Genitourinary System
ICD-10-CM Example from Tabular
N30 Cystitis
Use additional code to identify infectious agent (B95-B97)
Excludes1 prostatocystitis (N41.3)
Urinary System
Anatomy and Physiology
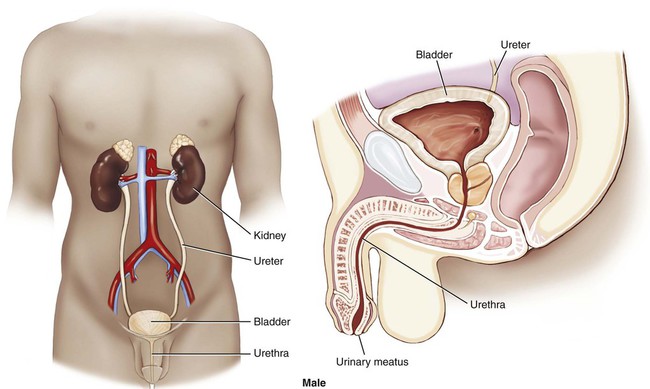
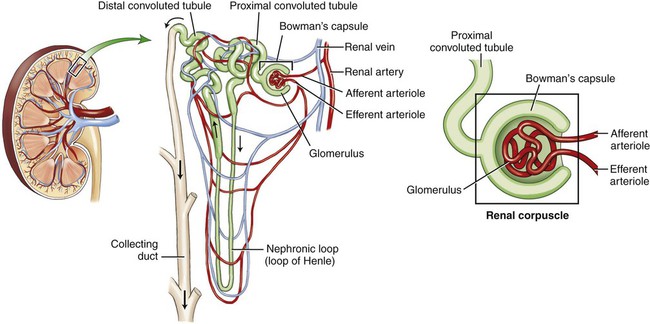
The urinary system is composed of two kidneys, two ureters, a urinary bladder, and a urethra (Figs. 6-1 and 6-2). The work of the urinary system is done by a specialized tissue in the kidneys called parenchymal tissue. The kidneys function to filter the blood and eliminate waste through the passage of urine. The ureters are thin, muscular tubes that move urine in peristaltic waves from the kidneys to the bladder. The urinary bladder is the sac that stores the urine until it is excreted. The bladder is lined with an epithelial mucous membrane of transitional cells. Underneath, a layer termed the lamina propria is composed of connective tissue that holds the blood vessels and nerves. The detrusor muscle is the final coat; it normally contracts to expel urine. The urethra is the tube that conducts the urine out of the bladder. The opening of the urethra is called the urinary meatus. The triangular area in the bladder between the ureters’ entrance and the urethral outlet is called the trigone. The ureters, bladder, and urethra are all stromal tissue, which is a supportive tissue.
The Kidney
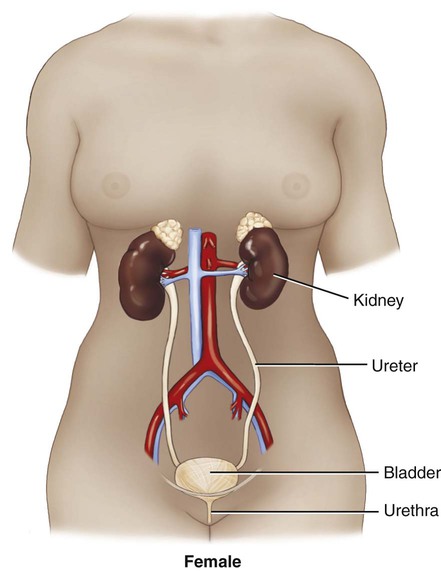
Because the kidneys are primarily responsible for the functioning of the urinary system, it is helpful to look at them in greater detail. Each of the two kidneys is located high in the abdominal cavity, tucked under the ribs in the back and behind the lining of the abdominal cavity (retroperitoneal). The normal human kidney is about the size of a fist. The tough outer covering of the kidney is the renal capsule. If a kidney were sliced open, the outer portion, the cortex (pl. cortices), and the inner portion, called the medulla (pl. medullae), would be visible (Fig. 6-3). The renal pelvis and calyces (sing. calyx) are an extension of the ureter inside the kidney. The renal pyramids are triangular sections that extend from the renal medulla toward the renal pelvis. The downward point of the pyramid is referred to as the papilla. The term renal means “pertaining to the kidneys.” The ureteropelvic junction (UPJ) is the area where the ureter joins the renal pelvis. It is a common site of obstruction of the outward flow of urine from the kidney.
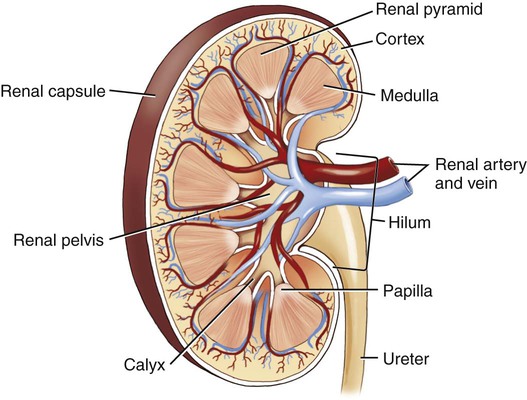
The hilum (pl. hila) is the location on the kidney where the ureter and renal vein leave the kidney and the renal artery enters. The cortex contains tissue with millions of microscopic units called nephrons (Fig. 6-4). Here in the tiny nephrons, blood passes through a continuous system of urinary filtration, reabsorption, and secretion that measures, monitors, and adjusts the levels of substances in the extracellular fluid.
