Chapter 13 Granulomatous diseases of the skin
| Infectious Agents | ||
| Fungi | Bacteria | Miscellaneous Infections |
| Blastomycosis Candidiasis Chromomycosis Coccidioidomycosis Cryptococcosis Histoplasmosis Sporotrichosis |
Actinomycosis Cat scratch fever Granuloma inguinale (donovanosis) Mycobacterial infections Nocardiosis Syphilis Tularemia |
Leishmaniasis Protothecosis (algae infection) |
| Foreign Body Agents | ||
| Exogenous | Endogenous | Miscellaneous Diseases |
| Aluminum Cosmetic fillers Hair Insect parts Paraffin Silica Splinters Starch Sutures Talc Tattoo pigment |
Bone Calcium Cholesterol Keratin Hair Sebum Urate crystals |
Actinic granuloma Crohn’s disease Granuloma annulare Granulomatous cheilitis Granulomatous rosacea Lupus miliaris disseminatus faciei Necrobiosis lipoidica Rheumatoid nodule Sarcoidosis |
| AGENT | SOURCE |
|---|---|
| Silicone | Breast implants, joint prostheses, soft tissue injections, hemodialysis tubing |
| Silica | Soil and rock (very abundant), glass |
| Paraffin (oils) | Cosmetic injection (historically), factitial injection, grease gun injury |
| Starch | Surgical gloves contaminating wounds |
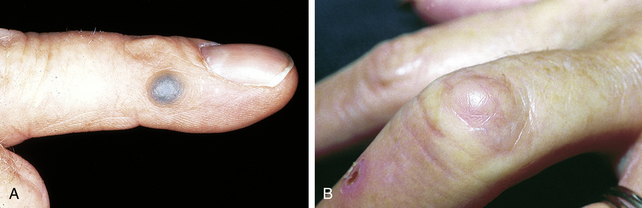
| Graphite | Pencil lead (see Fig. 13-1A) |
| Thorns | Roses, cactus, yucca (see Fig. 13-1B) |
| Hair | Barbers, dog groomers, sheep shearers |
| Talc | IV drug use, wound contamination |
| Aluminum | Adjuvant in DPT immunizations |
| Zirconium | Deodorant sticks |
| Beryllium | Metal, ceramic, and electronic industries; fluorescent lamp workers (historically, as this ceased in 1951) |
DPT, Diphtheria-pertussis-tetanus, IV, intravenous.
Winslow CP: The management of dermal filler complications, Facial Plast Surg 25:124–128, 2009.
Spicknall K, English JC 3rd, Elston DM: Lupus pernio, Cutis 79:289–290, 2007.
Doherty CB, Rosen T: Evidence-based therapy for cutaneous sarcoidosis, Drugs 68:1361–1383, 2008.
Key Points: Cutaneous Sarcoidosis
Stein JA, Fangman B, Strober B: Actinic granuloma, Dermatol Online J 13:19, 2007.

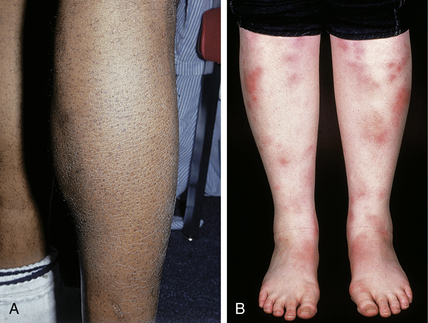
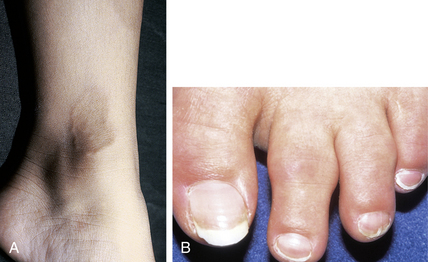
Figure 13-8. Unusually large dermal and subcutaneous rheumatoid nodules in a patient with severe rheumatoid arthritis.
(Courtesy of the Fitzsimons Army Medical Center teaching files.)
García-Patos V: Rheumatoid nodule, Semin Cutan Med Surg 26:100–107, 2007.
McGrath MH, Fleischer A: The subcutaneous rheumatoid nodule, Hand Clin 5:127–135, 1989.
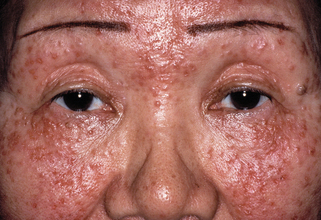
Figure 13-9. Lupus miliaris disseminatus faciei. Numerous red to reddish-brown papules of the central face.
(Courtesy of the Walter Reed Army Medical Center teaching files.)
Sehgal VN, Srivastava G, Aggarwal AK, et al: Lupus miliaris disseminatus faciei. Part II: an overview, Skinmed 4:234–238, 2005.