby’s body rotated 45 degrees toward the opposite side, the arm is delivered by flexion and medial rotation across the chest.
12. The baby is rotated to the opposite side in the same position, and the other arm is then delivered.
13. If assistants are present, the woman should be helped into the McRoberts position, with hyperflexion at the hips to maximize the space between the symphysis and the sacrum.
14. Maintaining the baby in the same plane as the vagina, the birth attendant reaches palm up between the baby’s legs and into the vagina, supporting the baby’s entire body on the forearm while placing the second and fourth fingers over the infant’s maxillae and placing the middle finger into the mouth or on the chin.
15. The other hand is positioned over the infant’s upper back so that the fingers are overlying each shoulder.
16. If there is sufficient room, the middle fingers can be applied to the fetal occiput. Then with the woman pushing, the baby’s head is flexed downward, completing the delivery.
17. Firm suprapubic pressure can help to maintain the head in flexion. During this final stage the baby’s body should not be elevated more than 45 degrees above the plane of the vagina to avoid hyperextension of the head.
18. If the fetal head cannot be delivered because the cervix is incompletely dilated, the cervix can be cut at the 2 and 10 o’clock positions (Dührssen incisions) to provide sufficient room to complete the delivery.
19. Once delivered, if the baby breathes and cries spontaneously or with minimal stimulation, cutting the umbilical cord can be delayed while the baby is dried. This allows some of the blood retained in the placenta from umbilical vein compression (common with breech deliveries) to return to the baby.