14. transurethral ____________________________________________________________________________________
15. paranephric _____________________________________________________________________________________
16. retroperitoneal __________________________________________________________________________________
17. suprarenal ______________________________________________________________________________________
18. perivesical ______________________________________________________________________________________
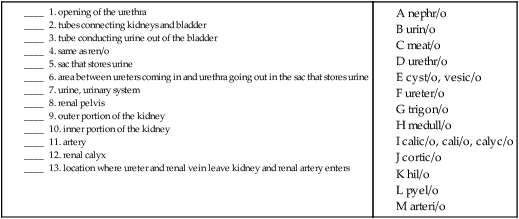
Combining Forms for the Anatomy of the Urinary System
| Meaning | Combining Form |
| artery | arteri/o |
| bladder | cyst/o, vesic/o |
| calyx | calic/o, cali/o, calyc/o |
| cell | cellul/o |
| cortex | cortic/o |
| glomerulus | glomerul/o |
| hilum | hil/o |
| kidney | nephr/o, ren/o |
| meatus | meat/o |
| medulla | medull/o |
| parenchyma | parenchym/o |
| peritoneum | peritone/o |
| renal pelvis | pyel/o |
| stroma | strom/o |
| trigone | trigon/o |
| ureter | ureter/o |
| urethra | urethr/o |
| urine, urinary system | urin/o, ur/o |
Prefixes for the Anatomy of the Urinary System
| Prefix | Meaning |
| extra- | outside |
| en- | in |
| par- | beside, near |
| retro- | backward |
Suffixes for the Anatomy of the Urinary System
| Suffix | Meaning |
| -al, -ar, -ic | pertaining to |
| -ation, -ion | process of |
Pathology
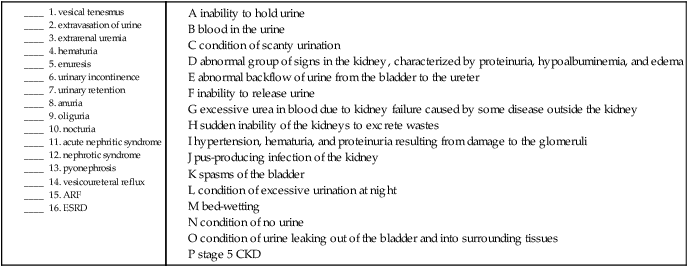
Terms Related to Symptoms and Signs Involving the Genitourinary System (R3Ø-R39)
| Term | Word Origin | Definition |
| anuria | an- without -uria urinary condition |
Condition of no urine. |
| dysuria | dys- painful, abnormal -uria urinary condition |
Condition of painful urination. |
| enuresis | en- in ur/o urine -esis state of |
Also commonly known as “bed-wetting,” enuresis can be nocturnal (at night) or diurnal (during the day). |
| extrarenal uremia | extra- outside ren/o kidney -al pertaining to ur/o urine -emia blood condition |
Excessive urea in blood (uremia) due to kidney failure caused by disease outside of the kidney (e.g., congestive heart failure). |
| extravasation of urine | extra- outside vas/o vessel -ation process of |
Condition of urine leaking outside of the bladder and into surrounding tissues. May be due to trauma or a stone. |
| hematuria | hemat/o blood -uria urinary condition |
Blood in the urine. |
| incontinence, urinary | Inability to hold urine. | |
| nocturia | noct/i night -uria urinary condition |
Condition of excessive urination at night. |
| oliguria | olig/o scanty, few -uria urinary condition |
Condition of scanty urination. |
| polyuria | poly- excessive, frequent -uria urinary condition |
Condition of excessive urination. |
| retention, urinary | Inability to release urine. | |
| vesical tenesmus | vesic/o bladder -al pertaining to |
Bladder spasms. |
Terms Related to Glomerular Diseases (NØØ-NØ8)
| Term | Word Origins | Definition |
| acute nephritic syndrome | nephr/o kidney -itic pertaining to |
Hypertension, hematuria, and proteinuria (protein in the urine) resulting from damage to the glomeruli. |
| nephrotic syndrome | nephr/o kidney -tic pertaining to |
Abnormal group of signs in the kidney, characterized by proteinuria, hypoalbuminemia (abnormally low levels of albumin in the blood), and edema; may occur in glomerular disease and as a complication of many systemic diseases (e.g., diabetes mellitus). Also called nephrosis. |
Terms Related to Renal Tubulo-interstitial Diseases (N1Ø-N16)
| Term | Word Origin | Definition |
| hydronephrosis | hydr/o water nephr/o kidney -osis abnormal condition |
Dilation of the renal pelvis and calices of one or both kidneys resulting from obstruction of the flow of urine. |
