CHAPTER 11 Gluteal Flap Breast Reconstruction
Summary/Key Points
Patient Selection
Breast reconstruction using autologous tissue has been performed for several decades and has become a safe and reliable technique.1 Abdominal flaps, either pedicled or free, remain the first choice for breast reconstruction using autologous tissue. However, in patients who are very thin or who had previously undergone abdominoplasty or prior breast reconstruction with an abdominal flap, a gluteal flap can be an excellent alternative.2–5
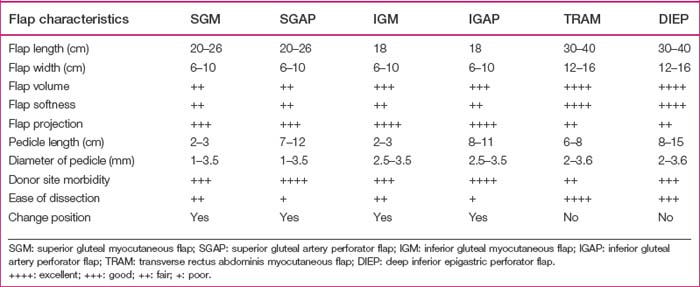
The reconstructed breast mound using gluteal flaps may have more projection, but not be as soft or mobile as when using abdominal flaps. Patient selection should be based on the patient’s individual characteristics, such as the volume of tissue required to achieve symmetry with the contralateral breast, the donor flap size, the pedicle length and caliber, and the relative advantages and disadvantages of each flap (Table 11.1). In patients with inadequate abdominal tissue or in whom an abdominal flap had been used before, gluteal flaps present an alternative for autologous breast reconstruction.6–8 Selection between the SGAP or IGAP flap depends on the patient’s desired scar position, distribution of adiposity, and where sizable perforators can be found (Table 11.1). In patients with a sagging buttock, the IGAP flap is usually preferred. We prefer to harvest a perforator flap rather than a myocutaneous flap to obtain a longer pedicle and to avoid sacrifice of the gluteus maximus muscle.
Indications
Indications for using gluteal flaps for breast reconstruction include:
Contraindications include previous buttock surgery, buttock liposuction or buttock lift, and heavy tobacco use. Dissection of the SGAP or IGAP flap is technically demanding and is better done by an experienced reconstructive microsurgeon. It is especially difficult in Asian women, who are relatively thin and have tiny perforators.6–8
Operative Technique
Surgical anatomy
After emerging from the external iliac artery, the superior and inferior gluteal arteries pass through the sciatic foramen and become the dominant pedicles of the gluteal maximus muscle. The superior gluteal artery runs superior to the piriformis muscle and gives several branches to the gluteus maximus muscle. A few musculocutaneous perforators go through the gluteus maximus muscle and supply the superolateral aspect of the buttock. The diameter of the major perforators ranges from 1.0 to 1.5 mm in Koshima’s series and averages 3.5 mm in Allen’s report.9,10 This disparity is probably due to the differences among races. The mean pedicle length from the perforator is 8 cm (Table 11.1).
The inferior gluteal artery runs inferior to the piriformis muscle and proximal to the coccygeus muscle. During passage through the sciatic foramen, the inferior gluteal artery is accompanied by the internal pudendal vessels, sciatic nerve, posterior cutaneous nerve of the thigh, and pudendal nerve. It supplies the inferior part of the gluteus maximus muscle. Musculocutaneous perforators pass through the muscle and supply the inferomedial aspect of the buttock. During its intramuscular course on the way to the subcutaneous tissue, the pedicle runs distally, accompanied by the posterior cutaneous nerve of the thigh. To avoid injury to these adjacent neurovascular structures, the dissection of the IGAP flap is more technically demanding than the SGAP flap.11,12 The perforators of the inferior gluteal artery are located along a line in the middle third of the gluteal region above the gluteal crease.13 The diameter of the inferior gluteal artery can be greater than 2 mm when dissection continues to their origin. Average pedicle length is 8 to 11 cm. The mean internal diameter of the perforators was 0.6 ± 0.1 mm in cadaveric dissections.13
Preoperative marking and flap dissection
Superior gluteal artery perforator flap
Preoperative marking
Preoperative marking is done with the patient in the prone or lateral decubitus position. A line is marked from the posterior superior iliac spine to the greater trochanter. The superior gluteal artery is located at the medial one third of this line.3,4 Two or three audible perforators are usually detectible by hand-held pencil Doppler. An elliptical skin paddle is designed around the perforators and its axis can be oriented transversely or obliquely (Fig. 11.1).