20. On the contrary, if the baby is clearly depressed, the umbilical cord should be immediately clamped and cut and neonatal resuscitation begun.
Delivery of the Placenta
1. Place the heel of your hand just above the symphysis to hold the uterus in place.
2. Apply fundal pressure with the tips of the same hand.
3. Simultaneously apply steady downward traction of the umbilical cord with the other hand. Do not use excessive traction.
4. A gush of blood and lengthening of the cord signify separation.
5. Once separated, rotate the placenta several times as it passes through the introitus.
6. Massage the uterus to promote contraction.
7. Assess for lacerations to the perineum and repair accordingly with polyglactin 910 (Vicryl) sutures.
8. Apply pressure to control small amounts of bleeding.
9. Place ice packs to the perineum for the first 12 to 24 hours if available.
Breastfeeding
1. During the first 24 hours after delivery, feed every 2 to 3 hours, 5 minutes on each breast, alternating first breast.
2. As milk production is established over the next 2 to 3 days, advance the feeding schedule to 10- to 15-minute periods on each breast 8 to 12 times per day.
3. Have the mother drink at least 2 L of fluids each day, increase caloric intake, and consume foods rich in calcium.
4. For engorgement, apply cool compresses after nursing, wear a nursing bra, and use acetaminophen for pain.
5. For mastitis, administer a course of antibiotics (e.g., dicloxacillin or cephalexin) for 10 to 14 days. In an appropriate circumstance, suspect methicillin-resistant Staphylococcus aureus.
Emergency Contraception
1. Two doses of levonorgestrel (Plan B) taken at one time within 120 hours of unprotected intercourse
