Chapter 34 Geriatric care
The elderly come to emergency department for a wide variety of reasons. Their presentation will most commonly be due to an acute medical illness, but equally there will often not be an obvious ‘medical’ emergency, but simply a crisis. What the older patient in the emergency department needs, more than anything else, is for you to take a careful history, which includes speaking to family, carers, friends and local doctor. Always check that the patient’s own account of him/herself is accurate, by asking someone else who knows the patient (this will often save time, unnecessary investigations and costs). Always consider the possibility of underlying medical problems as the cause of the current presentation, especially when the initial triage suggests that the presenting problem is merely ‘social’. Often, the biggest dilemma is deciding whether or not the patient can safely be sent home (see the discharge checklist in Box 23.1, Chapter 23, ‘The ill patient’), especially for those patients with minor, undifferentiated illnesses or falls, whose initial investigations have not shown any significant abnormality. Mistakes are often made when these decisions are rushed and ill-informed, leading to poor outcomes for the patient, including readmission to hospital and increased morbidity and mortality.
The rapidly increasing population of older Australians is placing enormous pressures on all aspects of our healthcare system, especially emergency departments. Many changes in primary care and community care of the elderly have left patients and their carers with little option other than to call an ambulance in response to a crisis situation or illness. Numerous studies on the elderly in emergency departments have shown similar findings. Older persons come to hospital more often by ambulance, wait longer in the emergency department, have a much higher rate of admission to hospital, have increased mortality, undergo more investigations and cost more money to treat. They are at increased risk of further deterioration or readmission after discharge from the emergency department.
It should be assumed that the patient will not remember much of what he or she has been told during their visit to the emergency department. It is wise to take a paternalistic approach, similar to when dealing with paediatric patients, where extra time is spent explaining the medical issues to the patient’s family or carers. This is not meant to suggest that the majority of our older patients are mentally incompetent, but merely to stress the importance of good communication, especially in those situations where the older patient is dependent on a variety of coordinated community services to remain at home.
THE GERIATRIC SYNDROMES
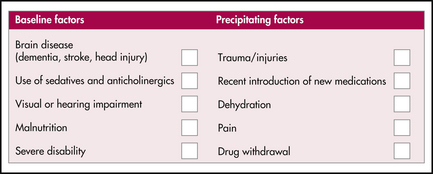
1 Acute confusion
Diagnosis
Management
2 Depression
Management
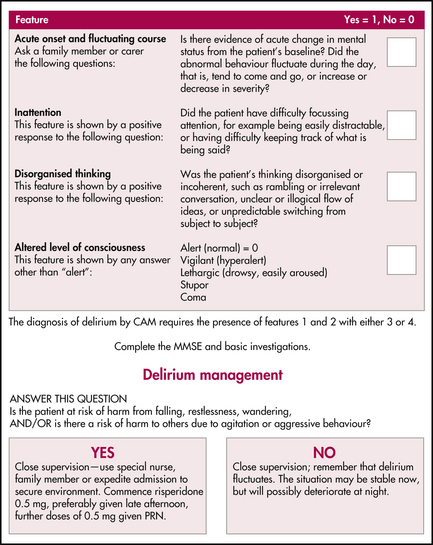
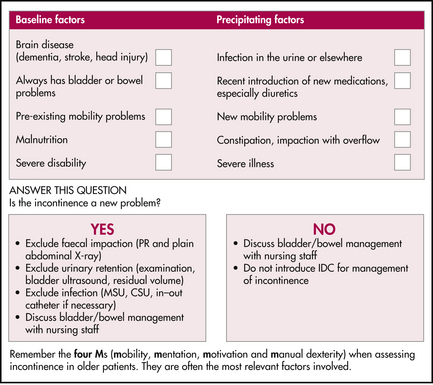
3 Falls
Elderly fallers are different from their healthy, age-matched counterparts. Although some have medical conditions that cause the fall, most have no single diagnosis, but rather a combination of risk factors for falls. The more risk factors present, the greater the likelihood of further falls. Interventions targeted at these risk factors have been shown to reduce the rate of further falls.