| pyelonephritis | pyel/o renal pelvis nephr/o kidney -itis inflammation |
Bacterial or viral infection of the kidneys and renal pelvis. |
| pyonephrosis | py/o pus nephr/o kidney -osis abnormal condition |
Pyogenic (pus-producing) infection of the kidney. |
| vesicoureteral reflux | vesic/o urinary bladder ureter/o ureter -al pertaining to re- back -flux flow |
Abnormal backflow of urine from the bladder to the ureter. |
Terms Related to Acute Kidney Failure and Chronic Kidney Failure (N17-N19)
| Term | Word Origin | Definition |
| renal failure | ren/o kidney -al pertaining to |
Inability of the kidneys to excrete wastes, concentrate urine, and conserve electrolytes. May be acute or chronic. |
| acute renal failure (ARF) | Sudden inability of the kidneys to excrete wastes, resulting from hemorrhage, trauma, burns, toxic injury to the kidney, pyelonephritis or glomerulonephritis, or lower urinary tract obstruction. Characterized by oliguria and rapid azotemia. | |
| chronic kidney disease (CKD) (formerly chronic renal failure) | CKD is measured in stages of increasing severity, from 1 (mild damage with a normal glomerular filtration rate) to 5 (complete kidney failure requiring either dialysis or a renal transplant). Stage 5 is also called end-stage renal disease (ESRD) and is the most extreme form of CKD. |
17. painful urinary condition ________________________________________________________________________
18. excessive (frequent) urinary condition ____________________________________________________________
19. abnormal condition of water in the kidney _______________________________________________________
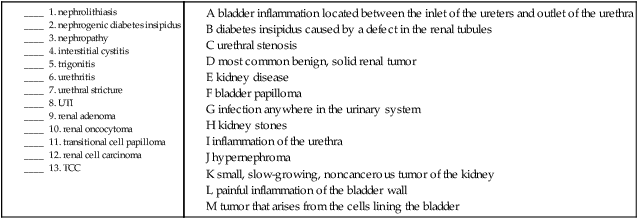
Terms Related to Urolithiasis (N2Ø-N23)
| Term | Word Origin | Definition |
| urolithiasis | ur/o urine, urinary system lith/o stone -iasis condition, presence of |
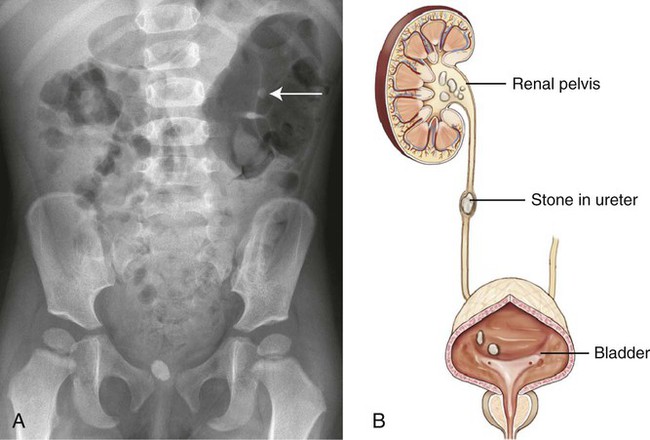
Stones (calculi) anywhere in the urinary tract, but usually in the renal pelvis or urinary bladder. Depending on where the stone is located, the term is nephrolithiasis (kidney), ureterolithiasis (ureter), cystolithiasis (urinary bladder), or urethrolithiasis (urethra). Usually formed in patients with an excess of the mineral calcium. Also called urinary calculi (Fig. 6-5). |
Terms Related to Other Disorders of the Kidney and Ureter (N25-N29)
| Term | Word Origin | Definition |
| nephrogenic diabetes insipidus | nephr/o kidney -genic pertaining to producing |
Diabetes insipidus caused by a defect in the renal tubules causing them to be unresponsive to antidiuretic hormone (ADH). |
| nephropathy | nephr/o kidney -pathy disease process |
Disease of the kidneys; a general term that does not specify a disorder. |
| nephroptosis | nephr/o kidney -ptosis drooping, sagging |
Prolapse or sagging of the kidney. |
Terms Related to Other Diseases of the Urinary System (N3Ø-N39)
| Term | Word Origin | Definition |
| cystitis | cyst/o bladder -itis inflammation |
Inflammation of the urinary bladder. |
| interstitial cystitis (IC) | inter- between stiti/o space -al pertaining to cyst/o bladder -itis inflammation |
A painful inflammation of the wall of the bladder. Symptoms include urinary frequency and urgency. |
| trigonitis | trigon/o trigone -itis inflammation |
Inflammation of the bladder between the inlet of the ureters and outlet of the urethra. |
| urethral stricture | urethr/o urethra -al pertaining to |
Narrowing of the urethra. Also called urethral stenosis. |
| urethritis | urethr/o urethra -itis inflammation |
Inflammation of the urethra. |
| urinary tract infection (UTI) | urin/o urine, urinary system | Infection anywhere in the urinary system, caused most commonly by bacteria, but also by parasites, yeast, and protozoa (sing. protozoon). Most frequently occurring disorder in the urinary system. |
