Chapter 41 Gynaecological problems in childhood and adolescence
INTERSEX
Congenital adrenal hyperplasia (CAH)
This condition affects one in 10 000 neonates and is due to a group of enzyme defects which prevent the synthesis of cortisone from progesterone. The lack of circulating cortisone permits the hypothalamus–pituitary to release quantities of corticotrophins, which stimulate the adrenal gland to secrete androgens, with resulting virilization of the external genitals (Fig. 41.1).
Other causes of intersex
Gonadal dysgenesis
There are two varieties of this condition, pure gonadal dysgenesis and Turner’s syndrome.
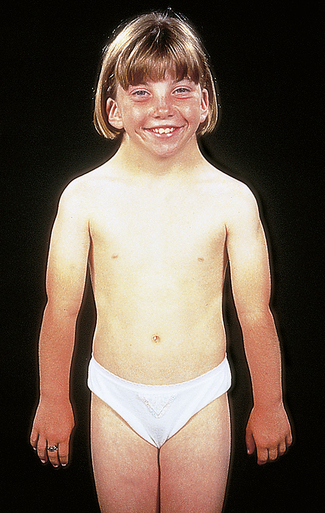
Gonadal dysgenesis/Turner’s syndrome
In adolescence the classic features are short stature and arrested or delayed puberty (Fig. 41.2). Only 9% with the 45, X karyotype have a complete spontaneous puberty compared with 40% of those with mosaicism. Spontaneous pregnancy is rare (2%); more likely in the mosaic form, but has been reported in the 45, X variant. The standard management is to administer growth hormone and some women can achieve normal adult height. As most have arrested pubertal development, hormone replacement therapy is carefully introduced to complete feminization over 2–3 years. These women need careful supportive counselling, especially to deal with the sexuality and infertility issues.
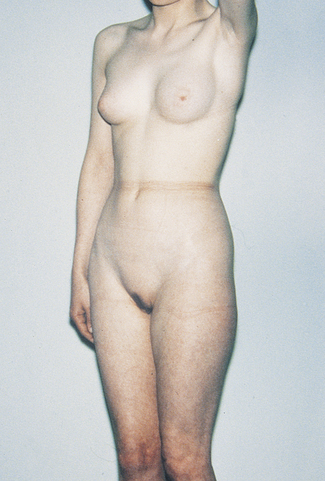
Testicular feminization
Physically, the person is female with female external characteristics, including good breast development (Fig. 41.3) and has been reared as a girl. She and her parents are concerned when she fails to menstruate. Examination shows that she has a short vagina, which ends blindly. Her karyotype is 46, XY, as she is genetically male. The gonads are in the abdominal cavity or in a hernial sac. They synthesize testosterone, but the body tissues lack α-reductase enzyme to convert it to di-hydroxytestosterone, and receptor cells in genital tract tissues and skin may be missing. As the testes may become malignant they should be removed and hormonal replacement treatment given.
VULVOVAGINITIS IN PREPUBERTAL CHILDREN
Vulvovaginitis may occur at any age. The child is brought by the mother complaining of an inflamed, tender vulva and, perhaps, a vaginal discharge. The causes are listed in Table 41.1. The vulval area should be inspected and an anal swab taken for pin and thread worms. A swab should be taken from the vagina. If an intravaginal foreign body is suspected and cannot easily be detected the child should be referred to a gynaecologist who deals with children, for examination with a vaginoscope.
| Percentage | ||
|---|---|---|
| 1. Non-specific | 60 | |
| 2. Specific | ||
| a. Bacterial E. coli N. gonorrhoeae Other |
 |
20 |
| b. Fungal (Candida) | 10 | |
| c. Protozoal (trichomonad) | 5 | |
| d. Foreign body | 5 | |
| e. Helminthic/viral | 1 | |
PHYSICAL CHANGES OF PUBERTY AND EARLY ADOLESCENCE
The endocrinological changes that occur before and after puberty are detailed in Chapter 2. These changes manifest in physical changes (Table 41.2). If they do not parallel, fairly closely, the changes in their peers, some girls become anxious and seek reassurance. Others may develop an eating disorder.
Table 41.2 Time of appearance of sexual characteristics in girls
| AGE | CHARACTERISTICS |
|---|---|
| 9–10 |
By the age of 17 over 99% of adolescents will have reached menarche. Delay after this age may be constitutional or have a recent cause (Table 41.3). Investigations include:
Table 41.3 Primary amenorrhoea
| PERCENTAGE OF CASES | |
|---|---|
| Gonadal dysgenesis (incl. Turner’s syndrome) | 45 |
| Congenital absence of uterus or vagina | 15 |
| Low body weight (incl. anorexia nervosa and severe malnutrition) | 10 |
| Congenital adrenal virilism | 5 |
| Testicular feminization | 5 |
| Other (incl. hypothyroidism in 4%; systemic disease 4%) | 15 |
| Hypogonadotrophic hypogonadism (usually constitutional delayed menarche) | 5 |
The history and examination may indicate special examinations, for example measurement of FSH; imaging of the skull or the pelvic organs; nuclear sex chromatin; laparoscopy. Treatment is discussed in Chapter 28.
MENSTRUAL DISTURBANCES IN ADOLESCENCE
Menstrual disturbances are discussed in Chapter 28. As mentioned, in the first 2 years after the menarche some young women experience oligomenorrhoea, whereas in others menstruation occurs at longer or shorter intervals. Unless the disorder persists, treatment consists of reassuring the young woman that it will settle.
Dysmenorrhoea affects many adolescent women and is considered on page 232.