Gram-Positive Toxigenic Rods
• Bacilli are large, gram-positive, aerobic, spore-forming rods that produce exotoxins.
• B. anthracis is nonmotile (unlike other bacilli) and forms Medusa’s head colonies on blood agar.
• Capsule composed of glutamic acid polymer prevents phagocytosis and antibody plus complement lysis.
• Anthrax toxin causes localized edema and cell death; highly toxic.
• Spores are extremely stable and can survive many years in soil, wool, hair, and animal hides.
2. Diseases caused by B. anthracis
• Anthrax is an occupational disease of individuals who handle wools, furs, and hides.
a. Cutaneous anthrax results from inoculation of spores or bacteria from soil or animal products into a superficial wound or abrasion.
• Marked by initial itching papule at inoculation site; ulcer with vesicles that can lead to necrosis with massive edema, septicemia, and possible death
b. Pulmonary anthrax is due to inhalation of spores from contaminated items such as wool, fur, and hides.
c. Gastrointestinal anthrax results from ingestion of bacteria in contaminated meat.
• Vaccination of animals and proper disposal of infected animals are important in controlling anthrax.
• Human vaccination is restricted to at-risk individuals (fur and wool handlers, military) and those living where disease is endemic.
• Prompt therapy is essential to reduce risk for death: amoxicillin if penicillin sensitive, otherwise ciprofloxacin (a fluoroquinolone).
• B. cereus, a ubiquitous soil organism found in grains, vegetables, and dairy products, is the most common pathogenic bacilli.
• Emetic form is caused by preformed heat-stable enterotoxin ingested in reheated foods (e.g., rice and beans).
a. Rapid onset (similar to S. aureus food poisoning); nausea, vomiting, and abdominal cramps developing within 1 to 5 hours after eating toxin-containing food
• Diarrheal form is caused by heat-labile enterotoxin produced by bacteria multiplying in the gastrointestinal (GI) tract following ingestion of contaminated meat, vegetables, or sauces.
• Refrigeration of foods after cooking
a. Spores survive initial cooking and will germinate into toxin-producing vegetative cells if foods are not refrigerated properly. Later reheating inactivates heat-labile toxin but does not affect vegetative cells or heat-stable toxin.
• Supportive therapy (e.g., replenish fluids and electrolytes)
• Four clostridial species are important human pathogens: C. botulinum, C. difficile, C. perfringens, and C. tetani.
• Clostridia are gram-positive, anaerobic (or aerotolerant), spore-forming rods that produce potent exotoxins.
• C. perfringens is found worldwide in soil, water, and sewage; normal inhabitant of the GI tract.
• Large, boxcar-shaped, aerotolerant, rapidly growing rods
• Double zone of hemolysis on blood agar
• Positive Nagler reaction (characteristic diffuse zone around colonies grown on egg yolk agar)
• Subtypes A to E defined based on production of major toxins
• Type A C. perfringens is most virulent in humans.
a. Alpha toxin (phospholipase C and lecithinase), produced by all types, causes lysis of blood cells and endothelial cells, leading to increased vascular permeability, hemolysis, and tissue destruction.
b. Hyaluronidase, collagenase, and other degradative enzymes cause tissue destruction.
c. Heat-labile enterotoxin disrupts ion transport in ileum, leading to watery diarrhea (food poisoning).
• C. tetani is present in soil, water, and sewage; part of the normal flora of many animals
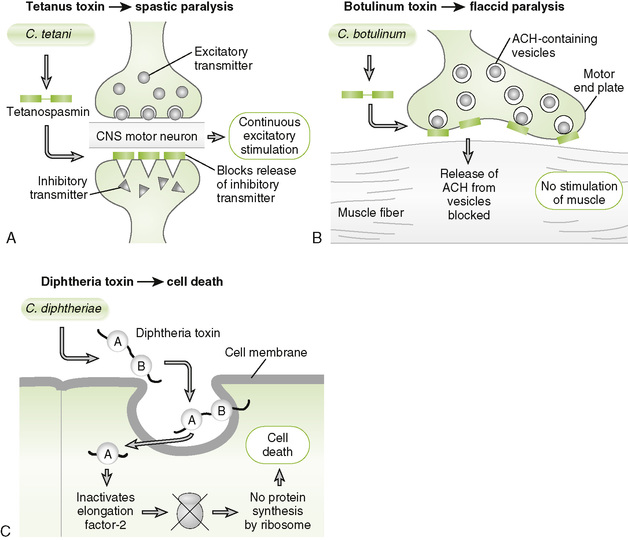
• Tetanospasmin, an A-B type neurotoxin, blocks release of inhibitory neurotransmitters (e.g., γ-aminobutyric acid and glycine), resulting in spastic paralysis due to unregulated excitatory synaptic activity (Fig. 10-1A).
a. Binding of B subunit to peripheral neurons at the site of infection promotes uptake of A subunit, which then travels to the central nervous system and exerts a blocking effect at inhibitory synapses.