Terms Related to Benign Neoplasms (D3Ø and D41)
| Term | Word Origin | Definition |
| renal adenoma | ren/o kidney -al pertaining to aden/o gland -oma tumor, mass |
Small, slow-growing, glandular, noncancerous tumors of the kidney, usually found at autopsy. |
| renal oncocytoma | onc/o tumor cyt/o cell -oma tumor, mass |
The most common benign solid renal tumor. |
| transitional cell papilloma | papill/o nipple -oma tumor, mass |
Also referred to as bladder papilloma. Although this type of tumor is benign when found, recurrences are occasionally malignant. |
Terms Related to Malignant Neoplasms (C64-C68)
| Term | Word Origin | Definition |
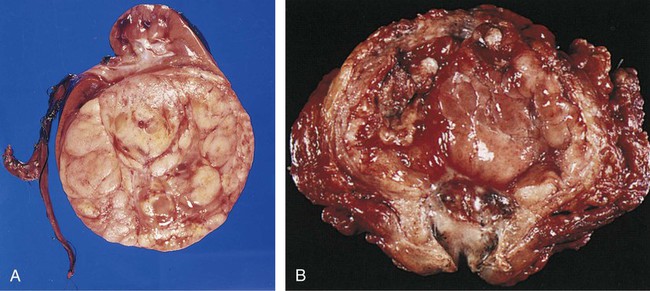
| nephroblastoma | nephr/o kidney blast/o embryonic -oma tumor |
Also called Wilms’ tumor, these tumors develop from kidney cells that did not develop fully before a child’s birth. These cancerous tumors of the kidney occur mainly in children (Fig. 6-6, A). |
| renal cell carcinoma | ren/o kidney -al pertaining to carcinoma cancerous tumor of epithelial origin |
Also referred to as hypernephroma or adenocarcinoma of the kidney, this is one of the most common cancers. Although the cause is unknown, risk factors include smoking and obesity. |
| transitional cell carcinoma (TCC) of the bladder | carcinoma cancerous tumor of epithelial origin | These malignant tumors account for approximately 90% of all bladder cancers and arise from the cells lining the bladder (Fig. 6-6, B). |
14. nephroptosis ____________________________________________________________________________________
15. cystitis _________________________________________________________________________________________
16. nephroblastoma _________________________________________________________________________________
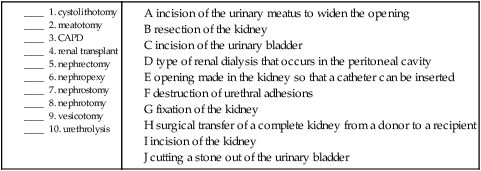
Procedures
| Term | Word Origin | Definition |
| cystectomy | cyst/o bladder -ectomy cutting out |
Cutting out part or all of the urinary bladder. |
| cystolithotomy | cyst/o bladder -lithotomy cutting out a stone |
Incision to cut a stone out of the urinary bladder. |
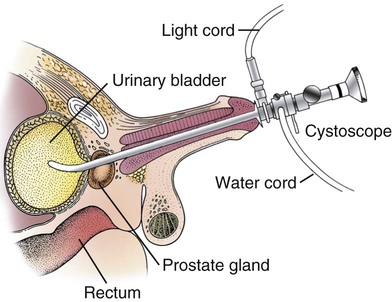
| cystoscopy | cyst/o bladder -scopy viewing |
Visual examination of the urinary bladder using a cystoscope (Fig. 6-7). |
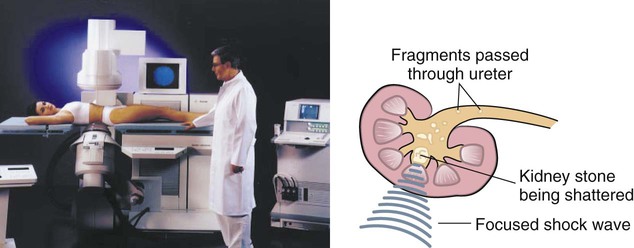
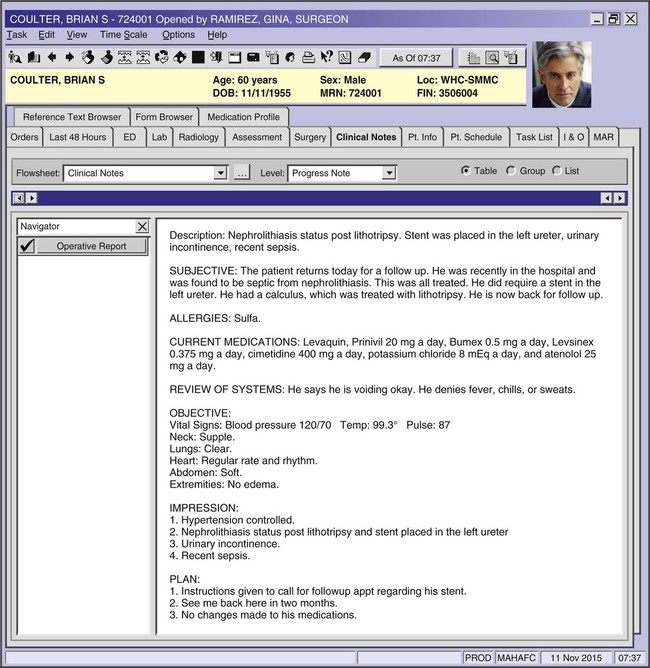
| lithotripsy | lith/o stone -tripsy crushing |
Process of crushing stones either to prevent or clear an obstruction in the urinary system; crushing may be done manually, by high-energy shock waves, or by pulsed dye laser. In each case, the fragments may be expelled naturally or washed out (Fig. 6-8). Use of shock waves is termed extracorporeal shock wave lithotripsy (ESWL). |
| meatotomy | meat/o meatus -tomy cutting |
Incision of the urinary meatus to widen the opening. |
| nephrectomy | nephr/o kidney -ectomy cutting out |
Resection of the kidney. |
| nephrolithotomy | nephr/o kidney -lithotomy cutting out a stone |
Incision of the kidney for removal of a kidney stone. |
| nephropexy | nephr/o kidney -pexy suspension |
Suspension or fixation of the kidney. |
| nephrostomy | nephr/o kidney -stomy making a new opening |
Opening made in the kidney so that a catheter can be inserted. |
| nephrotomy | nephr/o kidney -tomy cutting |
Incision of the kidney. |
| pyeloplasty | pyel/o renal pelvis -plasty surgically forming |
Surgical operation to repair a blockage between the renal pelvis and a ureter. |
| renal dialysis | ren/o kidney -al pertaining to dia- through, complete -lysis breaking down |
Process of diffusing blood across a semipermeable membrane to remove substances that a healthy kidney would eliminate, including poisons, drugs, urea, uric acid, and creatinine. |
