Genitourinary Tract Disorders
In the wilderness, genitourinary tract disorders are common, and urinary tract infections (UTIs) constitute the majority of complaints. Also included in this chapter are pyelonephritis, urethritis, epididymitis, prostatitis, testicular torsion, urinary tract obstruction, and acute urinary retention. Gynecologic infections and emergencies are discussed in chapter 31.
Urinary Tract Infection
1. UTIs are more common in women.
2. The incidence increases in postmenopausal women and women with histories of recent frequent sexual intercourse.
3. In women the primary cause of UTI is invasion of the urinary tract by bacteria that have ascended the urethra from the introitus.
4. Most of these infections are caused by gram-negative aerobic bacteria, most often Escherichia coli.
5. UTIs are rare entities in men younger than 50 years.
6. Despite the difference in prevalence, symptoms in men and women are similar.
7. Infection of the urinary tract in a male is often associated with prostatic enlargement or infection.
Lower UTI (Uncomplicated UTI)
1. Pyelonephritis associated with chills and fever
2. Urethritis (more probable in sexually active persons with multiple or new partners)
3. Chlamydial or gonococcal cervicitis (often associated with cervical discharge)
4. Vaginal infection (associated with vaginal discharge, external irritation, or pain with intercourse)
5. Ureterolithiasis (dysuria with flank pain, restlessness, and costovertebral angle [CVA] tenderness suggests urinary tract stone[s])
Treatment
1. Perform a physical examination, including determination of temperature, abdominal examination, and assessment for CVA tenderness.
2. Perform a pelvic (bimanual) examination in a woman whose symptoms are associated with pelvic pain or vaginal bleeding. Although a formal pelvic examination using a speculum with the individual in a lithotomy position is virtually impossible in the wilderness, a simple bimanual examination might identify an adnexal or uterine process (e.g., ectopic pregnancy, pelvic inflammatory disease). Perform a pregnancy test.
3. Give oral antibiotic therapy using one of the following:
a. Trimethoprim/sulfamethoxazole one double-strength (DS, 160/800 mg) tablet bid for 3 days
b. Ciprofloxacin 500 mg bid for 3 days
c. Nitrofurantoin 100 mg bid for 5 days is a safe option for pregnant women
4. If symptoms persist after standard therapy:
5. In addition to the antibiotic therapy, provide pain relief for dysuria by administering phenazopyridine (a urinary anesthetic) 200 mg PO tid for a maximum of 2 days. Warn the patient that the urine (and possibly contact lenses) will turn orange.
Pyelonephritis
Treatment
1. Administer an oral antibiotic if the patient is nonpregnant and immunocompetent and can tolerate oral medication.
a. Reasonable antibiotic choices include ciprofloxacin 500 mg bid or levofloxacin 750 mg daily for 10 to 14 days.
2. For a severely ill, immunocompromised, or pregnant patient, initiate therapy with a parenteral antibiotic such as a third-generation cephalosporin (ceftriaxone 1 g IM or IV daily).
4. When a high fever is present:
a. Routinely administer acetaminophen 500 mg q4h or ibuprofen 600 mg q6h to make the patient more comfortable.
b. If the fever persists, consider the possibility of a resistant organism, UTI, or abscess.
5. Arrange for evacuation of immunocompromised or pregnant patients, when protracted vomiting makes oral therapy impossible, or when generalized toxicity (volume depletion, fever greater than 38.9° C [102° F] or marked CVA tenderness) is present.
6. Instruct patients to seek medical follow-up on return, even if symptoms resolve fully.
Urinary Stones
1. Location of pain depends on the site of stone impaction, but most patients complain of flank pain
a. Pain may radiate to the groin as the stone migrates distally
b. Consider other causes for pain: acute aortic dissection, back strain, or herniated lumbar disk
3. Restlessness and inability to lie still
5. Absence of peritoneal signs; if these develop, they indicate a possible intraperitoneal process (e.g., appendicitis)
6. Absence of fever unless an associated UTI is present (which may develop in an obstructed ureter)
7. Gross hematuria possible, but microscopic hematuria is more likely
Treatment
1. Consider evacuation for severe nausea and vomiting (inadequate oral intake), fever (suggestive of an infection proximal to the obstruction), or the presence of an intraperitoneal process.
2. Arrange for adequate hydration to help move the stone.
3. Although not usually practical in the wilderness, filtering the urine for stones is helpful for diagnosis.
4. Administer an antiinflammatory medication such as ketorolac (Toradol) 60 mg IM or 30 mg IV q8h, or an oral nonsteroidal antiinflammatory drug (NSAID) such as ibuprofen 600 mg q6h, to reduce the pain of renal colic. NSAIDs may be used in addition to narcotic analgesia.
5. Administer a narcotic analgesic if needed.
a. Use an oral narcotic combination drug such as hydrocodone bitartrate 5 mg with acetaminophen 325 mg, one or two tablets q4-6h.
b. For more severe pain, administer a parenteral narcotic such as morphine sulfate 2 to 5 mg IV q5min, titrated for pain relief. Make sure to monitor the patient for excessive sedation manifested by hypoventilation, and have naloxone 0.4 mg IV available for emergency administration.