Flap dissection
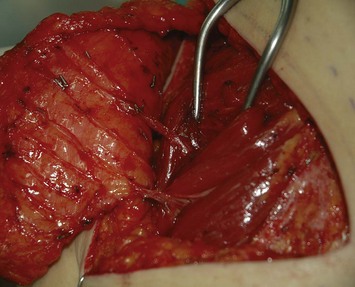
After reaching the subfascial plane, dissection is carried out from lateral to medial to identify the perforators. One large perforator is usually enough to supply the entire flap. After choosing the largest perforator, dissection is continued by splitting the gluteus maximus muscle along the direction of its fibers. A self-retaining retractor is used to spread the fibers of the gluteus maximus muscle. When proceeding to the deeper layer, good exposure of the surgical field by retracting the piriformis muscle is crucial to allow a clear visualization and to prevent any vascular damage. During dissection, any side branches or sacrificed perforators should be adequately coagulated or clamped with hemoclips to prevent postoperative hematoma or seroma accumulation. The perforator is traced to its proximal origin to gain as long a pedicle as possible. A longer pedicle can be obtained by using a perforator located more laterally in the flap. A pedicle averaging 8–12 cm in length can be dissected (Table 11.1). During the procedure, dissection requires an assistant to hold the flap gently and without traction on the pedicle to prevent avulsion or vasospasm. Intermittent irrigation of the pedicle with lidocaine or papaverine and keeping the pedicle moist also prevent vasospasm. Care should be taken to check the pulsation frequently during dissection to ensure that the perforator is intact and is not under too much tension.
Inferior gluteal artery perforator flap
Preoperative marking
Before flap dissection, a hand-held pencil Doppler is used to locate the perforators. The flap is designed as a transverse ellipse that includes the audible perforators (Fig. 11.2). The lower margin of the flap is situated in the gluteal crease to hide the scar (the so-called ‘in-the- crease’ flap).11
Flap dissection
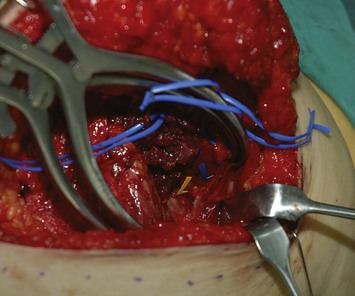
Incisions are made along the markings. A beveling technique can be applied in the superior and inferior margin to include more subcutaneous tissue, 3 cm wider than the skin paddle in each direction. This provides more flap volume and better breast shaping. The flap is elevated in the subfascial plane. When approaching the ischial tuberosity, the important cushion-providing adipose tissue, light brown in color, should be carefully preserved to minimize donor site morbidity. The intramuscular course of the inferior gluteal artery tends to be more tortuous and transverse than that of the superior gluteal artery (Fig. 11.3), and the dissection is more technically demanding. However, a longer pedicle can be obtained with the inferior gluteal artery than the superior gluteal artery (Fig. 11.4). Perforators supplying the lateral gluteal region have a slightly longer intramuscular course than those supplying the medial gluteal region; thus, usage of a lateral perforator can yield a pedicle 1–2 cm longer in length. The posterior cutaneous nerve of the thigh accompanies the inferior gluteal vessels and should be carefully preserved to prevent postoperative numbness of the posterior thigh. When approaching the origin of the perforator, the sciatic nerve may be encountered and must obviously be protected (Fig. 11.5). The surrounding muscle should be kept in place as much as possible to provide adequate coverage of the sciatic nerve after flap elevation. After the intramuscular dissection is finished, the pedicle is divided and the flap transferred. The donor site is closed primarily in layers with 2-0 Vicryl and 3-0 Monocryl, and the patient is turned to the supine position for the remainder of the procedure (Fig. 11.6).
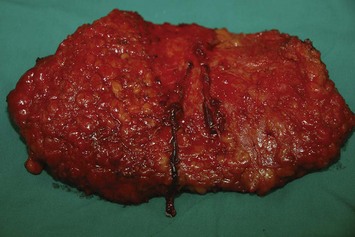
Fig. 11.4 A 10-cm in length pedicle can be dissected with a perforator of the inferior gluteal artery.
Preparation of the recipient site
The recipient site is prepared under loupe magnification when the patient is in the supine position. In a delayed reconstruction, exposure is gained through the previous scar, which is excised and sent for pathologic review. Extensive release of scar tissue is performed to create an adequate breast pocket, especially in the axillary region. The authors prefer to use the internal mammary artery (IMA) and vein (IMV) as the recipient vessels.14 A 1 × 1 cm section of the third costal cartilage is excised, preserving the superior aspect of the perichondrium. The small piece of cartilage is preserved and at the end of the case will be banked in the subcutaneous layer of the lower breast flap for the strut in nipple reconstruction later. The remaining third costal cartilage is removed in the direction of the sternal junction in piecemeal fashion with a rongeur until the recipient vessels are seen. The perichondrium is removed carefully with bipolar electrocautery. Dissection then proceeds under the microscope to prevent damage to the recipient vessels, especially the thin-walled vein. Dissection of the IMA and IMV is performed with two microforceps, gently shearing the adventitia (Fig. 11.7). After the dissection is finished, the wound is closed temporarily and the patient is turned to the prone position for flap elevation.
