CHAPTER 2 Gross Anatomy of the Subtalar Joint
The subtalar joint is a complex and functionally important joint of the lower extremity that plays a major role in the movement of inversion and eversion of the foot.1,2 The complex anatomy of the subtalar joint makes arthroscopic and radiographic evaluation difficult. However, advances in small joint arthroscopic techniques and instrumentation have expanded the use of arthroscopy in the subtalar joint. Arthroscopic visualization of the subtalar joint includes the posterior joint, anterior joint, and sinus tarsi. The tarsi sinus is extra-articular, but for practical purposes, it is included in the description of subtalar arthroscopy and the relevant anatomy.
The surgeon must comprehend the gross and arthroscopic anatomy of the subtalar joint to improve surgical performance and recognize abnormal pathology. Because the lateral and posterior anatomic approaches are used for performing subtalar joint arthroscopy,3–6 knowledge of the superficial anatomy in these areas is important.
SUBTALAR JOINT ANATOMY
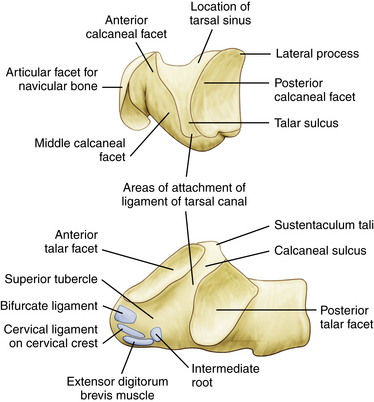
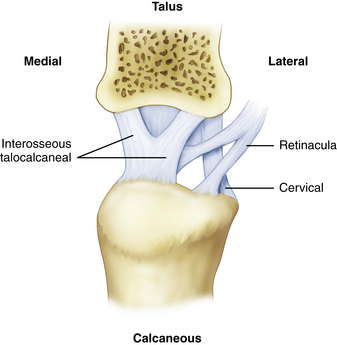
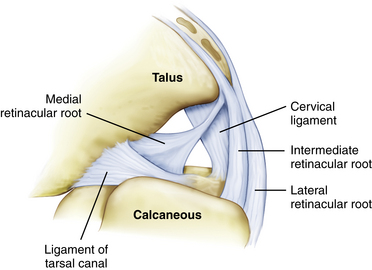
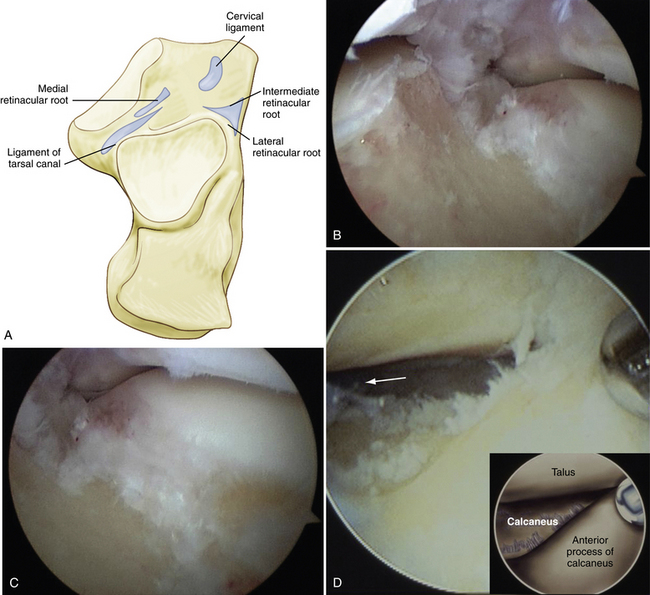
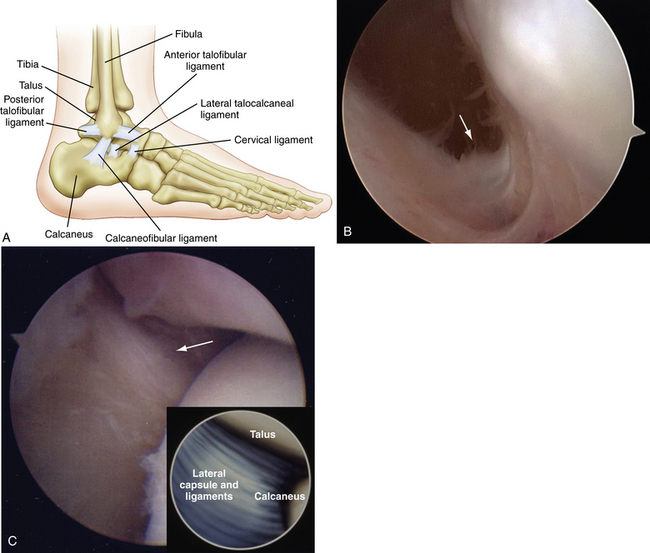
For arthroscopic purposes, the subtalar joint can be divided into anterior (talocalcaneonavicular) and posterior (talocalcaneal) articulations (Fig. 2-1).3–7 The anterior and posterior articulations are separated by the tarsal canal and the lateral opening of this canal, called the sinus tarsi, which is a soft, palpable area approximately 2 cm anterior to the tip of the lateral malleolus. The medial root of the inferior extensor retinaculum, the cervical and talocalcaneal interosseous ligaments, fatty tissue, and blood vessels are found within the sinus tarsi and tarsal canal. The ligaments that support the subtalar joint on the lateral side consist of a superficial, intermediate, and deep layer (Fig. 2-2). The superficial layer consists of the lateral talocalcaneal ligament, the posterior talocalcaneal ligament, the medial talocalcaneal ligament, the lateral root of the inferior extensor retinaculum, and the calcaneofibular ligament. The intermediate layer is formed by the intermediate root of the inferior extensor retinaculum and the cervical ligament. The deep layer consists of the medial root of the inferior extensor retinaculum and the interosseous ligament (Fig. 2-3).8–11