6. For additional narcotic analgesic options, see Chapter 24.
7. Administer an antiemetic drug (ondansetron 4–8 mg oral dissolving tablet q6h) if nausea and vomiting develop.
8. Encourage the patient to seek medical follow-up even if symptoms resolve fully.
Epididymitis
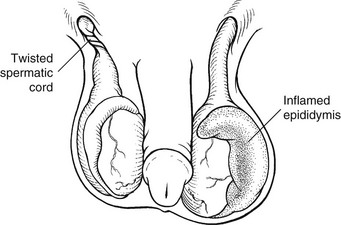
Epididymitis is abrupt inflammation of the epididymis that spreads rapidly and can appear as generalized inflammation of the entire hemiscrotum (Fig. 30-1). The differential diagnosis includes torsion of the testis, acute orchitis, or tumor of the testis with hemorrhage or hydrocele. Most cases of epididymitis in young men are caused by Chlamydia trachomatis. At any age, UTI caused by gram-negative rods can spread to the epididymis.
Signs and Symptoms
1. Acute scrotal pain in men older than age 20 years (infectious epididymitis)
2. Testicular torsion in men (usually) younger than age 30 years
3. Gradual (over days) onset of pain
4. Dysuria or urethral discharge
5. Normal urinalysis in torsion, but pyuria in epididymitis (if urinalysis can be done)
8. Tenderness and swelling localized to one epididymis (usually at the superior pole of the testis)
9. Prehn’s sign: relief of pain when elevating the testis (suggestive of epididymitis rather than torsion)
Treatment
1. Administer an antibiotic that covers Neisseria gonorrhoeae and C. trachomatis.
2. Allow the patient to rest supine with the scrotum elevated.
3. Administer analgesic medication.
4. Arrange for the patient to wear men’s supportive briefs or an athletic supporter to offer pain relief if the patient is expected to ambulate.
5. Be aware that relief after therapy usually occurs within 24 hours.
6. Inform the patient that induration and edema in the region of the epididymis may persist for 6 to 8 weeks.
Testicular Torsion
1. Rare in males older than 30 years
2. May or may not occur during physical exertion
4. No preceding urethral discharge or fever
5. Testis that rides high in the upper part of the scrotum
6. Relief of pain when the affected testis is elevated (Prehn’s sign) is suggestive of epididymitis rather than torsion, but this is not absolute (see Fig. 30-1)
Treatment
1. Be aware that testicular torsion of the spermatic cord requires surgical intervention. Therefore consider immediate evacuation if this diagnosis is suspected.
a. Torsion most often occurs with the anterior portion of the testis rotating from its lateral aspect to its medial aspect.
b. To correct the torsion manually, attempt to turn the right testis clockwise and the left testis counterclockwise, when viewed from above.
c. Be aware that extreme tenderness may make manual correction difficult.
3. Advise the patient that evaluation by a urologist is indicated after successful detorsion.
4. Be aware that if the torsion is not corrected, loss of the affected testis is likely.
Acute Bacterial Prostatitis
Treatment
1. Initiate oral antibiotic treatment with a fluoroquinolone, such as ciprofloxacin 500 mg bid or levofloxacin 500 mg daily.
2. Alternatively, administer ampicillin 500 mg PO qid.
3. Alternatively, administer trimethoprim/sulfamethoxazole one 160/800 mg (DS) tablet PO bid.
4. Continue therapy for at least 28 days.
5. If urinary retention is present, catheterization or suprapubic aspiration may be necessary.
Acute Urinary Retention
Treatment
1. Tamsulosin 0.4 mg daily is a third-generation α-blocker that may provide some relief by promoting bladder neck and prostatic urethral relaxation.
2. Bladder decompression should be initially attempted with a standard Foley catheter.
3. In men with prostatic hypertrophy, passage of the catheter may be challenging, and a large catheter or coudé catheter should be used if a standard Foley catheter cannot be passed.
4. Instrumentation of the urethra with hemostats or dilators is dangerous and should not be attempted in the field.
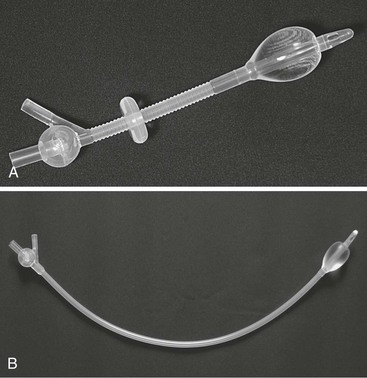
5. OPTION-vf (Fig. 30-2, A) and OPTION-vm (Fig. 30-2, B) catheters are valved urinary catheters that eliminate the need for urine drainage bags and connecting tubes normally required with Foley catheters. These catheters incorporate a manually activated valve at the end of the catheter that allows the patient to store urine in the bladder and to mimic normal voiding behavior. The catheters may be used with a continuous drainage adapter when appropriate so that a bag may be placed and urination rate and volume assessed.