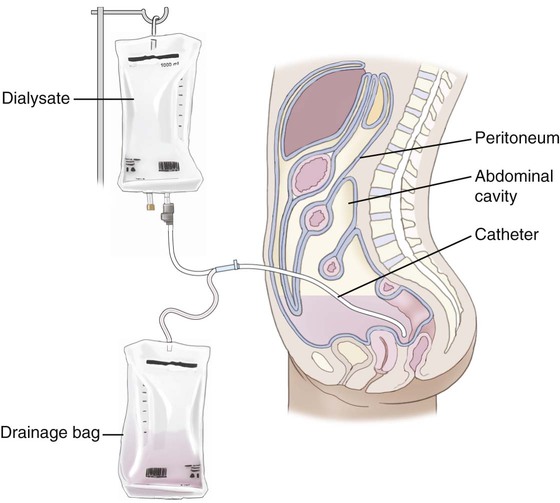
| continuous ambulatory peritoneal dialysis (CAPD) | peritone/o peritoneum -al pertaining to dia- through, complete -lysis breaking down |
Type of renal dialysis in which an indwelling catheter in the abdomen permits fluid to drain into and out of the peritoneal cavity to cleanse the blood (Fig. 6-9). |
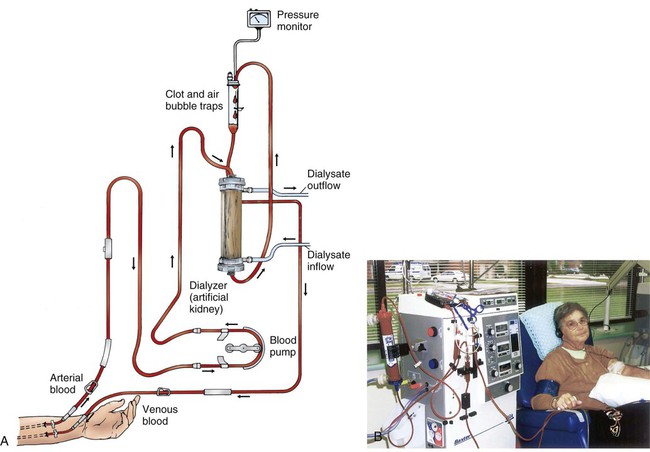
| hemodialysis (HD) | hem/o blood dia- through, complete -lysis breaking down |
Type of renal dialysis that cleanses the blood by shunting it from the body through a machine for diffusion and ultrafiltration and then returning it to the patient’s circulation (Fig. 6-10). |
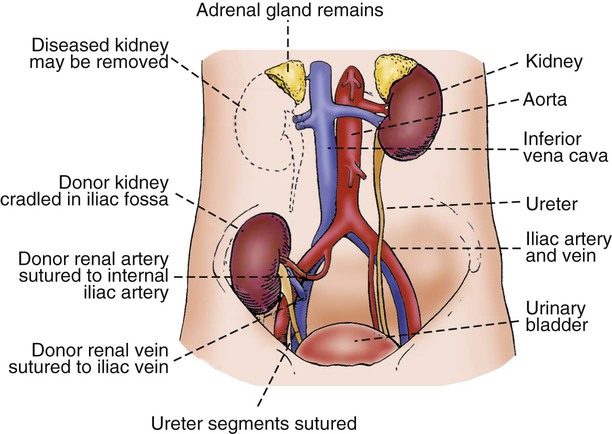
| renal transplant | ren/o kidney -al pertaining to trans- across |
Surgical transfer of a complete kidney from a donor to a recipient (Fig. 6-11). |
| urethrolysis | urethr/o urethra -lysis breaking down |
Destruction of adhesions of the urethra. |
| urinalysis (UA) | urin/o urinary system, urine –lysis breaking down |
The physical, chemical, and/or microscopic examination of urine. |
| blood urea nitrogen (BUN) | Blood test that measures the amount of nitrogenous waste in the circulatory system; an increased level is an indicator of kidney dysfunction. | |
| creatinine clearance test | Test of kidney function that measures the rate at which nitrogenous waste is removed from the blood by comparing its concentration in the blood and urine over a 24-hour period. | |
| glomerular filtration rate (GFR) | The amount of blood that is filtered by the glomeruli of the kidneys. This rate is decreased when the kidneys are dysfunctional. | |
| vesicotomy | vesic/o bladder -tomy cutting |
Incision of the urinary bladder. |
11. cutting out the bladder __________________________________________________________________________
12. complete breaking down of the blood ____________________________________________________________
13. removing a kidney stone ________________________________________________________________________
14. crushing a stone ________________________________________________________________________________
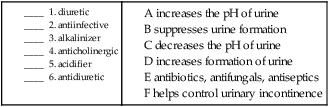
Pharmacology
urinary pH modifiers: Increase (acidifiers) or decrease (alkalinizers) the pH of the urine to prevent kidney stones, treat acidosis, or promote excretion of some drugs and toxins. Examples of acidifiers include methionine and ammonium chloride, but are more commonly used in animals. Examples of alkalinizers include sodium bicarbonate (Neut) and potassium citrate (Urocit-K).
anticholinergics: Help control urinary incontinence by delaying the urge to void, increasing the bladder capacity, and relaxing the bladder muscles. Examples include tolterodine (Detrol), darifenacin (Enablex), and oxybutynin (Ditropan).
antidiuretics: Suppress urine formation. Examples include vasopressin (also known as antidiuretic hormone, ADH) and desmopressin (DDAVP).
antiinfectives: Fight infection in the urinary system, such as antibiotics, antiseptics, or antifungals. Nitrofurantoin (Macrobid), sulfamethoxazole-trimethoprim (Septra, Bactrim), and levofloxacin (Levaquin) are common examples of antiinfectives used for conditions of the urinary tract.
antispasmodics: Anticholinergic drugs that relax the bladder for the treatment of incontinence. Examples include flavoxate (Urispas) and dicyclomine (Bentyl).
diuretics: Increase the formation of urine by promoting excretion of water and sodium. These drugs are often used to treat high blood pressure, congestive heart failure, and peripheral edema. Examples include hydrochlorothiazide (Hydro-Diuril, also found in many combinations), furosemide (Lasix), and triamterene (Dyrenium, also found in many combinations).