The talocalcaneonavicular joint, or anterior subtalar joint, is composed of the talus, the posterior surface of the tarsal navicular, the anterior surface of the calcaneus, and the plantar calcaneonavicular (spring) ligament. The anterior portion of the subtalar joint includes the anterior and middle articulating facets. Compared with the posterior joint, the anterior subtalar joint is more difficult to examine with the arthroscope because the thick ligaments that fill the sinus tarsi and tarsal canal may block the initial view. The anterior joint normally has no connection to the posterior joint because the thick interosseous ligament fills the tarsal canal and separates the two anatomic areas (Fig. 2-4).
The posterior subtalar joint has a long axis oriented obliquely 40 degrees to the midline of the foot, facing laterally. It is a synovium-lined joint consisting of the convex posterior facet of the calcaneus and the concave posterior facet of the talus. The posterior subtalar joint consists of the posterior calcaneal facet of the undersurface of the talus and the posterior articular surface of the calcaneus. The joint capsule is reinforced on the lateral side by the lateral talocalcaneal ligament and the calcaneofibular ligament. The posterior joint has a posterior capsular pouch with small lateral, medial, and anterior recesses (Fig. 2-5).
ANATOMY OF PORTAL PLACEMENT AND SAFETY
Lateral Approach Anatomy
Arthroscopic evaluation of the subtalar joint has traditionally been performed using a lateral approach. Three portals are recommended for visualization and instrumentation of the subtalar joint using the lateral approach (Fig. 2-6). The anatomic landmarks for lateral portal placement include the lateral malleolus, the anterior process of the calcaneus, the sinus tarsi, and the Achilles tendon. The lateral malleolus and anterior process of the calcaneus are easy to palpate. The sinus tarsi is a palpable depression between the distal tip of the fibula and the anterior process of the calcaneus, although it can be filled with large amounts of adipose tissue. Inversion and eversion of the foot may be helpful in palpating the sinus tarsi.
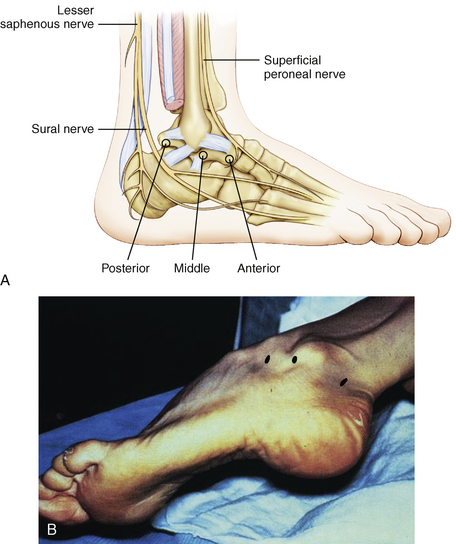
FIGURE 2-6 A, Three standard portals are used to approach the subtalar joint: anterior, middle, and posterior. B, Anatomic landmarks are used for placement of the lateral portals: the distal fibula, the anterior process of the calcaneus, and the sinus tarsi between the fibula and calcaneus. The patient is in the lateral decubitus position.
