Gonadal function
Male gonadal function
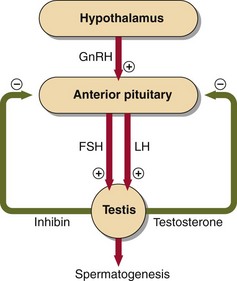
The testes secrete testosterone and manufacture spermatozoa. Before puberty, gonadotrophin and testosterone concentrations in plasma are very low. The development of the Leydig cells and their secretion of testosterone is influenced by LH, whereas Sertoli cell function is influenced by FSH (Fig 50.1). Testosterone is responsible for the development of the male secondary sex characteristics such as hair growth, deep voice and characteristic musculature.
Disorders of male sex hormones
Causes of primary hypogonadism include:
 congenital defects such as Klinefelter’s syndrome or testicular agenesis
congenital defects such as Klinefelter’s syndrome or testicular agenesis
 acquired defects due to testicular infections (e.g. mumps), trauma, irradiation, or cytotoxic drugs.
acquired defects due to testicular infections (e.g. mumps), trauma, irradiation, or cytotoxic drugs.
Female gonadal function
Oestradiol is responsible for:
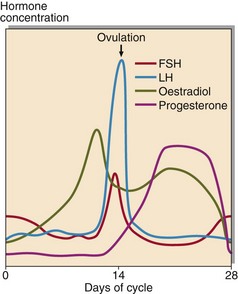
The normal hormonal control of the menstrual cycle is shown in Figure 50.2. At the beginning of the cycle, FSH is released and initiates follicular growth. At mid-cycle a surge of LH triggers ovulation. The ruptured follicle differentiates into the corpus luteum that secretes progesterone and oestradiol whose target is the endometrium, which they prepare for implantation.
Disorders of female sex hormones
Disorders of female sex hormones include:
 Subfertility, amenorrhoea and oligomenorrhoea (see p. 102).
Subfertility, amenorrhoea and oligomenorrhoea (see p. 102).
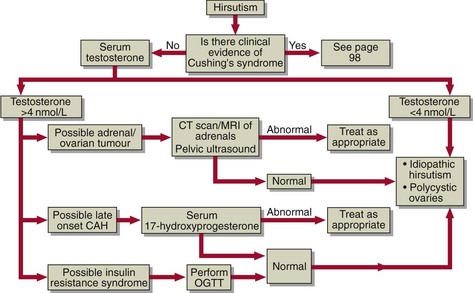
 Hirsutism. This is an increase in body hair with male pattern distribution. It may be idiopathic but the commonest pathological cause is obesity (insulin resistance) often in association with polycystic ovarian disease. It is essential when investigating hirsute women that serious disease is excluded. A diagnostic decision chart for the investigation of hirsutism is shown in Figure 50.3.
Hirsutism. This is an increase in body hair with male pattern distribution. It may be idiopathic but the commonest pathological cause is obesity (insulin resistance) often in association with polycystic ovarian disease. It is essential when investigating hirsute women that serious disease is excluded. A diagnostic decision chart for the investigation of hirsutism is shown in Figure 50.3.
 Virilism. Although uncommon it is a sign of serious disease. Testosterone concentrations are markedly elevated in the virilized patient and there is evidence of excessive androgen action such as clitoral enlargement, hair growth in a male pattern, deepening of the voice and breast atrophy. Tumours of the ovary or of the adrenal are the likely cause.
Virilism. Although uncommon it is a sign of serious disease. Testosterone concentrations are markedly elevated in the virilized patient and there is evidence of excessive androgen action such as clitoral enlargement, hair growth in a male pattern, deepening of the voice and breast atrophy. Tumours of the ovary or of the adrenal are the likely cause.
The androgen screen in women
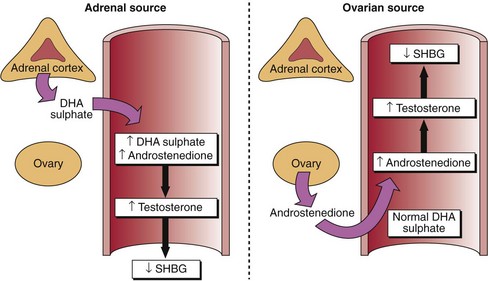
The observation of an elevated testosterone in a woman should always be investigated further. A decreased SHBG concentration is usually evidence of elevated androgen, as the synthesis of this protein in the liver is depressed by testosterone. By measuring the concentration of other androgens such as androstenedione and DHA sulphate (an ‘androgen screen’), the source of the testosterone can be pinpointed (Fig 50.4). An elevated DHA sulphate suggests that the adrenal, or an adrenal tumour, is overproducing androgens. If the ovary is the source then only androstenedione will be raised.