CHAPTER 28 Glenohumeral Arthritis
Initially, arthroscopic management of shoulder arthritis was limited to diagnosis. The pioneering work of Ellman and colleagues1 and Cofield2 was primarily directed at differentiating arthritis from other shoulder diagnoses, especially in its early stages, where it is often radiographically silent. Treatment of these serendipitously identified lesions was limited to lavage and débridement, with little information as to functional outcomes. The outcome of arthroplasty, especially in younger individuals, has also been better defined. Although showing improvement, Sperling and associates3 have shown that half of all patients who have an arthroplasty for shoulder arthritis who are younger than 50 years have an unsatisfactory outcome, whether or not the glenoid is resurfaced. The poor outcomes and limited durability of arthroplasty in young individuals has led to renewed interest in nonarthroplasty treatment methods for glenohumeral arthritis, especially those techniques that can be performed arthroscopically. Arthroscopic débridement for arthritis now has reasonable midrange results reported, with significant information to relate to the prospective patient in regard to anticipated outcome. Although other techniques have also been reported, follow-up and detailed information about outcomes remain limited.
CLASSIFICATION
Arthritis of the shoulder has traditionally been classified into inflammatory or noninflammatory arthropathies (Table 28-1). Each diagnosis will have its unique presentations and difficulties. The primary unifying factor is the presence or absence of significant synovitis with the inflammatory arthropathies for which arthroscopic synovectomy is recommended. Recent peer-reviewed studies have shown significant benefit for synovectomy and arthroscopic treatment in patients with rheumatoid arthritis, although progression of disease is not universally halted, and maximal benefits were seen in patients with more modest radiographic changes.4 Conversely, synovectomy would rarely be indicated in noninflammatory arthropathy.
| Inflammatory | Noninflammatory |
|---|---|
| Rheumatoid arthritis | Primary osteoarthritis |
| Systemic lupus erythematosus | Posttraumatic osteoarthritis |
| Gout | Septic arthritis |
| Calcium pyrophosphate deposition | Postinstability arthritis |
| Psoriatic arthritis | Capsulorrhaphy arthropathy |
| Ankylosing spondylitis | Charcot arthritis |
Noninflammatory arthritis rarely presents with significant synovitis. Arthroscopic treatment for these conditions will vary depending on the associated findings and preference of the surgeon. The Outerbridge classification,5 developed for the knee, has been widely used to classify the extent of arthritic change in the shoulder (Table 28-2). Recent data have shown that the Outerbridge classification is of significant benefit in predicting the outcome of arthroscopic treatment of the shoulder. Radiographic classification is also of value. Although many classifications are available, that of Samilson and Prieto6 has been widely used to assess the outcome of arthroscopic treatment of the arthritic shoulder (Table 28-3). Chondrolysis has been a challenging problem that has been associated with thermal capsulorrhaphy and pain pumps with continuous infusion of local anesthetics. The cause of chondrolysis in general remains unclear; degeneration, inflammation or infection may play a role.7
TABLE 28-2 Glenohumeral Joint: Arthroscopic Grading Criteria
| Grade | Cartilage |
|---|---|
| I | Softening or blistering |
| II | Fissuring or fibrillation |
| III | Deep ulceration |
| IV | Exposed bone |
TABLE 28-3 Samilson Classification of Shoulder Arthritis
| Grade | Description |
|---|---|
| I | No changes |
| II | Mild arthrosis, osteophyte <3 mm |
| III | Moderate arthrosis, osteophyte 3- 7 mm, some joint space irregularity |
| IV | Severe arthrosis, osteophyte >7 mm, joint space narrowing, sclerosis |
From Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65:456-460.
PHYSICAL EXAMINATION
Findings for arthritis, especially in the early stages, can often be vague and nonspecific, as initially noted by Ellman and coworkers.1 Arthroscopy and synovial biopsy remain principal mechanisms of diagnosis for early arthritis of the inflammatory or degenerative type. Nonspecific deep tenderness, especially posteriorly, can be a clue. Pain at the extremes of motion may be present. The hallmark of later degenerative glenohumeral osteoarthritis is progressive loss of active and passive external rotation of motion. Crepitus is nonspecific, but can be present in inflammatory and noninflammatory arthritis. Warmth, redness, and swelling are nonspecific findings. Often, differential injections can be very useful. Patients with early glenohumeral arthritis will have a negative subacromial lidocaine impingement test but a positive response to intra-articular lidocaine injection.