The point of entry for the anterior portal is usually about 2 cm anterior and 1 cm distal to the tip of the distal fibula, directing the instrument slightly upward and about 40 degrees posteriorly. The location of the portal in cadaveric dissection studies is an average of 28 mm (range, 23 to 35 mm) anterior to the tip of the fibula (Fig. 2-7).7 Structures at risk when placing the portal include the dorsal intermediate cutaneous branch of the superficial peroneal nerve, the dorsal lateral cutaneous branch of the sural nerve, the peroneus tertius tendon, and the small branch of the lesser saphenous vein. The dorsal intermediate cutaneous branch of the superficial peroneal nerve is located an average of 17 mm (range, 0 to 28 mm) anterior to the portal. The dorsal lateral cutaneous branch of the sural nerve (indentified in 8 of 15 specimens) was located an average of 8 mm (range, 2 to 12 mm) inferior to the anterior portal.7 The peroneus tertius tendon was located an average distance of 21 mm (range, 8 to 33 mm) anterior to the portal. A small branch of the lesser saphenous vein consistently coursed along the anterolateral aspect of the foot in the vicinity of the anterior portal. It is located an average of 2 mm (range, 0 to 5 mm) from the anterior portal and was lacerated 20% of cases in one report of portal safety.7 With use of the anterior portal, care must be taken to avoid injury to the dorsal intermediate cutaneous branch of the superficial peroneal nerve as it divides on the dorsum of the foot. A small branch of the lesser saphenous vein is also at risk, although damage to the structure is unlikely to cause significant problems.
The posterior portal is located an average of 25 mm (range, 20 to 28 mm) posterior and 6 mm (range, 0 to 10 mm) proximal to the tip of the fibula.7 Compared with other subtalar portals, the posterior portal used for the lateral approach is more likely to cause nerve or vessel damage. Structures subject to injury with posterior portal placement include the sural nerve, lesser a saphenous vein, peroneal tendons, and the Achilles tendon. Great care must be taken during posterior portal placement to avoid injury, especially to the sural nerve and lesser saphenous vein.
The sural nerve and lesser saphenous vein run parallel to each other along the posterolateral aspect of the ankle, with the nerve coursing posterior to the vein at the level of the ankle joint. In 7 of 10 cases reported by Frey,7 the posterior portal was located posterior to the sural nerve, and in two cases, it was found to be anterior to the nerve. The average distance from the sural nerve to the posterior portal was 4 mm (range, 8 mm posterior to 6 mm anterior). In one case, the sural nerve was transected during portal placement, and in another, a small laceration was made in the lesser saphenous vein. The peroneal tendon sheath was located an average of 11 mm (range, 6 to 16 mm) anterior to the portal, and the Achilles tendon was an average of 15 mm posterior (range, 10 to 20 mm) to the portal. Neither tendon was damaged in the series, but the tendons’ proximity should be considered.
Accessory portals for posterior subtalar arthroscopy have been described in the literature. The accessory anterolateral and posterolateral portals are used as needed for viewing and instrumentation. The accessory anterolateral portal is usually slightly anterior and superior to the standard anterior portal. The accessory posterolateral portal is made behind the peroneal tendons, lateral to the standard posterior portal.12–16
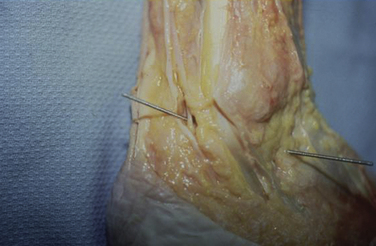
Posterior Approach Anatomy
Posterior subtalar arthroscopy can be performed from a purely posterior approach using posterolateral and posteromedial portals (Fig. 2-8).17,18 This is a two-portal endoscopic approach to the hindfoot, which becomes arthroscopic after it enters the subtalar joint. The posterior approach can be accomplished with the patient in the prone position. The posterior approach has been reported to provide better access to the medial and anterolateral aspects of the posterior subtalar joint,17,18 but the posterolateral and posteromedial portals used to approach the subtalar joint are the same as those used to approach the posterior aspect of the ankle and the hindfoot.
