CHAPTER 20 Great Toe Arthroscopy
Arthroscopy of the first metatarsophalangeal joint (MTP-1) was originally described by Watanabe in 1972.1 Because of the small size of the joint, the applicability of arthroscopy has been limited by the small number of clinical results reported in the literature. Advances in technology for visualization and instrumentation and the recent clinical experience of the surgeons have propelled small joint arthroscopy into a new era. Although arthroscopy in the MTP-1 has not been as widely used as arthroscopy in the knee or the shoulder, its value has been demonstrated, and its use continues to grow for the treatment of traumatic and degenerative conditions and for reconstructive procedures. With proper patient selection and familiarity with the technique, MTP-1 arthroscopy can be a useful addition to the surgeon’s armamentarium.
NORMAL AND PATHOLOGIC ANATOMY
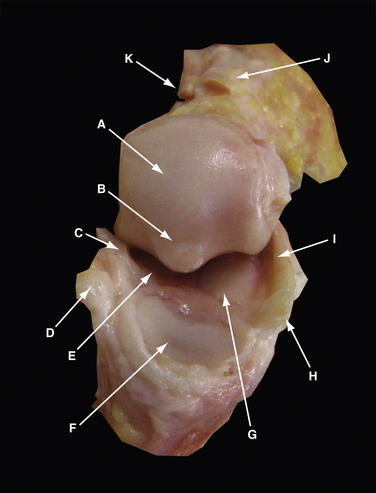
The MTP-1 is composed of the first metatarsal head and neck, proximal phalangeal base, and medial and lateral sesamoids. The first metatarsal articular surface is composed of two fields in continuity, the superior phalangeal and inferior sesamoidal fields. The former is smaller and convex, whereas the latter is larger and separated into two sloped surfaces by a small bony ridge or crista (Fig. 20-1). The proximal phalanx articular surface is oval, concave, and smaller than the corresponding articular surface of the metatarsal head. The base of the proximal phalanx serves as insertions of the extensor hallucis brevis and longus dorsally and the intrinsic muscles of the big toe and plantar plate plantarly.
The dorsomedial aspect of the joint contains a sizable synovial fold, with the average width of 7 mm and covering 29% of the joint.2 It has abundant blood supply, but the nerve supply is found only in the periphery.
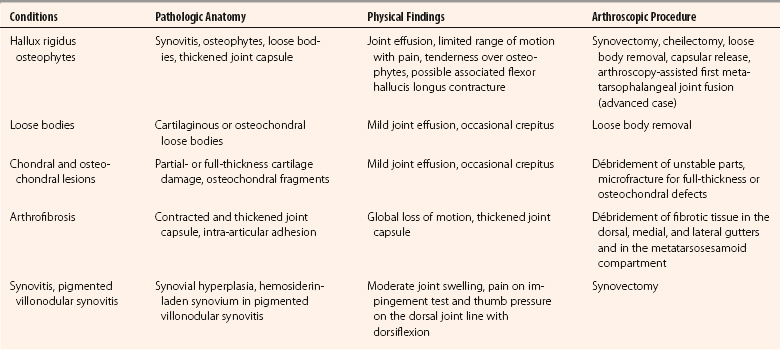
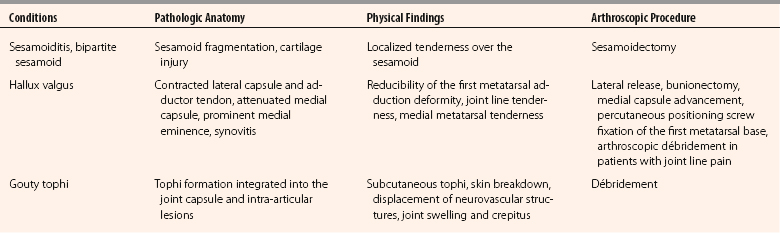
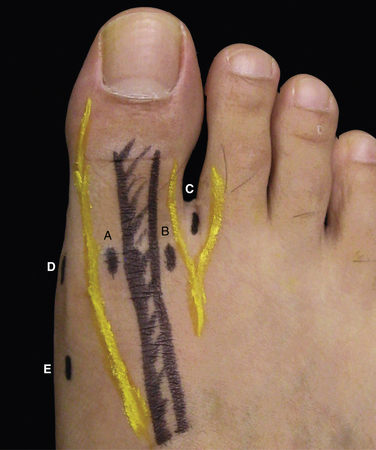
At the level of the MTP-1, the distribution of the cutaneous nerve varies, but the dorsomedial and dorsolateral cutaneous branches usually originate from the medial dorsal cutaneous branch of the superficial peroneal nerve and the deep peroneal nerve, respectively (Fig. 20-2). The plantar medial and plantar lateral branches originate from the medial plantar nerve. The dorsomedial cutaneous nerve lies close to the dorsomedial portal and is on average 13.1 mm medial to the extensor hallucis longus tendon,3 but it has been reported to be 2 to 5 mm from it.4 The plantar medial hallucal nerve is on average 10.6 mm plantar to the midline, which is the location for the medial portal. Because of the variations of the nerves in the foot, all the arthroscopic portals should be handled as if a nerve was located directly underneath. The pathologic anatomy of various conditions of the MTP-1 that can be addressed arthroscopically or endoscopically are listed in Table 20-1.