DIAGNOSTIC IMAGING
Changes of early arthritis are often difficult to detect on plain radiographs, as reported early on by Ellman and colleagues.1 Later osteoarthritic changes such as joint space narrowing, posterior subluxation, and the common anteroinferior osteophyte described by many as the goat’s beard osteophyte. Inflammatory arthritis will rarely present with significant osteophytes. Periarticular erosions, however, are common, resulting from chronic synovitis, and vertical migration caused by associated rotator cuff damage can be seen. MRI scanning similarly can be negative in early disease, and standard MRI scanning with or without contrast will often miss significant articular cartilage injuries. The presence of a large effusion on an MRI scan can indicate an active arthritic process, especially if other obvious causes for the effusion are absent. Investigational MRI techniques may improve the accuracy of MRI for articular cartilage injuries.
TREATMENT OPTIONS
Nonoperative Treatment
Nonoperative treatment remains the mainstay of the management of the arthritic shoulder. Because all treatment would require permanent activity modification in the postoperative period, preoperative activity modification would seem to be in order. Heavy weightlifting, impact activities, and manual labor would at best be expected to eliminate the long-term benefit of any operative treatment, and honest counseling about reasonable activities with the arthritic shoulder is necessary. Anti-inflammatory medications can offer symptomatic relief. Gentle physiotherapy can bring significant improvement in range of motion. Steroid injection can also be of benefit in inflammatory and noninflammatory conditions. Viscosupplementation is not currently approved for the shoulder by the U.S. Food and Drug Administration (FDA) but has shown benefits in the knee, and might offer similar short-term benefits in the shoulder.8 Operative treatment should only be considered for those individuals who have failed nonoperative treatment.
Arthroscopic Techniques
Diagnostic Arthroscopy
Diagnostic arthroscopy for arthritis can be performed in the lateral decubitus or beach chair position, although our preference is for lateral decubitus position. Standard portal placement is usually adequate, although placement accuracy is even more important because of the constricted nature of the joint. Joints with extensive contractures will need releases anyway, and these releases should be performed sequentially early to allow safe evaluation of the entire joint to minimize risk of instrumentation and iatrogenic damage to the articular surfaces. Arthroscopic visualization and synovial biopsy can be the mainstay of diagnosis for many arthridites.
Débridement and Lavage
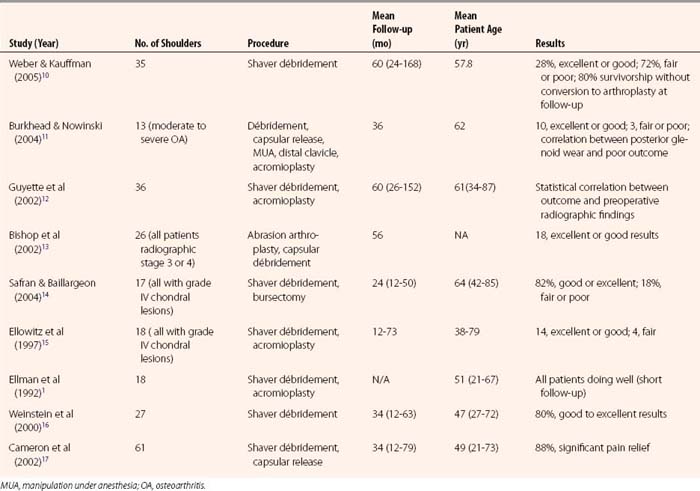
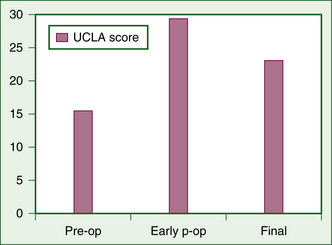
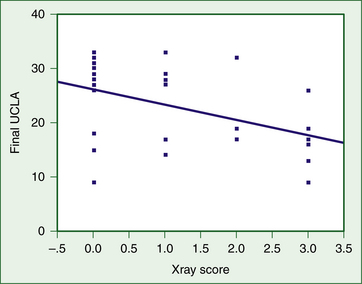
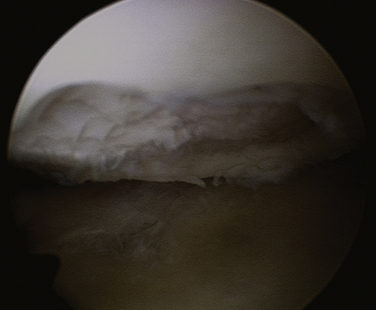
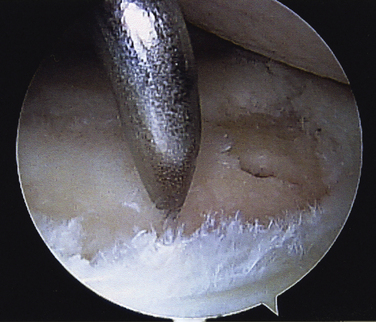
Débridement and lavage have been widely used in arthroscopic treatment of arthritis of the shoulder, much as with arthritis of the knee.9 Results are summarized in Table 28-4.1,10–17 Several of these studies now have follow-up of at least 60 months. Almost all studies have shown good short-term improvement with minimal complications; long-term results have been positive as well, but generally not as encouraging as the short-term results. In 1997, Norris and Green18 presented a series of failed arthroscopic débridements that has been widely quoted as emphasizing poor outcomes. This series, however, was limited to patients who presented to these surgeons with failed débridement requesting arthroplasty, and