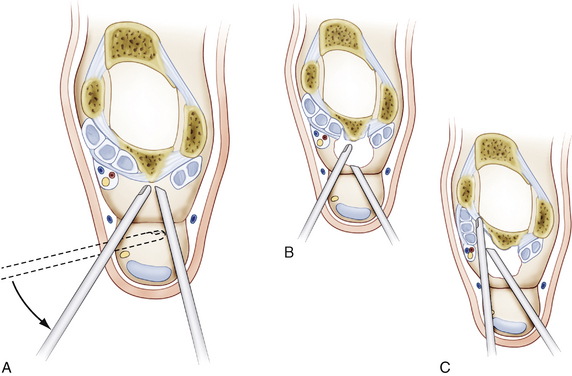
FIGURE 2-8 Posterior subtalar arthroscopy can be performed using posterolateral and posteromedial portals.
The medial aspect of the posterior subtalar joint is tighter than on the lateral side, possibly increasing the risk of iatrogenic cartilage damage. The tibial nerve, the posterior tibial artery, and the medial calcaneal nerve are in proximity and can be at risk when the posteromedial portal is used. Several investigators have studied the relative safety of the posterior portals for hindfoot endoscopy in anatomic specimens.17–20 Mekhail and colleagues determined the average distance between the point of entry of the posteromedial arthroscope and the posterior tibial neurovascular bundle to be 1.0 cm. The closest distance was 8 mm.19 Sitler evaluated the safety of posterior ankle arthroscopy in 13 cadaver specimens.18 Posteromedial and posterolateral portals were established in each specimen, and after performing arthroscopy to determine how much of the talar dome could be visualized, plastic cannulas were placed into the portal locations. Magnetic resonance imaging (MRI) was used to document the distance of the cannulas to neurovascular structures, and these measurements were correlated with the results of anatomic dissections. The average distance between the posteromedial cannula and the tibial nerve was 6.4 mm (range, 0 to 16.2 mm). The distance between the posterior tibial artery and the cannula was on average 9.6 mm (range, 2.4 to 20.1 mm). The average distance between the cannula and the medial calcaneal nerve was 17.1 mm (range, 19 to 31 mm). The location of the posterolateral portal in relation to the tip of the lateral malleolus is an important measurement to determine the proximity of the portal to relevant anatomic structures. It appears that the posterolateral and posteromedial portals used for subtalar arthroscopy are relatively safe, are reproducible, and can be used for the treatment of intra-articular and extra-articular hindfoot pathology.
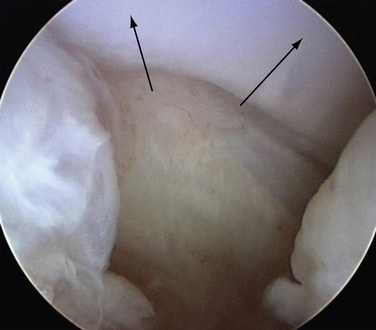
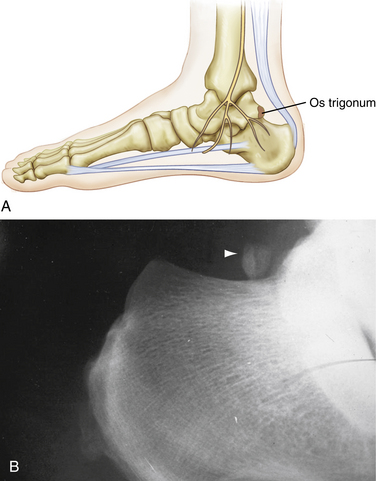
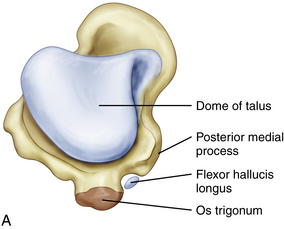
Os Trigonum Gross Anatomy
Because the os trigonum can be approached through the subtalar joint, it is included in the description of relevant gross anatomy (Fig. 2-9).21–23 Terminology regarding the anatomy of the posterior aspect of the talus and the subtalar joint can be confusing. The posterior surface of the talus (“process posterior”) consists of the posterior medial and the posterior lateral processes, also known as tubercles. Between these tubercles glides the flexor hallucis longus tendon in its small sulcus, which is directed obliquely, downward, and inward, angling anteriorly (Fig. 2-10).