2. Two doses of estrogen-progestin combination oral contraceptive pills (for this purpose, each dose: Ovrette 20 tablets; Ovral 2 white tablets; Lo/Ovral 4 white tablets; Nordette 4 orange tablets; Levlen 4 orange tablets; Levora 4 white tablets; Tri-Levlen 4 yellow tablets; Triphasil 4 yellow tablets; Trivora 4 pink tablets; Alesse 5 pink tablets) taken 12 hours apart within 72 hours of unprotected intercourse
Immunizations during Pregnancy
Table 31-2
CDC Recommendations for Vaccination During Pregnancy
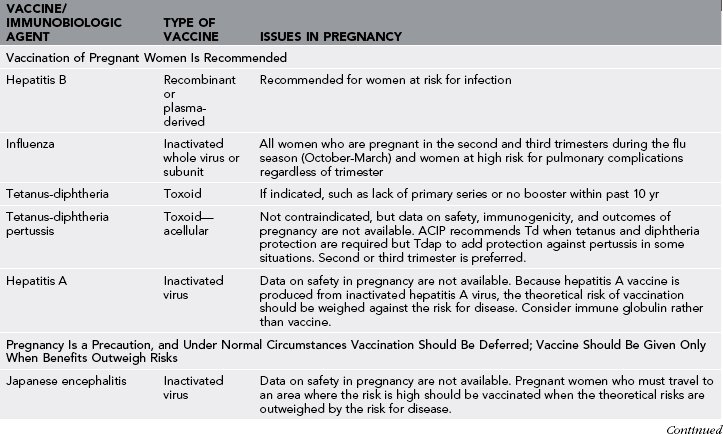
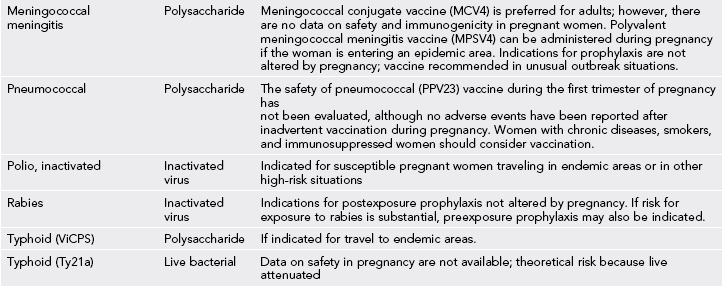
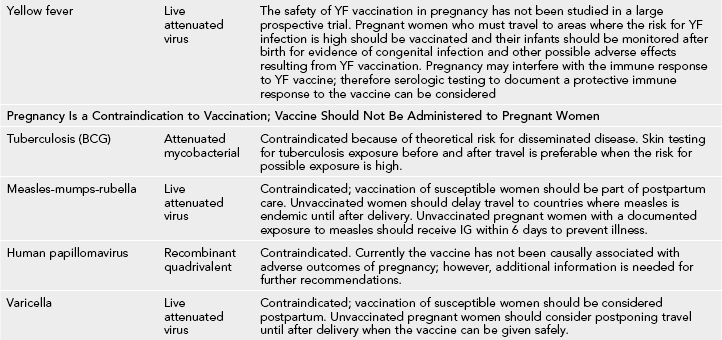
Note: See 2012 CDC update: Do not give YF vaccine to pregnant or breastfeeding women.
Modified from CDC health information for international travel 2012; pp 470-474. http://www.cdc.gov/vaccines/pubs/preg-guide.htm.
Medications during Pregnancy
The Food and Drug Administration has developed a set of guidelines to categorize drugs with regard to developmental toxicity and adverse fetal outcome (Box 31-1). Medication use during pregnancy and lactation is guided by these recommendations (Table 31-3).
Table 31-3
Medication Use During Pregnancy and Lactation
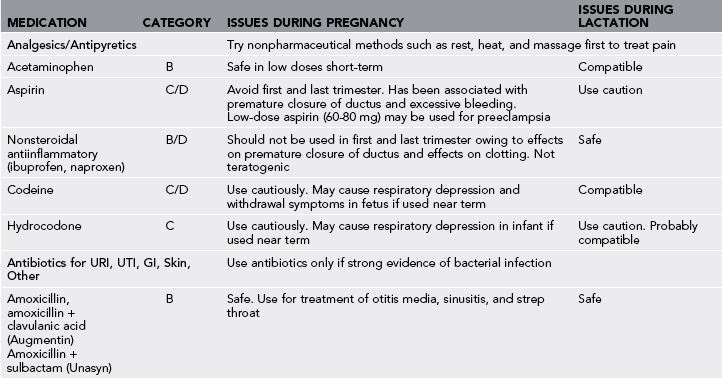
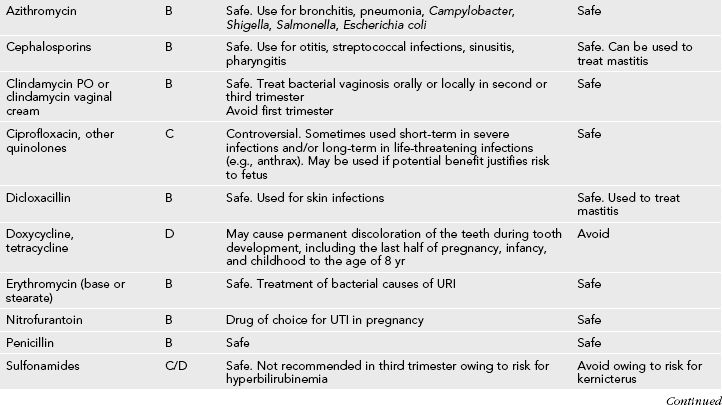
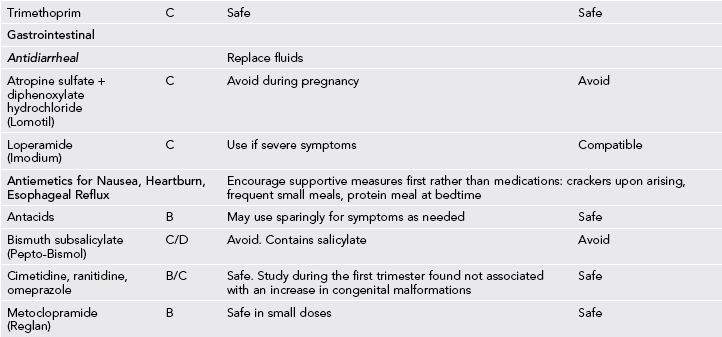
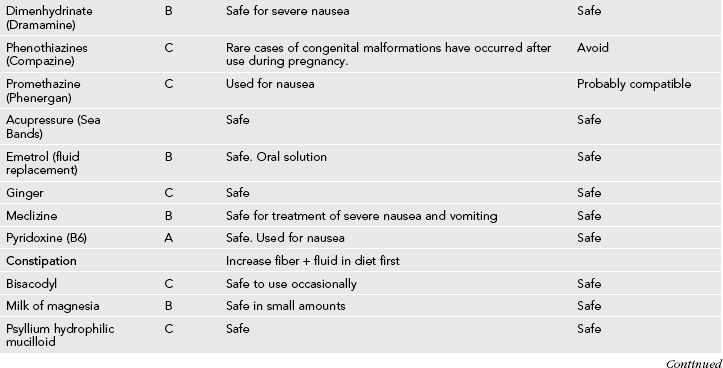
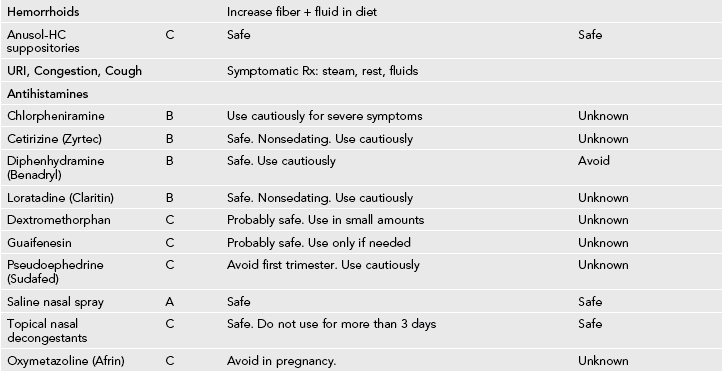
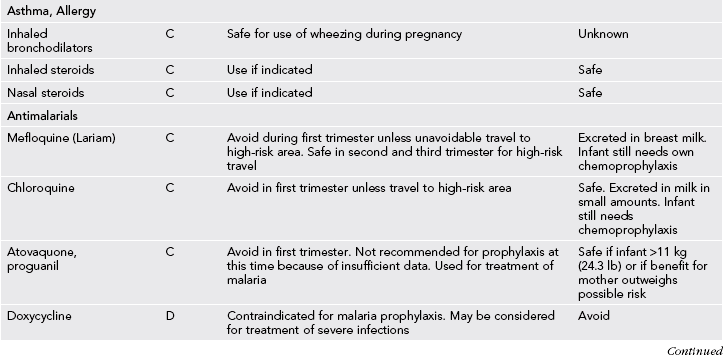
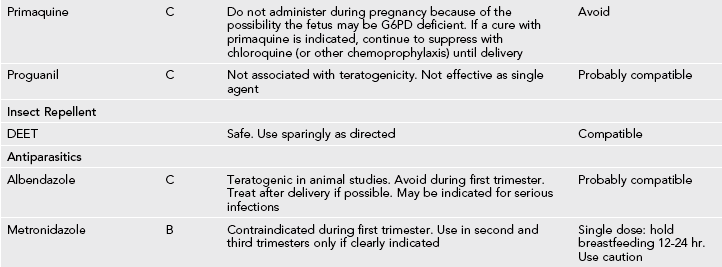
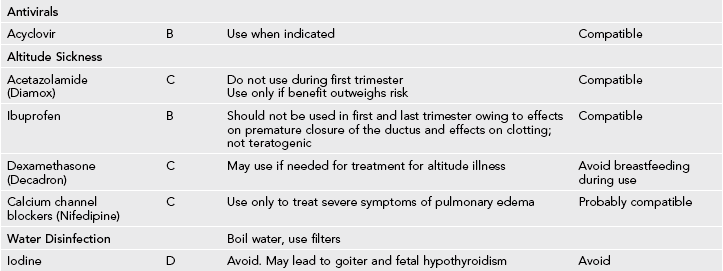
GI, Gastrointestinal; URI, upper respiratory infection; UTI, urinary tract infection.
Data from Briggs G, Freeman R, Yaffe S: Drugs in pregnancy and lactation, Baltimore, 2005, Lippincott Williams & Wilkins; Micromedex Online; American Academy of Pediatrics, 2005; and Lexi-Comp Online UptoDate.