Donor site closure and morbidity
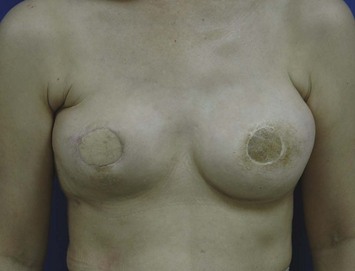
The morbidity of the gluteal donor site is minimal. Splitting the muscle fibers and preserving the motor nerve to the gluteus maximus muscle during pedicle dissection may effectively reduce donor site morbidity. The postoperative ambulation is not restricted in most cases. The most significant morbidities are numbness of the surrounding skin, contour deformity, and minor asymmetry of the buttocks (Figs 11.8 and 11.9).
More donor site morbidities are reported in harvesting the IGAP flap. The inferior gluteal artery accompanies the sciatic nerve when traversing the greater sciatic foramen. Unpreventable exposure of the sciatic nerve during IGAP dissection may result in dysesthesia that persists for several months after surgery. Gentle dissection and preservation of the gluteal muscles minimize this complication. Another important step is to preserve the adipose tissue around the ischial tuberosity when dissecting the IGAP flap to prevent postoperative discomfort with sitting (Box 11.1).
Box 11.1 Summary of the operative steps
Pitfalls and How to Correct
The IGAP flap holds several advantages over the SGAP flap. Usually the inferior gluteal region provides more tissue than the superior gluteal region, and removal of the excess inferior fat is sometimes of benefit to the patient. Flaps harvested from the superior gluteal region leave a scar in the aesthetic unit of the buttock while those from the inferior region leave the scar hidden ‘in- the-crease.’ Figures 11.8–11.12 show a patient who twice underwent immediate breast reconstruction with a gluteal flap each time. In the first reconstruction, the right SGAP flap was used since there was adequate tissue in the superior gluteal area. However, the selection was shifted to the left IGAP flap in the second reconstruction because the patient was concerned about the contour deformity and visible scar left at the right superior gluteal site. The selection should be based on each patient’s individual situation. Figures 11.13–11.16 demonstrate another happy patient receiving breast reconstruction with the SGAP flap. The early concern of sciatic nerve palsy is not a problem with recent approaches. The inferior gluteal area is now considered a better donor site than the superior gluteal area in most situations.11 However, the dissection of tiny perforators of the IGAP flap is extremely difficult and requires a more experienced surgeon to perform. Preoperative Doppler study mapping of the perforators may be helpful in flap design and dissection. However, the benefit of preoperative duplex mapping seems uncertain due to the thicker subcutaneous fat tissue.

Fig. 11.13 A 28-year-old female underwent modified radical mastectomy for right breast cancer, stage 1.
Breast reconstruction using autologous tissue is a challenge for a thin patient presenting with a breast defect post mastectomy with an implant in the submuscular plane. The gluteal region provides adequate soft tissue for symmetric and projecting breast reconstruction (Figs 11.17–11.20).

Fig. 11.18 Same patient as in Figure 11.17. There was adequate soft tissue at the inferior gluteal region to provide breast reconstruction with satisfactory volume.
1 Kroll SS. Why autologous tissue? Clin Plast Surg. 1998;25:135-143.
2 Shaw WW. Breast reconstruction by superior gluteal microvascular free flaps without silicone implants. Plast Reconstr Surg. 1983;72:490-501.
3 Codner MA, Nahai F. The gluteal free flap breast reconstruction: making it work. Clin Plast Surg. 1994;21:289-296.
4 Guerra AB, Metainger SE, Bidros RS, et al. Breast reconstruction with gluteal artery perforator flaps: a critical analysis of 142 cases. Ann Plast Surg. 2004;52:118-125.
5 Heitmann C, Levine JL, Allen RJ. Gluteal artery perforator flaps. Clin Plast Surg. 2007;34:123-130.
6 Shaw WW. Superior gluteal free flap breast reconstruction. Clin Plast Surg. 1998;25:267-274.
7 Boustred AM, Nahai F. Inferior gluteal free flap breast reconstruction. Clin Plast Reconstr. 1998;25:275-282.
8 Allen RJ, Tucker C. Superior gluteal artery perforator free flap for breast reconstruction. Plast Reconstr Surg. 1995;95:1207-1212.
9 Koshima I, Moriguchi T, Soeda S, et al. The gluteal perforator-based flap for repair of sacral pressure sore. Plast Reconstr Surg. 1993;91:678.
10 Allen RJ. The superior gluteal artery perforator flap. Clin Plast Surg. 1998;25:293-302.
11 Allen RJ, Levine JL, Granzow JW. The in-the-crease inferior gluteal artery perforator flap for breast reconstruction. Plast Reconstr Surg. 2006;118:333-339.
12 Zenn M, Milard JA. Free inferior gluteal flap harvest with sparing of the posterior femoral cutaneous nerve. J Reconstr Microsurg. 2006;22:509-512.
13 Ahmadzadeh R, Bergeron L, Tang M, Morris SF. The superior and inferior gluteal artery perforator flaps. Plast Reconstr Surg. 2007;120:1551-1556.
14 Dupin CL, Allen RJ, Glass CA, et al. The internal mammary artery and vein as a recipient site for free flap breast reconstruction: a report of 110 consecutive cases. Plast Reconstr Surg. 1996;98(S):685-689.