PATIENT EVALUATION
History and Physical Examination
Patients with MTP-1 problems usually present with forefoot pain. Obtaining a problem-focused history should include the characteristics of pain, swelling, deformities, associated injuries, preexisting diseases, shoewear, prior treatments, and a family history. Athletic activities and expectation are also important factors. Systemic diseases can be associated with increased uric acid and urate crystal arthropathy, which is a common cause of MTP-1 pain.5
Physical examination is the cornerstone of all clinical judgments. We always perform a systematic and thorough examination of all patients with foot and ankle problems, starting with gait, skin, motor, motion, palpation, and special tests. Patients with considerable pain in the MTP-1 may walk on the lateral border of the foot. The forefoot should be observed for deformities, swelling, and discoloration. Active and passive motion of the MTP-1 should be evaluated and compared with the contralateral side. The average passive motion of the MTP-1 in men older than 45 years is 87 degrees, with 67 degrees of dorsiflexion and 20 degrees of plantar flexion.6 Patients with decreased range of motion of the MTP-1 should be differentiated by the characteristics of stiffness. Arthrofibrosis or osteoarthrosis may result in global loss of motion, whereas an early hallux rigidus may produce primarily limited dorsiflexion. Pseudo-hallux rigidus can mimic or be associated with a hallux rigidus, but the tightness from the flexor hallucis longus tendon contracture can usually be decreased by ankle plantar flexion.7 Occasionally, crepitus can be differentiated from arthritis, osteochondral injury, or loose bodies. Pain can be provoked with forced dorsiflexion in patients with hallux rigidus or soft tissue impingement. Bony landmarks, such as the head of the first metatarsal and the base of the proximal phalanx, are superficial and easily palpable. Pain in daily activities often can be reproduced by direct palpation over the osteophytes or the sesamoids.
In hallux valgus, the first metatarsal adduction can be evaluated if it can be manually corrected, which is a requirement for an endoscopic correction of hallux valgus deformity.8 Sometimes, complete correction may not be achieved because of obstruction by the dislocated fibular sesamoid bone in the web space. This is not a contraindication for the procedure, because the sesamoid bone can be reduced after lateral release, and the intermetatarsal space can then be closed. Specific physical examinations for various pathologies of the MTP-1 that are amendable to arthroscopic treatment are listed in Table 20-1.
Diagnostic Imaging
We use standard weight-bearing anteroposterior, lateral, and axial sesamoid views for initial evaluation of all patients with forefoot problems (Fig. 20-3). Osteophytes, joint space narrowing, and loose bodies usually can be demonstrated.
Elevation of the first metatarsal in relation to the lesser metatarsals can be associated with hallux rigidus.9 Inflammatory arthropathy can develop juxta-articular osteopenia or joint destruction in the late stages, whereas gouty tophi often have juxta-articular punch-out lesions and soft tissue thickening. Hallux valgus requires measurements of the hallux valgus angle, intermetatarsal angle, distal metatarsal articular angle, and proximal phalanx articular angle. Oblique views may be helpful in visualizing dorsal MTP-1 osteophytes, the joint space, and the profile of an individual sesamoid.
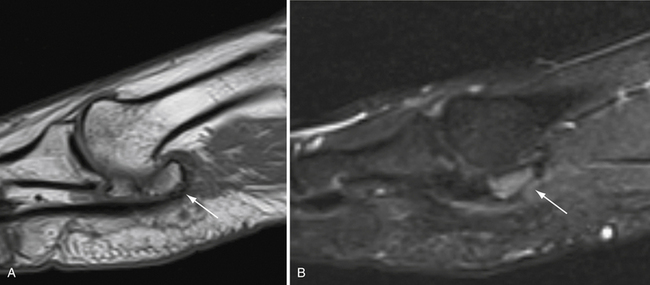
Computed tomography (CT) is rarely indicated, but it can better visualize the osteochondral lesions or loose bodies with an osseous component. Magnetic resonance imaging (MRI) can demonstrate a bone bruise, cartilage defects, and synovial hyperplasia, especially with pigmented villonodular synovitis (PVNS), which has low signal intensity on T1-weighted and T2-weighted images.10 MR images of a symptomatic, bipartite medial sesamoid are shown in Figure 20-4. Ultrasound imaging is advantageous in the forefoot because of its magnification power and real-time visualization.11 It can identify loose bodies and small bone spurs. The probe can also be used to reproduce pain with direct pressure over the suspected location.
