Chapter 59 Geriatric dermatology
| INTRINSIC AGING | EXTRINSIC AGING (PRIMARILY UV LIGHT) |
|---|---|
Morita A: Tobacco smoke causes premature skin aging, J Dermatol Sci 48:169–175, 2007.
Patterson WM, Fox MD, Schwartz RA: Favre-Racouchot disease, Int J Dermatol 43:167–169, 2004.
Farris PK: Combination therapy for solar lentigines, J Drugs Dermatol 3:S23–S26, 2004.
Superficial peel (stratum granulosum to superficial papillary dermis)
Key Points: Geriatric Dermatology
Curnier A, Choudhary S: Rhinophyma: dispelling the myths, Plast Reconstr Surg 114:351–354, 2004.

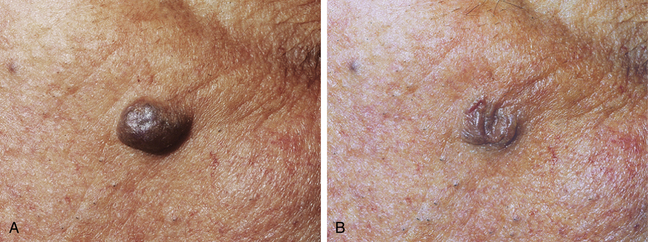
Figure 59-7. Typical stucco keratosis manifesting as small white or white-gray scaly papules with “stuck-on” appearance.
Ceylan C, Alper S, Kiline I: Leser-Trélat sign, Int J Dermatol 41:687–688, 2002.