Recognizing Suffixes for PCS
Suffixes and Root Operations for the Urinary System
| Suffix | Root Operation |
| -ectomy | Excision, resection |
| -lithotomy | Extirpation |
| -lysis | Release |
| -pexy | Repair, reposition |
| -scopy | Inspection |
| -stomy | Bypass, drainage |
| -tomy | Drainage, division |
| -tripsy | Fragmentation |
Abbreviations for the Urinary System
| Abbreviation | Definition |
| ADH | antidiuretic hormone |
| ARF | acute renal failure |
| BUN | blood urea nitrogen |
| CAPD | continuous ambulatory peritoneal dialysis |
| Cl | chloride |
| CKD | chronic kidney disease |
| ESRD | end-stage renal disease |
| ESWL | extracorporeal shock wave lithotripsy |
| GFR | glomerular filtration rate |
| HD | hemodialysis |
| IC | interstitial cystitis |
| K | potassium |
| Na | sodium |
| TCC | transitional cell carcinoma |
| UA | urinalysis |
| UPJ | ureter pelvic junction |
| UTI | urinary tract infection |
Male Reproductive System
Functions of the Male Reproductive System
Anatomy and Physiology
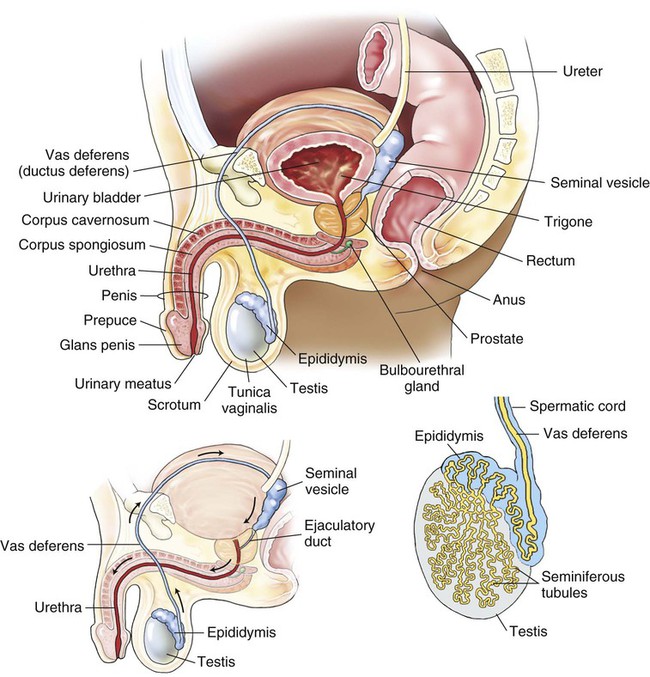
In the male, the gonads are the testes (sing. testis) or testicles, paired organs that produce the gametes called spermatozoa (sing. spermatozoon). The testes are suspended in a sac called the scrotum (pl. scrota) outside the body’s trunk (Fig. 6-12).
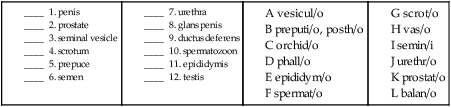
Combining Forms for the Anatomy of the Male Reproductive System
| Meaning | Combining Form |
| epididymis | epididym/o |
| glans penis | balan/o |
| gonad | gonad/o |
| juices | chym/o |
| penis | pen/i, phall/o |
| prepuce, foreskin | preputi/o, posth/o |
| prostate | prostat/o |
| scrotum | scrot/o |
| semen | semin/i |
| seminal vesicle | vesicul/o |
| spermatozoon | sperm/o, spermat/o |
| steroid | ster/o |
| stroma | strom/o |
| testis, testicle | test/o, testicul/o, orchid/o, orch/o |
| urethra | urethr/o |
| vas deferens, ductus deferens | vas/o |
Prefixes for the Anatomy of the Male Reproductive System
| Prefix | Meaning |
| en- | in |
| par- | near, beside |
Suffixes for the Anatomy of the Male Reproductive System
| Suffix | Meaning |
| -al, -ous, -ar, -ile, -atic, -ic | pertaining to |
| -ferous | pertaining to carrying |
| -genesis | production |
| -one | substance that forms |
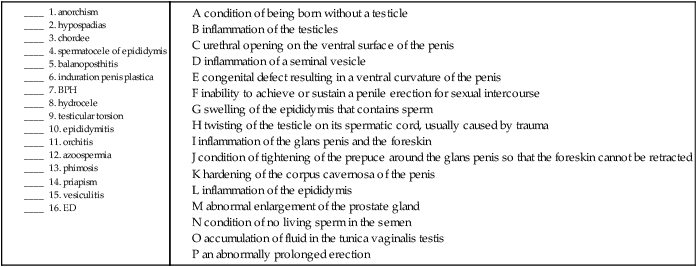
Pathology
Terms Related to Congenital Disorders (QØØ-Q99)
| Term | Word Origin | Definition |
| anorchism | an- no, not, without orch/o testis -ism condition |
Condition of being born without a testicle. May also be an acquired condition due to trauma or disease. Also termed monorchism. |
| chordee, congenital | chord/o cord | Congenital defect resulting in a downward (ventral) curvature of the penis due to a fibrous band (cord) of tissue along the corpus spongiosum. Often associated with hypospadias (Fig. 6-13). |
| cryptorchidism | crypt- hidden orchid/o testis -ism condition |
Condition in which the testicles fail to descend into the scrotum before birth. Also called cryptorchism (Fig. 6-14). |
| epispadias | epi- above -spadias a rent or tear |
Urethral opening on the dorsum (top) of the penis rather than on the tip. Also called hyperspadias. |
| hypospadias | hypo- below -spadias a rent or tear |
Urethral opening on the ventral surface (underside) of the penis instead of on the tip (Fig. 6-15). May be acquired as a result of a disease process. |
Terms Related to Diseases of Male Genital Organs (N4Ø-N51)
| Term | Word Origin | Definition |
| azoospermia | a- no, not, without zo/o animal sperm/o sperm -ia condition |
Condition of no living sperm in the semen. This may be a desired condition, as when it follows a vasectomy. |
| balanitis | balan/o glans penis -itis inflammation |
Inflammation of the glans penis. |
| balanoposthitis | balan/o glans penis posth/o foreskin -itis inflammation |
Inflammation of the glans penis and the foreskin. |