TREATMENT
Indications and Contraindications
Arthroscopic Technique
Positioning
We prefer to do the arthroscopy of the MTP-1 with the patient in a supine position and with both hips in abduction (Fig. 20-5). The surgeon has 360-degree access to the forefoot, but most of the procedures can be done with the surgeon at the end of the bed. Plantar portals, if needed, can be approached with the surgeon sitting between the patient’s legs.
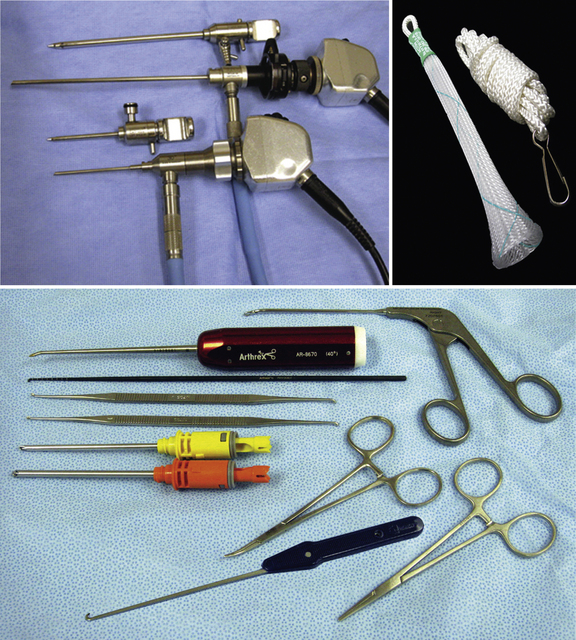
Instruments
A 1.9- or 2.7-mm, 30-degree, small joint arthroscope is used for most arthroscopic visualization of the MTP-1. The 1.9-mm arthroscope is used in tight joints, especially when no traction is applied, but it should be handled with care because of its fragility. A 4-mm, 30-degree arthroscope, which provides a wider field of view and easier orientation, is helpful in periarticular endoscopy, such as in a first web space release and gouty tophi excision. The gravity-driven inflow usually is adequate, and the arthroscopic pump is rarely required. An alternative is to use a 50-mL syringe with continuous irrigation controlled by an assistant. Small bone-cutting shavers allow soft tissue and bone débridement, which can minimize instrument switching. Equipment is listed Box 20-1 and Figure 20-6.
Portals
Dorsomedial and dorsolateral portals are commonly used as the main arthroscopic portals for most MTP-1 pathology (Fig. 20-7). The dorsomedial portal is at the level of joint line and just medial to the extensor hallucis longus tendon joint. The dorsolateral portal is at the same level, but it is just lateral to the extensor hallucis longus tendon. The dorsomedial and dorsolateral hallucal nerves can be directly beneath or can send off a branch close to the dorsal portals.3 The medial portal is at the level of the joint line at the equator of the joint and is positioned away from neurovascular structures (Fig. 20-8). The portal is established through a thick medial capsule by making a longitudinal capsulotomy with a no. 15 blade.
The combination of dorsolateral and medial portals has been more commonly used as the main access route in our experience. It allows a wider distance between portals, reducing crowding of the instruments. The medial portal is particularly helpful in the visualization of the sesamoids, dorsal and plantar gutters, and parts of the metatarsal head.4 The proximal medial portal is in line with the medial portal but is just proximal to the medial eminence. This portal is used for the medial exostectomy.8 The plantar medial portal described for the instrumentation in the metatarsosesamoid compartment is located 4 cm proximal to the joint line and between the abductor hallucis tendon and the medial head of the flexor hallucis brevis.13,19
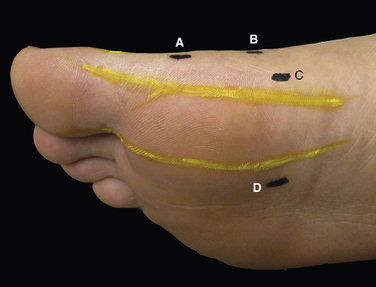
The toe web portal and the plantar portal are required for endoscopic lateral release of the hallux valgus correction and for lateral sesamoidectomy.8,13 The toe web portal is just dorsal to the first web space. The plantar portal is approximately 4 to 5 cm proximal to the web space created inside-out by a Wissinger rod from the toe web portal passing underneath the intermetatarsal ligament. The key to establishing the plantar portal is to make the portal wound just proximal to the point where the rod penetrated the plantar aponeurosis, minimizing the length of the subcutaneous tunnel of the portal tract, which is not the working length of the tract. The toe web portal is relatively safe from the neurovascular structures, but the plantar portal is in the vicinity of the branches from the medial plantar nerve.