introduces a significant selection bias. Results of our study10 are summarized in Figures 28-1 to 28-3. Although the early results are encouraging, there is significant degradation of the results with longer term follow-up (see Fig. 28-1). The radiographic score based on the Samilson classification was highly correlated with function at final follow-up (see Fig. 28-2). Although the results tend to diminish with time, only 20% of the patients required arthroplasty at a mean follow-up of 60 months, indicating that débridement appears to be able to defer the need for arthroplasty in a large number of patients (see Fig. 28-3). This is not insignificant in view of the risk of precocious loosening of arthroplasty in younger individuals. Higher grade articular lesions and more severe radiographic changes are associated with inferior long-term results, consistent with similar treatment in the knee.9 Techniques vary among studies, but most involve lavage, mechanical smoothing of the articular surfaces, and removal of any loose bodies (Fig. 28-4). Capsular release to remove the standard internal rotation contracture has shown good results.19 This can be done to correct preoperative loss of motion. Release of the anterior capsule will improve external rotation, and posterior capsular release will improve internal rotation. Release is best done sequentially, checking the gains in motion with each sequential release until full motion is recovered. This prevents overrelease and potential instability. Some have suggested removal of the anteroinferior osteophyte,20 but the risk of iatrogenic injury to the axillary nerve has tempered the enthusiasm for this step. Glenoplasty to restore the glenoid to a concave configuration in patients in whom posterior subluxation has resulted in a biconcave glenoid has been discussed but is also controversial.21 Concomitant acromioplasty and acromioclavicular (AC) resection has been shown to provide good outcomes, despite the presence of arthritis.12,22 Recently, Kerr and McCarty23 have suggested that those patients with lesions of both the glenoid and humerus fare worse with débridement than those with unipolar lesions. Moderate improvement in symptoms and low complication rates favor the use of débridement and acromioplasty as the initial treatment in the management of mild to moderate glenohumeral arthritis. However, the older patient with Samilson grade III or IV changes on radiographs may be better managed with arthroplasty, because their results with arthroplasty tend to be superior to those in younger patients.
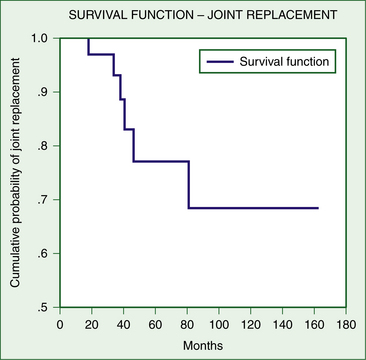
FIGURE 28-3 Survivorship curve—progression of débrided shoulders to total shoulder replacement at final follow-up.
(Weber SC, Kauffman JI: Arthroscopic débridement for glenohumeral osteoarthritis: long-term follow-up. Paper presented at: AAOS 72nd Annual Meeting; February 23-27, 2005; Washington, DC.)
Marrow Stimulation Techniques
The results of marrow stimulation techniques such as microfracture have shown favorable results in the knee, but remain largely anecdotal in the shoulder (Fig. 28-5). McCarty and Cole have offered an excellent summary of the data available.24 Microfracture has been described in the knee as an open procedure combined with a periosteal flap coverage. Results in this study were generally good; at mean 32-month follow-up, Constant scores increased significantly and osseous integration was proven in two second-look operations.25 It seems reasonable that microfracture of focal lesions of the humerus or glenoid would offer improved outcomes over simple débridement, but data to support this assertion are lacking.