Management
4 Immobility
Mobility problems are a common link in those patients who have a number of the geriatric syndromes (incontinence, falls and dependency) and are often overlooked by young doctors. It is important to determine if the immobility is an acute or chronic problem and train yourself to comment on the gait. Is it safe or unsafe? Mobility is affected by falls (pain from fractures or soft tissue injury, fear of further falling, lack of confidence), and intercurrent illness (breathlessness, muscle weakness, dizziness, fear) in the acute setting. A brief period of gait retraining is often all that is required to restore confidence and safety, and is a good reason in itself to recommend admission to hospital. Those with long-standing mobility problems may need a much more intensive multidisciplinary team approach to get home, and should be referred to the geriatric service for assessment. The screening tool for immobility is the same as the falls risk assessment, and the time to ‘Up and Go’ test (Box 34.3) is a simple objective measure of gait that you could perform, although such tests have not been shown to accurately predict outcomes after discharge from the emergency department.
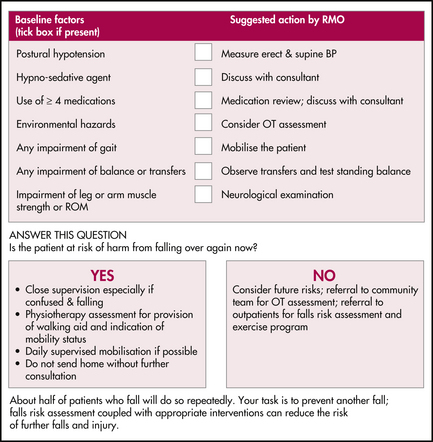
5 Incontinence
Initial assessment of incontinence
Diagnosis and management
6 Dependency in activities of daily living (ADLs)
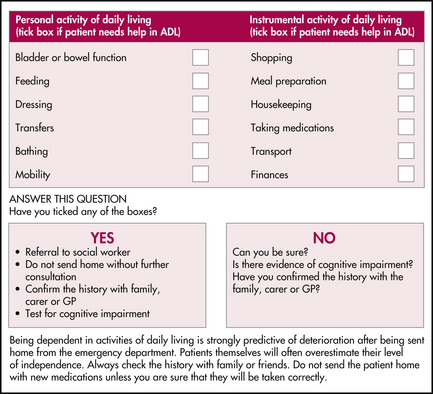
You should be very wary of the frail elderly patient whose triage assessment lists social factors, ‘not coping’ or ‘acopia’ as the main presenting problem. Such patients commonly have a combination of identifiable medical conditions that are collectively responsible for their current inability to manage their activities of daily living (ADLs), and appropriate medical treatments often improve these patients to the point where they can continue to cope at home. This is often the aim of a geriatric admission to hospital. What may initially present as a simple case of ‘not coping’ will often result in weeks of hospitalisation with the patient eventually returning home. Obviously, this is not a role for the emergency department. Nonetheless, you should become familiar with a brief assessment of ADLs (Figure 34.5). This should become part of your routine medical assessment because being dependent in basic ADLs is a powerful predictor of poor health outcomes from acute illness.
Involvement of the emergency department social worker is important in the early stages, especially if you are sending the patient directly home. Many emergency departments now have specific aged care teams available to help coordinate services on discharge. Your patient may temporarily need services to cope once they go home, but do not assume that appropriate services can be arranged immediately (especially after hours and on weekends).
1 Creasey H. Acute confusion in the elderly. Current Therapeutics. Aug 1996:21-27.
2 Inouye S.K., van Dyck C.H., Alessi C.A., et al. Clarifying confusion: the Confusion Assessment Method; a new method for detection of delirium. Ann Intern Med. 1990;113:941-948.
3 Folstein M.F., Folstein S.E., McHugh P.R. The Mini-Mental State Examination: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189-198.
4 Yesavage J., Brink T., Rose T., et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiat Res. 1983;17:37-49.
5 Tinetti M.E., Speechley M., Ginter S.F. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701-1707.
6 Podsialdo D., Richardson S. The time to ‘Up &Go’: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142-148.
Aminzadeh F., Dalziel W. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39:238-247.
Gray L., Woodward M., Scholes R., Fonda D. Geriatric medicine: a pocket guide for doctors, health professionals and students. Port Melbourne: Ausmed Publications; 1994.
Resnick N., Marcantonio E. How should clinical care of the aged differ? Lancet. 1997;350(9085):1157-1158.