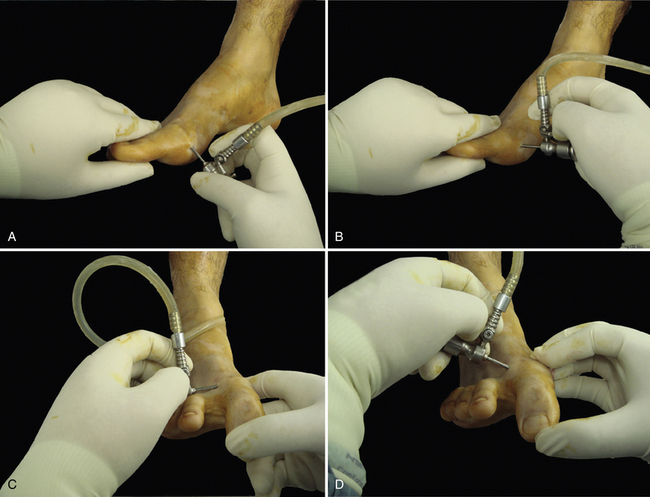
Arthroscopic Examination
The joint line is localized by puckering of the skin with straight traction of the great toe and by direct palpation (Fig. 20-9). The dorsomedial portal is established at the previously described location by making a longitudinal, 3-mm incision followed by blunt dissection with a curved hemostat. The dorsolateral portal and the medial portal placement can be assisted by arthroscopic localization with a 21-gauge needle. Alternatively, the dorsolateral portal can be created first, followed by a medial portal made under direct visualization.
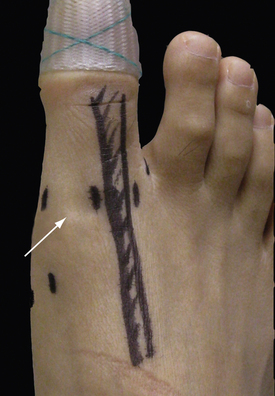
FIGURE 20-9 The skin overlying the joint line is puckered with traction of the great toe in a finger trap.
An easy way to introduce instruments without traction is shown in Figure 20-10. The 13-point examination of the joint has been described by Ferkel to systematically visualize intra-articular structures.4 The areas visualized from the dorsomedial, dorsolateral, and medial portals are shown in Figures 20-11 through 20-13. A 2.0-mm probe is used to palpate the cartilage surface for the detection of softening, crevices, delamination, and osteochondral lesions. Loose bodies are removed with small, straight hemostats, which are preferable over the graspers because of the suction effect that pulls the loose body to the jaws when opened. Sometimes, a tight joint may require manual manipulation to enhance visualization, such as plantar flexion to open the metatarsosesamoid compartment or a combination of traction, plantar flexion, and varus stress for the lateral plantar recess.16

FIGURE 20-11 Several areas can be visualized from the dorsomedial portal: dorsal metatarsal head (A), dorsolateral metatarsal head (B), lateral gutter (C), lateral metatarsophalangeal compartment (D), central metatarsophalangeal compartment (E), and medial metatarsophalangeal compartment (F).
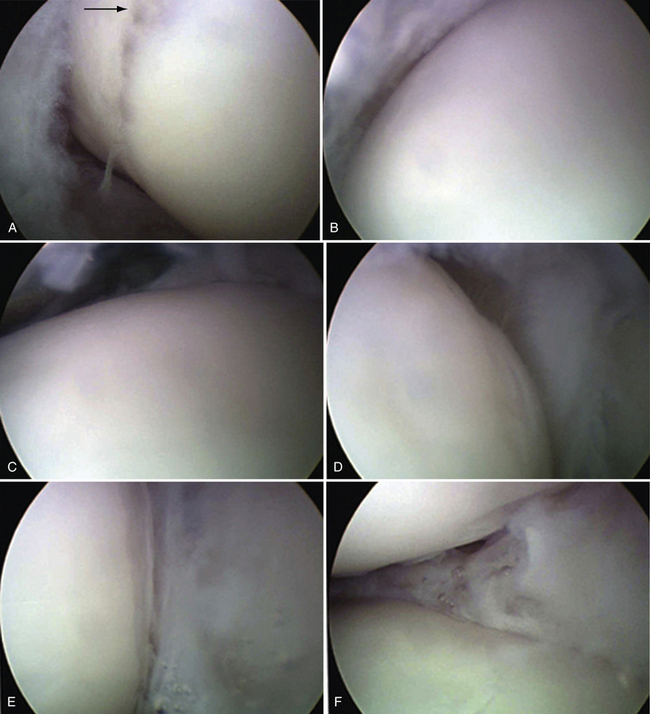
FIGURE 20-12 Several areas can be visualized from the dorsolateral portal: central metatarsal head and the sagittal sulcus (arrow) (A), dorsomedial metatarsal head and medial gutter (B), dorsocentral metatarsal head (C), dorsolateral metatarsal head (D), lateral gutter (E), and lateral metatarsophalangeal compartment (F).