None of these terms should be confused with the lateral process of the talus, which is a distinctly different structure located on the midlateral aspect of the talus. It provides an insertion site for the lateral talocalcaneal ligament. The lateral process of the talus is of arthroscopic importance because it is a palpable landmark and can be identified intra-articularly on the medial side of the lateral gutter of the subtalar joint. The lateral talocalcaneal ligament coming off the lateral process makes up a thick portion of the lateral capsule of the subtalar joint (Fig. 2-11).
CONCLUSIONS
Advances in small joint techniques and instrumentation have expanded the use of arthroscopic techniques in the subtalar joint. The surgeon must thoroughly understand the gross and arthroscopic anatomy of the subtalar joint. This knowledge can facilitate performance of arthroscopic techniques and recognition of abnormal pathology in the subtalar joint.
1. Inman VT. The subtalar joint. In: The Joints of the Ankle. Baltimore, MD: Williams & Wilkins; 1976:35-44.
2. Perry J. Anatomy and biomechanics of the hindfoot. Clin Orthop, 1983;177 9-15.
3. Parisien JS. Arthroscopy of the posterior subtalar joint. In Current Techniques in Arthroscopy, 3rd ed, New York, NY: Thieme; 1998:161-168.
4. Parisien JS. Posterior subtalar joint arthroscopy. In: Guhl JF, Parisien JS, Boynton MD, editors. Foot and Ankle Arthroscopy. 3rd ed. New York, NY: Springer-Verlag; 2004:175-182.
5. Frey C, Feder KS, DiGiovanni C. Arthroscopic evaluation of the subtalar joint. does sinus tarsi syndrome exist, Foot Ankle Int. 201999 185-191.
6. van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16:871-876.
7. Frey C, Gasser S, Feder K. Arthroscopy of the subtalar joint. Foot Ankle Int. 1994;15:424-428.
8. Lapidus PW. Subtalar joint. its anatomy and mechanics, Bull Hosp Joint Dis. 161955 179-195.
9. Viladot A, Lorenzo JC, Salazar J, Rodriguez A. The subtalar joint. embryology and morphology, Foot Ankle. 51984 54-66.
10. de Palma L, Santucci A, Ventura A, Marinelli M. Anatomy and embryology of the talocalcaneal joint. Foot Ankle Surg. 2003;9:7-18.
11. Harper MC. The lateral ligamentous support of the subtalar joint. Foot Ankle. 1991;11:354-358.
12. Beimers L, Frey C, van Dijk CN. Arthroscopy of the posterior subtalar joint. Foot Ankle Clin. 2006;11:369-390.
13. Tasto JP. Arthroscopic subtalar arthrodesis. Tech Foot Ankle Surg. 2003;2:122-128.
14. Gavlik JM, Rammelt S, Zwipp H. The use of subtalar arthroscopy in open reduction and internal fixation of intra-articular calcaneal fractures. Injury. 2002;33:63-71.
15. Gavlik JM, Rammelt S, Zwipp H. Percutaneous, arthroscopically assisted osteosynthesis of calcaneus fractures. Arch Orthop Trauma Surg. 2002;122:424-428.
16. Jerosch J. Subtalar arthroscopy—indications and surgical technique. Knee Surg Sports Traumatol Arthrosc. 1998;6:122-128.
17. Lijoi F, Lughi M, Baccarani G. Posterior arthroscopic approach to the ankle. an anatomic study, Arthroscopy. 192003 62-67.
18. Sitler DF, Amendola A, Bailey CS, et al. Posterior ankle arthroscopy. an anatomic study, J Bone Joint Surg Am. 84A2002 763-769.
19. Mekhail AO, Heck BE, Ebraheim NA, Jackson WT. Arthroscopy of the subtalar joint. establishing a medial portal, Foot Ankle Int. 161995 427-432.
20. Feiwell LA, Frey C. Anatomic study of arthroscopic portal sites of the ankle. Foot Ankle. 1993;14:142-147.
21. Chao W. Os trigonum. Foot Ankle Clin. 2004;9:787-796. vii
22. Marumoto JM, Ferkel RD. Arthroscopic excision of the os trigonum. a new technique with preliminary clinical results, Foot Ankle Int. 181997 777-784.
23. Williams MM, Ferkel RD. Subtalar arthroscopy. indications, technique, and results, Arthroscopy. 141998 373-381.