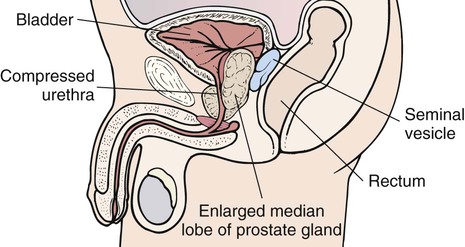
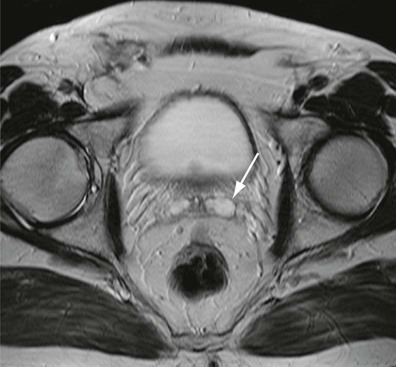
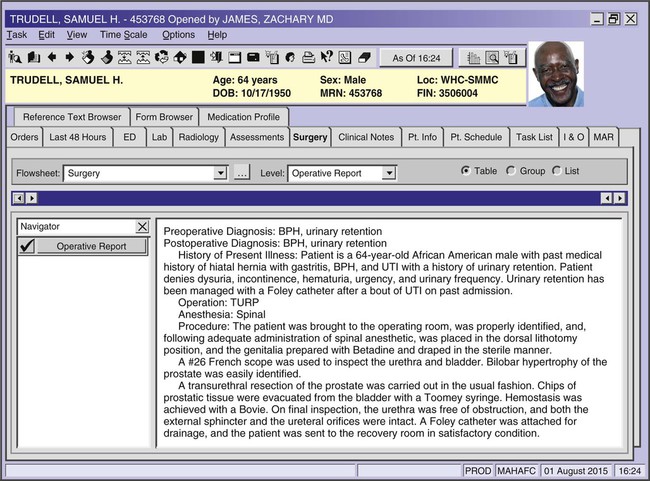
| benign prostatic hyperplasia (BPH) | prostat/o prostate -ic pertaining to hyper- excessive -plasia formation |
Abnormal enlargement of the prostate gland surrounding the urethra, leading to difficulty with urination (Fig. 6-16). Also known as benign prostatic hypertrophy and enlarged prostate. PSA (prostate-specific antigen) is a blood test used to diagnose BPH. Very high levels may indicate prostate cancer. |
| epididymitis | epididym/o epididymis -itis inflammation |
Inflammation of the epididymis, usually as a result of an ascending infection through the genitourinary tract. |
| erectile dysfunction (ED) | Inability to achieve or sustain a penile erection for sexual intercourse. Also known as impotence. | |
| hydrocele | hydr/o water, fluid -cele herniation, protrusion |
Accumulation of fluid in the tunica vaginalis testis (Fig. 6-17). |
| induration penis plastica | indur/o to make hard -ation process of |
A hardening of the corpus cavernosa of the penis that can cause painful erections. Idiopathic in nature. Also called Peyronie’s disease. |
| oligospermia | olig/o scanty, few sperm/o sperm -ia condition |
Condition of temporary or permanent deficiency of sperm in the seminal fluid; related to azoospermia. |
| orchitis | orch/o testis -itis inflammation |
Inflammation of the testicles; may or may not be associated with the mumps virus. Also known as testitis. |
| phimosis | Condition of tightening of the prepuce around the glans penis so that the foreskin cannot be retracted. May also be congenital. | |
| priapism | An abnormally prolonged erection. | |
| prostatitis | prostat/o prostate -itis inflammation |
Inflammation of the prostate gland. |
| spermatocele of epididymis | spermat/o sperm -cele herniation, protrusion |
A swelling of the epididymis that contains sperm. |
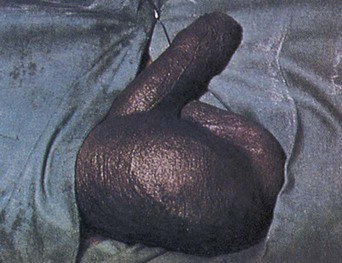
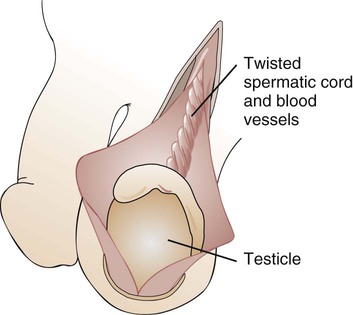
| testicular torsion | testicul/o testicle -ar pertaining to |
Twisting of a testicle on its spermatic cord, usually caused by trauma. May lead to ischemia of the testicle. Also called torsion of testis (Fig. 6-18). |
| vesiculitis | vesicul/o seminal vesicle -itis inflammation |
Inflammation of a seminal vesicle, usually associated with prostatitis. |
17. inflammation of the glans penis _________________________________________________________________
18. condition of no living sperm (in the semen) ______________________________________________________
19. inflammation of the prostate ____________________________________________________________________
20. a rent or tear above _____________________________________________________________________________
21. condition of hidden testis _______________________________________________________________________
Terms Related to Sexually Transmitted Diseases (STDs)
| The pathogens that cause STDs are various, but what they have in common is that all are most efficiently transmitted by sexual contact. The other term for STDs is venereal disease, abbreviated VD. Note that some of these are coded in the Certain Infectious and Parasite Diseases chapter. | ||
| Term | Word Origin | Definition |
| gonorrhea | gon/o seed -rrhea flow, discharge |
Disease caused by the gram-negative diplococcus Neisseria gonorrhoeae bacterium (Gc), which manifests itself as inflammation of the urethra, prostate, rectum, or pharynx (Fig. 6-19). The cervix and fallopian tubes may also be involved in females, although they may be asymptomatic, meaning without symptoms. Diagnosed with a Gram stain test, a method of staining microorganisms as either gram-negative or gram-positive. |
| herpes genitalis (herpes simplex virus, HSV-2) | Form of the herpesvirus transmitted through sexual contact, causing recurring painful vesicular eruptions (Fig. 6-20). | |