Treatment of Specific Conditions
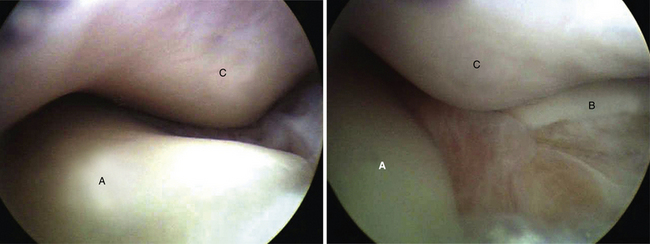
Synovitis and Pigmented Villonodular Synovitis
Treatment of synovitis and soft tissue impingement had good results in a case series.16 Successful treatment of a patient with PVNS of the MTP-1 with arthroscopic synovectomy has been reported.15 Visualization of the (occasionally enlarged) dorsomedial synovial fold is more easily performed through the dorsolateral portal (Fig. 20-14).2 Thorough débridement of the inflamed synovial tissue, which is usually a major pain generator, can be performed with a 3.0-mm, full-radius shaver. Traction is typically not required for a synovectomy. Suction is kept at minimum due to the limited inflow from the small arthroscopic cannula.
Hallux Rigidus and Osteophytes
Van Dijk and colleagues reported good or excellent results in 8 of 12 patients with dorsal impingement and in 2 of 5 patients with hallux rigidus at the 2-year follow-up assessment.13 Iqbal and coworkers reported satisfactory results in all 15 patients with mild to moderate hallux rigidus.12
Small osteophytes can be easily removed with a bone-cutting shaver, with the round-tip abrader reserved for large ones or those with unusually hard bone. For an arthroscopic cheilectomy, the dorsal metatarsal head, including a small amount of articular cartilage, is decompressed until 50 to 70 degrees of dorsiflexion is achieved. If there is any question regarding the amount of the decompression, fluoroscopy can be used. A prominent osteophyte on the proximal phalangeal base should be evaluated and adequately decompressed (Fig. 20-15).
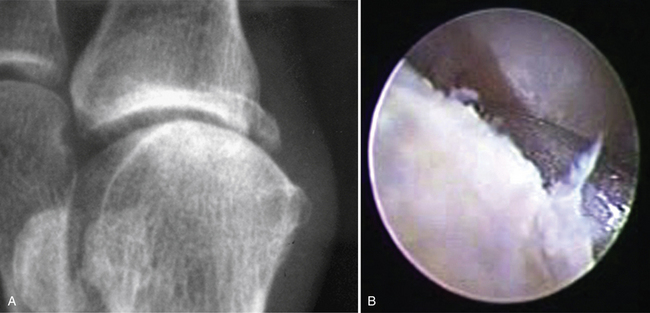
Osteoarthritis
Mild to moderate osteoarthritis of the MTP-1 with pain, which usually is caused by synovitis, is an appropriate indication for an arthroscopic treatment, especially when arthrodesis or arthroplasty is not indicated (Fig. 20-16). However, patients with advanced osteoarthritis with midrange pain have not had lasting benefit from arthroscopic débridement.16,26 Cases with large osteophytes (>5 mm) may have obliteration of the dorsal joint space. This can be handled arthroscopically by first stripping the dorsal capsule with a small periosteal elevator through the dorsal portals to increase the working space (Fig. 20-17).

FIGURE 20-16 Anteroposterior (A) and lateral (C) radiographs of a foot with moderate osteoarthritis show dorsal osteophytes and loose bodies at the first metatarsophalangeal joint. Eburnation of the cartilage is seen on the dorsal aspect of the metatarsal head (B).
The dorsomedial and dorsolateral portals can be established farther away from the extensor tendons at the dorsomedial and the dorsolateral corners of the joint (see Fig. 20-17B). This allows better access for débridement of the osteophytes in the dorsal, medial, and lateral gutters while avoiding crowding of the instruments. For example, the medial osteophytes can be débrided with the dorsolateral portal used as the visualization portal and the dorsomedial portals used as the instrumentation portals. In the event of a large, overhang osteophyte at the metatarsal head, an accessory proximal dorsal portal can be established at the proximal end of the osteophyte. If adequate débridement is not possible arthroscopically, the decision should be made to perform an open débridement.
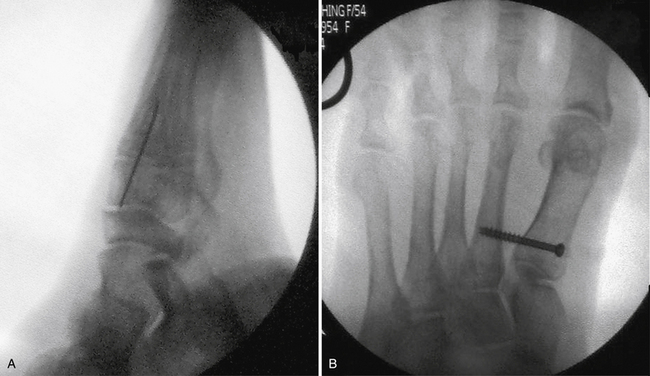
Arthroscopy-assisted arthrodesis has been described for end-stage disease without gross deformity or bone loss.17,18 Dorsomedial, dorsolateral, and medial portals are used together with finger trap traction. Residual cartilage is débrided using curettes, shavers, or abraders. The preserved subchondral bone is microfractured using a small chondral pick (Fig. 20-18). The position of the fusion is 15 degrees of valgus and 20 degrees of dorsiflexion. The provisional fixation is made with a Kirschner wire, and the position is confirmed with fluoroscopy. When the foot is placed flat on a metal tray, the interphalangeal joint should be slightly elevated from the surface. Crossed cannulated screws are inserted under fluoroscopic guidance.