Osteochondral Autograft Transfer
Osteochondral autograft transfer has shown good preliminary results in the shoulder, although donor site morbidity from the knee was the most significant complication. Humeral lesions are generally more amenable to osteochondral autograft transfer because of the ability to rotate the humerus to allow perpendicular access to the articular surface. Described as an open procedure by Schiebel and Bartl,26 there would be no reason that these procedures could not be performed arthroscopically, as in the knee. The role of osteochondral autograft transfer again is elusive, but probably would be limited to those patients with focal lesions who fail more traditional, established techniques, such as débridement.
Autogenous Chondrocyte Transfer
Autogenous chondrocyte transfer has been widely used in the knee to manage Outerbridge grade IV lesions. One might anticipate as good or better results in the shoulder, because weight-bearing would not be an issue. Although implantation is not an actual arthroscopic procedure, Romeo and associates27 have described the successful use of autogenous chondrocyte transfer in a patient with large lesions on the anterosuperior humerus created by chondrolysis secondary to thermal capsullorrhaphy. The lesions were exposed through a deltopectoral approach, and the periosteal graft was taken from the tibia.
Arthroscopic Interposition Arthroplasty
Preliminary results of interposition arthroplasty for the glenoid in association with prosthetic humeral resurfacing have been encouraging.28 These results have led to attempts to perform interposition arthroplasty without prosthetic replacement arthroscopically. Huijsmans and coworkers’29 preliminary study used an acellular allograft skin-derived collagen matrix. Of 11 patients, 6 had 90% improvement, with complete resolution of pain in the short term (8- to 20- month follow-up), 5 showed no improvement, and 1 was converted to a hemiarthroplasty. Similar results have been presented in the peer-reviewed literature with interposition arthroplasty using a lateral meniscus30 and also an acellular orthobiologic xenograft.31 Most of the studies had short-term follow-up, with limited outcome data. Clearly, the advantages of avoiding prosthetic replacement in the younger patient are significant, but long-term data on which to make recommendations to pursue these techniques is lacking, and the procedures are technically challenging. Complications in these series were minimal, however, and did not appear to complicate subsequent arthroplasty significantly if required.
PEARLS& PITFALLS
COMPLICATIONS
Complications of these procedures are those generic to arthroscopic interventions in general. Reported complications for débridement and lavage have been very low. More complicated procedures would be anticipated to have more complications. Interposition arthroplasty has the complications associated with the implanted material, whether it is xenograft or allograft, in terms of antigenicity and infection.
1. Ellman H, Harris E, Kay S Early degenerative joint disease simulating impingement syndrome: arthroscopic findings. Arthroscopy, 8; 1992:482-487.
2. Cofield RH. Arthroscopy of the shoulder. Mayo Clin Proc. 1983;58:501-508.
3. Sperling JW, Cofield RH, Rowland CM. Minimum 15-year follow-up of Neer hemiarthroplasty and total shoulder arthroplasty in patients 50 years and younger. J Bone Joint Surg Am. 1998;80:464-473.
4. Smith AM, Sperling JW, O’Droscoll SW, Cofield RH. Arthroscopic shoulder synovectomy in patient with rheumatoid arthritis. Arthroscopy. 2006;22:50-56.
5. Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43:752-757.
6. Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65:456-460.
7. Petty DH, Jazrawi LM, Estrada LS, Andrews JR Glenohumeral chondrolysis after shoulder arthroscopy: case reports and review of the literature. Am J Sports Med, 32; 2004:509-515.
8. Valiveti M, Reginato AJ, Falasca GF. Viscosupplementation for degenerative joint disease of shoulder and ankle. J Clin Rheumatol. 2006;12:162-163.
9. Aaron RK, Skolnick AH, Reinert SE. Arthroscopic débridement for osteoarthritis of the knee. J Bone Joint Surg. 2006;88:936-943.
10. Weber SC, Kauffman JI Arthroscopic débridement for glenohumeral osteoarthritis: long-term follow-up. Washington, DC: Weber SC, Kauffman JI; February 23-27, 2005 Paper presented at: AAOS 72nd Annual Meeting
11. Burkhead WZ, Nowinski RJ. Role of arthroscopy in treating glenohumeral arthritis. Washington, DC: Burkhead WZ, Nowinski RJ; February 2005. Paper presented at: AANA Specialty Day Meeting
12. Guyette TM, Bae H, Warren RF, et al. Results of arthroscopic subacromial decompression in patients with subacromial impingement and glenohumeral degenerative joint disease. J Shoulder Elbow Surg. 2002;11:299-304.