• Spore formation permits survival in unfavorable conditions.
3. Diseases caused by C. tetani
• Infection is acquired via entry of spores from contaminated materials (e.g., dirty nails and splinters) into a cut or stab wound.
• Generalized tetanus: onset usually within 1 week of exposure
a. Spasms of masticatory muscles (trismus, lockjaw), drooling, sweating, irritability, persistent back spasms (opisthotonos), and sardonic grin (risus sardonicus)
• Localized tetanus: later onset and less serious unless progresses to generalized form
• Vaccination with tetanus toxoid (formaldehyde-inactivated toxin) administered as part of the DPT or DT vaccine
• Treatment for unvaccinated individuals
a. Supportive care (e.g., muscle relaxants, oxygen) to reduce spasms and maintain breathing until circulating toxin is metabolized
b. Passive immunization with human antitoxin immunoglobulin to neutralize circulating tetanospasmin
c. Débridement of the primary wound and penicillin therapy to eliminate clostridial cells
• Botulinum toxin in patient specimens or food is detected by immunoassay.
• Botulinum toxin, an A-B type neurotoxin, blocks release of acetylcholine at cholinergic synapses, leading to flaccid paralysis (Fig. 10-1B).
a. B subunit binds to nerve cells; internalized A subunit exerts neurotoxic effect. Recovery period is prolonged because nerve endings affected by toxin must regenerate.
• Spores are heat resistant, but the toxin and bacteria are not.
2. Diseases caused by C. botulinum
• Classic food-borne botulism results from ingestion of preformed toxin, most commonly present in improperly prepared home-canned foods.
a. Variable onset of symptoms, including weakness and dizziness; blurred vision, fixed and dilated pupils; dry mouth; flaccid paralysis; and death from respiratory paralysis
b. Spores that survive the canning procedure may germinate and produce toxin in sealed, anaerobic containers.
• Infant botulism is associated with ingestion of honey contaminated with C. botulinum, which colonizes the GI tract and produces toxin in vivo.
a. Most common form of botulism in the United States, primarily affecting infants younger than 1 year of age.
b. Initial nonspecific symptoms (e.g., failure to thrive and constipation) may progress to flaccid paralysis (floppy baby syndrome) and respiratory arrest (in 1% to 2% of patients).
• Wound botulism results from skin inoculation and local in vivo production of toxin, leading to disease clinically similar to food-borne botulism.
• Proper canning techniques and adequate heating of home-canned food, which inactivates any toxin present
• Administration of trivalent antitoxin against the major toxin types (A, B, and E) as early as possible in all forms of botulism
• Emptying of stomach contents, respiratory support, and penicillin (in infant and wound botulism)
• C. difficile is part of normal intestinal flora in some individuals.
• Toxin in stool samples is detected by immunoassay or by its ability to kill cultured cells (cytotoxicity test).
• Resistance to certain antibiotics may permit overgrowth or acquisition of C. difficile in patients receiving these drugs for other infections.
• Enterotoxin (toxin A) promotes fluid secretion and intestinal hemorrhage (similar to cholera toxin).
• Cytotoxin (toxin B) damages mucosal membranes by depolymerizing cellular cytoskeleton.
• Adhesion factor binds to human colon cells.
• Spores are insensitive to oxygen and resistant to many disinfectants, including alcohol-based hand cleaners, making their elimination from hospital environments difficult.
2. Pseudomembranous colitis due to C. difficile
• Patients on antibiotic therapy develop profuse, foul-smelling, liquid, sometimes bloody diarrhea. Leukocytes in the stool, fever, and abdominal pain may also be present.
• Disease can be acquired endogenously or exogenously via spores, which are often spread nosocomially on hands of hospital workers or fomites.
• Discontinuation of causative antibiotic therapy is sufficient treatment in mild cases. More serious cases may also require treatment with metronidazole, vancomycin, or even bacitracin.
III Corynebacterium diphtheria
• C. diphtheriae is the only significant human pathogen in the genus Corynebacterium.
1. Diphtheria toxin, an A-B type exotoxin, inhibits protein synthesis in mammalian cells, leading to cell death and disease manifestations (Fig. 10-1C).
C Diseases caused by C. diphtheriae
1. Respiratory diphtheria is acquired by inhalation of respiratory droplets from infected individuals, including asymptomatic immunized carriers (Box 10-2).
2. Cutaneous (wound) diphtheria is acquired by skin contact and entrance of organism via breaks in the skin.
• Initial papule develops into chronic, nonhealing ulcer; systemic effects, if present, usually are mild.
3. Systemic toxemia can cause damage to distant organs (e.g., myocarditis, neuropathy, and renal tubular necrosis).