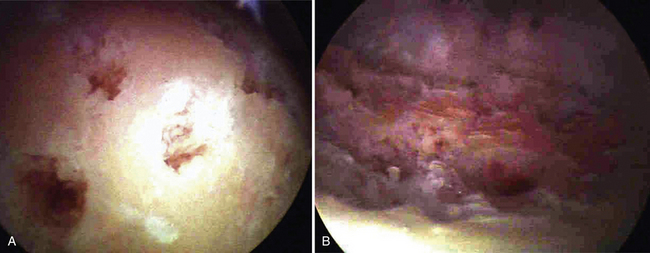
Chondral and Osteochondral Lesions
Chondral and osteochondral lesions have been successfully treated arthroscopically, and the benefits included less pain, less stiffness, and reduced rehabilitation time (Fig. 20-19).13,14,16 In cases with cartilage lesions, the aims are to remove the source of pain, stimulate fibrocartilaginous regeneration, and eliminate mechanical symptoms.
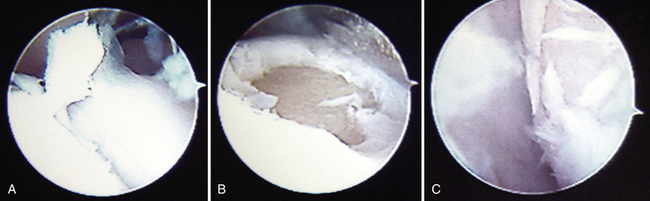
FIGURE 20-19 A full-thickness cartilage lesion on the dorsum of the metatarsal head is visualized before (A) and after (B) débridement. A kissing lesion (C) can be seen in the metatarsosesamoid compartment.
Partial-thickness cartilage injury can be treated with a radiofrequency probe to provide smooth edges. We recommend a microfracture technique using a small joint microfracture probe or a Kirschner wire for a full-thickness cartilage loss or an osteochondral defect. For the in situ osteochondral lesion, the overlying cartilage may look deceptively normal, but with careful palpation with a probe, the lesion can be identified. A curette can be used to remove the osteochondral fragments, although we have found the 2.0-mm probe causes less trauma to the surrounding tissue. Softened cartilage can be easily penetrated and cut with the tip of the probe. The probe can then be used as a hook to pull the fragment loose. The fragment can be débrided with a shaver or removed with hemostats. The defect is further débrided until fresh cancellous surface is uncovered. Microfracture is then performed. The joint is mobilized through range of motion, and any potential location that can provide mechanical catching is smoothed with a radiofrequency probe. A corresponding lesion that may manifest on the proximal phalangeal base should be observed and treated.27
Arthrofibrosis
Arthroscopic lysis of the MTP-1 arthrofibrosis has been reported.19,26 It has the potential advantage of early postoperative rehabilitation, because there is less pain associated with the procedure. Arthroscopic visualization in the joint can be limited by advanced arthrofibrosis.
The routine dorsomedial and dorsolateral portals are employed for the débridement of the dorsal, medial, and lateral gutters. At the initial portal placement, the trocar should be used to free the dorsal fibrotic tissue by sweeping in a back-and-forth fashion. Soft tissue release can involve stripping the medial capsule from the metatarsal head if overplication has occurred from a hallux valgus reconstruction. The sesamoid apparatus can be examined from the medial portal, and a plantar medial working portal is created under direct visualization for the débrider (Fig. 20-20). Plantar flexion of the joint opens the metatarsosesamoid compartment for easier instrumentation. Manual manipulation to achieve maximum range of motion is usually performed after the release.
Sesamoidectomy
The medial and lateral sesamoids can be accessed from the combination of dorsomedial, dorsolateral, medial, and plantar medial portals.24 The evidence is limited, with only case reports presented in the literature. The lateral sesamoid has been removed using the medial portal or the toe web portal for visualization and the plantar medial portal for instrumentation.25 The medial sesamoid has been removed using the dorsolateral portal for visualization and the medial portal for instrumentation.24 The sesamoid can be excised in piecemeal with a pituitary rongeur or a 2.0-mm, round abrader. The ligamentous attachments are preserved. Van Dijk and colleagues found the medial sesamoid excision to be less successful, and an open excision was used in all three cases in their series.13 Excision of both sesamoids is not recommended because of the risk of a cock-up deformity.