13. Bishop JY, Neviaser TJ, Neviaser RJ. Abrasion arthroplasty as a temporizing measure for the treatment of glenohumeral osteoarthritis. Dallas: Bishop JY, Neviaser TJ, Neviaser RJ; February 2002. Paper presented at: AAOS 69th Annual Meeting
14. Safran MR, Baillargeon D. The role of arthroscopy in the treatment of glenohumeral arthritis. Sports Med Arthros Rev. 2004;12:139-145.
15. Ellowitz AS, Rosas R, Quick DC, et al. The benefit of arthroscopic subacromial decompression for impingement in patients found to have unsuspected glenohumeral osteoarthritis. Orthop Trans. 1997;21:1135-1136.
16. Weinstein DM, Bucchieri JS, Pollock RG, et al. Arthroscopic débridement of the shoulder. Arthroscopy. 2000;16:471-476.
17. Cameron BD, Galatz LM, Ramsey ML, et al. Non-prosthetic management of grade IV osteochondral lesions of the glenohumeral joint. J Shoulder Elbow Surg. 2002;11:25-32.
18. Norris T, Green A. Arthroscopic treatment of glenohumeral osteoarthritis. Newport, RI: ASES; 1997. Paper presented at: 14th Annual Closed Meeting
19. Holloway, GB, Schenk T, Williams GR, et al. Arthroscopic capsular release for the treatment of refractory postoperative or post fracture shoulder stiffness. J Bone Joint Surg Am. 2001;83:1682-1687.
20. Andrews JR Arthroscopic débridement for glenohumeral arthritis Paper presented at: AAOS 67th Annual Meeting; Orlando, Fla. 2000.
21. O’Driscoll SW Arthroscopic glenoidplasty and osteocapsular arthroplasty for advanced glenohumeral osteoarthritis Paper presented at: AAOS 67th Annual Meeting; Orlando, Fla. 2000.
22. Simpson NS, Kelley JG. Extra-glenohumeral joint shoulder surgery in rheumatoid arthritis the role of bursectomy, acromioplasty, and distal clavicle excision. J Shoulder Elbow Surg. 1994;3:66-69.
23. Kerr BJ, McCarty EC. Outcome of arthroscopic débridement is worse for patients with glenohumeral arthritis of both sides of the joint. Clin Orthop Relat Res. 2008;466:634-638.
24. McCarty LPIII, Cole BJ. Nonarthroplasty treatment of glenohumeral cartilage lesions. Arthroscopy. 2005;21:1131-1142.
25. Siebold R, Lichtenberg S, Habermeyer P Combination of microfracture and periosteal flap for the treatment of focal full-thickness articular cartilage lesions of the shoulder: a prospective study. Knee Surg Sports Traumatol Arthrosc, 11; 2003:183-189.
26. Scheible M, Bartl C. Osteochondral autologous transplantation for the treatment of full-thickness articular cartilage defects of the shoulder. J Bone Joint Surg Br. 2004;86:991-997.
27. Romeo AA, Cole BJ, Mazocca AD, et al. Autologous chondrocyte repair of an articular defect in the humeral head. Arthroscopy. 2002;18:925-929.
28. Burkhead WZ, Hulton KS. Biologic resurfacing of the glenoid with hemiarthroplasty of the shoulder. J Shoulder Elbow Surg. 1995;4:263-270.
29. Huijsmans PE, McConnel L, Cresswell T, VanRooyan K The arthroscopic treatment of glenohumeral osteoarthritis in the young and active patient with arthroscopic resurfacing of the glenoid: preliminary results. Kiwa Maritana, South Africa: Huijsmans PE, McConnel L, Cresswell T, VanRooyan K; April, 2005 Paper presented at: South African Shoulder and Elbow Society
30. Pennington WT, Bartz BA Arthroscopic glenoid resurfacing with meniscal allograft: a minimally invasive alternative for treatment glenohumeral arthritis. Arthroscopy, 21; 2005:1517-1520.
31. Brislin KJ, Savoie FH, Field LD, Ramsey JR. Surgical treatment for glenohumeral arthritis in the young patient. Tech Shoulder Elbow Surg. 2004;5:165-169.