41. Guillain-Barré Syndrome
Definition
Guillain-Barré syndrome is an acute, ascending motor neuron paralysis that progresses very rapidly. This disease is also called acute inflammatory demyelinating polyradiculoneuropathy (AIDP), acute idiopathic polyneuritis, or acute inflammatory polyneuropathy.
Incidence
The incidence of Guillain-Barré syndrome ranges from 0.5:100,000 to 1.5:100,000. It is reported in all races. This disease has a slightly higher occurrence in males than in females (1.2:1). Risk of the disease increases steadily after age 40 years and peaks at 70 to 80 years.
Etiology
Guillain-Barré syndrome is an autoimmune-mediated malady frequently triggered by environmental factors, which can be pathogenic or stressful exposures. Pathogenic triggers usually precede the onset of symptoms by 1 to 3 weeks. The triggers include Epstein-Barr virus, cytomegalovirus, hepatitis, varicella, Mycoplasma pneumoniae, and Campylobacter jejuni. Endogenous antigens include myelin P-2, ganglioside GQ1b, GM1, and GT1a.
Signs and Symptoms
• Ataxia
• Autonomic instability
• Dysesthesias
• Illness or immunization 2 to 4 weeks before onset of symptoms
• Ophthalmoplegia
• Orthostatic hypotension
• Pain
• Polyneuritis cranialis
• Progressive ascending flaccid paralysis
• Respiratory compromise
• Urinary retention
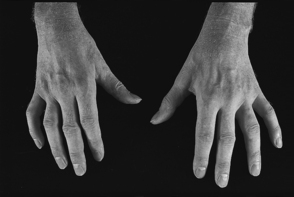 |
| Guillain-Barré Syndrome. Residual hand muscle wasting in Guillain-Barré syndrome. |
Medical Management
Treatment of Guillain-Barré syndrome is primarily focused on immunomodulation and supportive measures. Intravenous immunoglobulin is considered the most effective immuno- modulation therapeutic measure.
Plasmapheresis is also an effective immunomodulation treatment that can significantly shorten the recovery time, but the efficacy is most optimal if initiated within 2 weeks of the appearance of symptoms.
Respiratory muscles are frequently affected by this disease. The patient’s ability to maintain adequate respiratory effort is quickly impaired. Mechanical ventilation is indicated when arterial Pco 2 is greater than 50 mm Hg, alveoarterial O 2 tension gradient is greater than 300 mm Hg at an Fio 2 of 1.0, maximum inspiratory and expiratory pressures are less than 30 cm H 2O, and vital capacity is under 14 mL/kg.
Autonomic dysfunction also frequently occurs with Guillain-Barré syndrome and is characterized by labile blood pressure—vacillation between hypertension and hypotension—sinus tachycardia, diaphoresis, and orthostatic hypotension. Treatment of the hypertension and hypotension may be required.
Complications
• Adult respiratory distress syndrome
• Autonomic instability
• Constipation
• Decubitus ulcers/pressure sores
• Dysesthesias
• Gastritis
• Ileus
• Pneumonia
• Pulmonary embolus
• Respiratory muscle weakness
• Septicemia
Anesthesia Implications
Chief concerns for the anesthetist revolve around the severity of both respiratory and autonomic dysfunction. Anesthetic management for the patient with Guillain-Barré syndrome incorporates the same concerns as for other patients with degenerative motor neuron disorders. Succinylcholine should not be used in the patient with Guillain-Barré syndrome because of the potassium release associated with its administration. The patient may likely exhibit greater sensitivity to nondepolarizing muscle relaxants.
Because of the associated autonomic dysfunction, intraoperative intra-arterial pressure should be monitored continuously. The catheter should be inserted preoperatively because of the large, rapid fluctuations that may occur, particularly during induction.
No particular inhalational anesthetic agent is more or less desirable or effective than another for the patient with Guillain-Barré syndrome. The anesthetist should anticipate potentially prolonged or residual effects from inhalational agents. The possible residual effects may combine with residual effects of nondepolarizing muscle relaxants to necessitate postoperative ventilation.
Use of regional anesthesia is controversial. A few reports have demonstrated no complications or detrimental effects from this anesthesia technique; however, some reports have suggested that a regional anesthetic can cause onset of this disease.