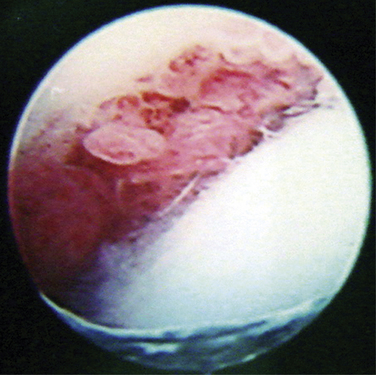
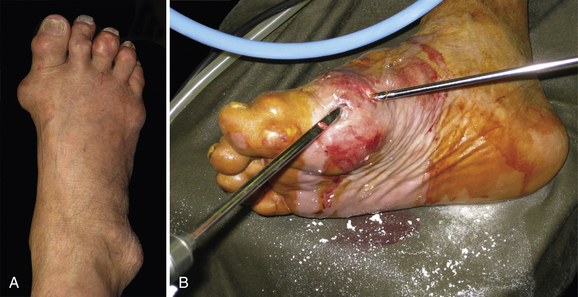
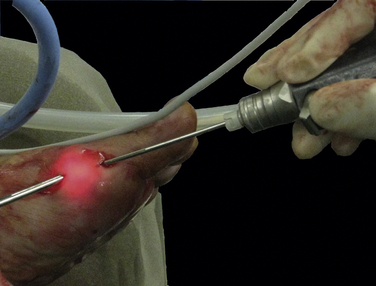
Gouty Tophi
Percutaneous soft tissue shaving of gouty tophi has produced good aesthetic results in 17 patients, with 2 patients having partial skin necrosis and no reported nerve injuries.23 An endoscopy-assisted technique has been described to minimize wound breakdown and persistent drainage.22 A study by Wang and colleagues5 showed superior reduction in the number of acute attacks (5.4 vs. 1.9) and an increase in the American Orthopaedic Foot and Ankle Society (AOFAS) score (20.9 vs. 4.0) after endoscopic débridement (n = 15) compared with medication alone (n = 13) at a minimum of 2 years’ follow-up.
Two portals are localized at the proximal and distal ends of the tophi (Fig. 20-21). A trocar is used to make a tunnel through the tophi that joins both portals. The portals can be used interchangeably for visualization or instrumentation. The tophaceous material is removed with a shaver, progressing from the tunnel toward the pseudocapsule at the periphery. Part of the medial capsule may need to be removed. Great care is used to avoid injury to the dorsomedial hallucal nerve superficial to the pseudocapsule. The dorsolateral portal can be added for intra-articular débridement. The use of warm irrigation fluid is recommended to increase the solubility of the urate and prevent the system from clogging.23 Postsurgical gout attack can be prevented by presurgical control of serum uric acid and prophylactic perioperative administration of colchicine.28,29
Hallux Valgus
Patients with hallux valgus can develop pain at the joint line without bunion pain or difficulties due to the deformity. In a case series of 30 feet, arthroscopic synovectomy through the standard dorsomedial and dorsolateral portals achieved complete pain relief in 22, significant pain relief in 5, and persistent pain in 3 at 5 years’ follow-up.20 Five patients developed bunion pain and required further arthroscopy-assisted correction. For patients with a painful joint line and a hallux valgus requiring correction, synovectomy performed through the described portals can be used in conjunction with deformity correction.
The arthroscopy-assisted correction of hallux valgus deformity has been reported by Lui and associates in a series of 94 patients with reducible 1-2 intermetatarsal angle and normal distal metatarsal articular angle.8 The average hallux valgus angle improved from 33 ± 7 degrees to 14 ± 5 degrees, and the intermetatarsal angle improved from 14 ± 3 degrees to 9 ± 2 degrees°. The postoperative AOFAS score was 93, and the satisfaction rate was 95.7%. Complications included hallux varus, skin impingement, screw breakage, and MTP-1 stiffness.
The lateral release is performed through the toe web and the plantar portals. Under arthroscopic visualization through the plantar portal, the intermetatarsal ligament, adductor hallucis tendon, and lateral capsule are released with a retrograde knife (Fig. 20-22). Manipulation is performed to bring the toe to at least neutral alignment. The sesamoid reduction can be evaluated from the toe web portal or the medial portal. The medial portal and the proximal medial portal are used interchangeably for the arthroscope and the round abrader for the medial exostectomy (Fig. 20-23). The sagittal sulcus is a landmark that can be visualized from the dorsolateral portal. Through the medial and proximal medial portals, the medial capsule is percutaneously plicated with a no. 1 PDS suture to pull the distal plantar part toward the proximal dorsal part. The intermetatarsal angle is manually closed, and fixation with a 4.0 cannulated screw is performed under fluoroscopic guidance (Fig. 20-24).30 The PDS suture is tied afterward (Fig. 20-25).
PEARLS& PITFALLS
PEARLS
PITFALLS
1. Watanabe M. Selfox-Arthroscope (Wantantabe No. 24 Arthroscope). Tokyo, Japan: Teishin Hospital; 1972.
2. Lidtke RH, George J. Anatomy, biomechanics, and surgical approach to synovial folds within the joints of the foot. J Am Podiatr Med Assoc. 2004;94:519-527.
3. Solan MC, Lemon M, Bendall SP. The surgical anatomy of the dorsomedial cutaneous nerve of the hallux. J Bone Joint Surg Br. 2001;83:250-252.
4. Ferkel R. Great-toe arthroscopy. In: Whipple T, editor. Arthroscopic Surgery: The Foot & Ankle. Philadelphia, PA: Lippincott-Raven; 1996:255-272.
5. Wang CC, Lien SB, Huang GS, et al. Arthroscopic elimination of monosodium urate deposition of the first metatarsophalangeal joint reduces the recurrence of gout. Arthroscopy. 2009;25:153-158.
6. Browne K, Lee J. The appreciation of passive movement of the metatarsophalangeal joint of the great toe in man 10-1P. J Physiol. 1231954.
7. Michelson J, Dunn L. Tenosynovitis of the flexor hallucis longus. a clinical study of the spectrum of presentation and treatment, Foot Ankle Int. 262005 291-303.
8. Lui TH, Chan KB, Chow HT, et al. Arthroscopy-assisted correction of hallux valgus deformity. Arthroscopy. 2008;24:875-880.
9. Roukis TS. Metatarsus primus elevatus in hallux rigidus. fact or fiction?, J Am Podiatr Med Assoc. 952005 221-228.
10. Masih S, Antebi A. Imaging of pigmented villonodular synovitis. Semin Musculoskelet Radiol. 2003;7:205-216.
11. Fessell DP, van Holsbeeck M. Ultrasound of the foot and ankle. Semin Musculoskelet Radiol. 1998;2:271-282.
12. Iqbal MJ, Chana GS. Arthroscopic cheilectomy for hallux rigidus. Arthroscopy. 1998;14:307-310.
13. van Dijk CN, Veenstra KM, Nuesch BC. Arthroscopic surgery of the metatarsophalangeal first joint. Arthroscopy. 1998;14:851-855.
14. Bartlett DH. Arthroscopic management of osteochondritis dissecans of the first metatarsal head. Arthroscopy. 1988;4:51-54.
15. Borton DC, Peereboom J, Saxby TS. Pigmented villonodular synovitis in the first metatarsophalangeal joint. arthroscopic treatment of an unusual condition, Foot Ankle Int. 181997 504-505.
16. Debnath UK, Hemmady MV, Hariharan K. Indications for and technique of first metatarsophalangeal joint arthroscopy. Foot Ankle Int. 2006;27:1049-1054.
17. Carro LP, Vallina BB. Arthroscopic-assisted first metatarsophalangeal joint arthrodesis. Arthroscopy. 1999;15:215-217.
18. Stroud CC. Arthroscopic arthrodesis of the ankle, subtalar, and first metatarsophalangeal joint. Foot Ankle Clin. 2002;7:135-146.
19. Lui TH. Arthroscopic release of first metatarsophalangeal arthrofibrosis. Arthroscopy. 2006;22:906.e1-906.e4.
20. Lui TH. First metatarsophalangeal joint arthroscopy in patients with hallux valgus. Arthroscopy. 2008;24:1122-1129.
21. Lui TH, Ng S, Chan KB. Endoscopic distal soft tissue procedure in hallux valgus surgery. Arthroscopy. 2005;21:1403.
22. Lui TH. Endoscopic resection of the gouty tophi of the first metatarsophalangeal joint. Arch Orthop Trauma Surg. 2008;128:521-523.
23. Lee SS, Lin SD, Lai CS, et al. The soft-tissue shaving procedure for deformity management of chronic tophaceous gout. Ann Plast Surg. 2003;51:372-375.
24. Perez Carro L, Echevarria Llata JI, Martinez Agueros JA. Arthroscopic medial bipartite sesamoidectomy of the great toe. Arthroscopy. 1999;15:321-323.
25. Chan PK, Lui TH. Arthroscopic fibular sesamoidectomy in the management of the sesamoid osteomyelitis. Knee Surg Sports Traumatol Arthrosc. 2006;14:664-667.
26. Ferkel R, Buecken KV. Great toe arthroscopy. indications, technique and results. April, 1991 Presented at the Arthroscopy Association of North America San Diego, CA
27. Shonka TE. Metatarsal phalangeal joint arthroscopy. J Foot Surg. 1991;30:26-28.
28. Kang EH, Lee EY, Lee YJ, et al. Clinical features and risk factors of postsurgical gout. Ann Rheum Dis. 2008;67:1271-1275.
29. Linton RR, Talbott JH. The surgical treatment of tophaceous gout. Ann Surg. 1943;117:161-182.
30. Friscia DA. Distal soft tissue correction for hallux valgus with proximal screw fixation of the first metatarsal. Foot Ankle Clin. 2000;5:581-589.