| human papillomavirus (HPV) | Virus that causes common warts of the hands and feet and lesions of the mucous membranes of the oral, anal, and genital cavities. A genital wart is referred to as a condyloma (pl. condylomata). | |
| nongonococcal urethritis (NGU) | urethr/o urethra -itis inflammation |
Inflammation of the urethra caused by Chlamydia trachomatis, Mycoplasma genitalium, or Ureaplasma urealyticum. |
| syphilis | Multistage STD caused by the spirochete Treponema pallidum. A highly infectious chancre, a painless, red ulcer, appears in the first stage, usually on the genitals. Diagnosed with a VDRL (Venereal Disease Research Laboratory) test and/or a FTA-ABS (fluorescent treponemal antibody absorption) test. | |
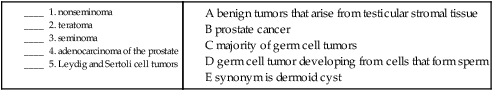
Terms Related to Benign Neoplasms (D29)
| Term | Word Origin | Definition |
| Leydig and Sertoli cell tumors | These testicular tumors arise from the stromal tissue of the testes that produce hormones. They are usually benign. |
Terms Related to Malignant Neoplasms (C6Ø-C63)
| Term | Word Origin | Definition |
| adenocarcinoma of the prostate | aden/o gland -carcinoma cancer of epithelial origin |
Prostate cancer is diagnosed in one of every six men. With early detection, however, this cancer is treatable (Fig. 6-21). |
| nonseminoma | non- not semin/i semen -oma tumor, mass |
Nonseminoma is a type of germ cell tumor (GCT). It accounts for the majority of testicular cancer cases and occurs in younger men, usually between the ages of 15 and 35. |
| seminoma | semin/i semen -oma tumor, mass |
This malignancy is one type of GCT that develops from the cells that form sperm (Fig. 6-22). |
| teratoma, malignant | terat/o deformity -oma tumor, mass |
This tumor is a type of nonseminoma that is usually benign in children. Because these tumors are created from germ cells, they have half of the necessary genetic information to form an individual. A synonym is the term dermoid cyst. |
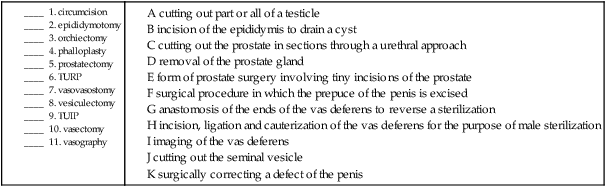
Procedures
| Term | Word Origin | Definition |
| balanoplasty | balan/o glans penis -plasty surgically forming |
Surgically correcting a defect of the glans penis. |
| circumcision | circum- around –cision cutting |
Surgical procedure in which the prepuce of the penis (or that of the clitoris of the female) is excised. |
| epididymotomy | epididym/o epididymis -tomy cutting |
Incision of the epididymis to drain a cyst. |
| epididymovesiculography | epididym/o epididymis vesicul/o seminal vesicle -graphy recording |
Imaging of the epididymis and seminal vesicle using a contrast medium (Fig. 6-23). |
| orchidectomy | orchid/o testis -ectomy cutting out |
Cutting out part or all of one or both testicles, usually for removal of a tumor or cyst. Also called orchectomy and orchiectomy. |
| orchiopexy | orchi/o testis -pexy suspension |
Surgical procedure to mobilize an undescended testicle, attaching it to the scrotum. |
| phalloplasty | phall/o penis -plasty surgically forming |
Surgically correcting a defect of the penis. |
| prostatectomy | prostat/o prostate -ectomy cutting out |
Removal of the prostate gland. In a radical prostatectomy, the seminal vesicles and area of vas ampullae of the vas deferens are also removed. |
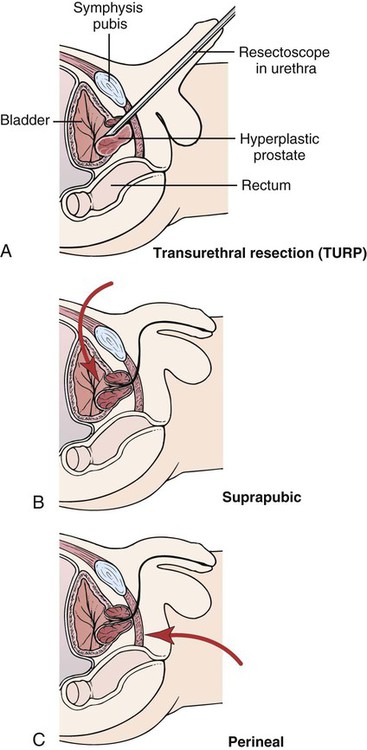
| transurethral resection of the prostate (TUR, TURP) | trans- through urethr/o urethra -al pertaining to |
Cutting out the prostate in sections through a urethral approach (Fig. 6-24). This procedure is the most common type of prostatectomy. The approach may be through the urethra (transurethral), above the pubic bone (suprapubic), or through the perineum (perineal). |
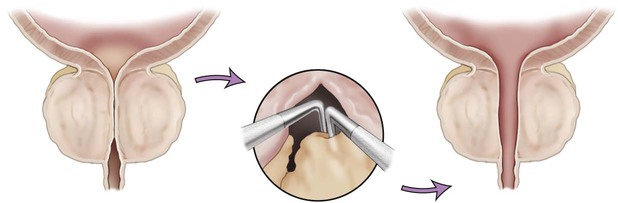
| transurethral incision of the prostate (TUIP) | trans- through urethr/o urethra -al pertaining to |
Form of prostate surgery involving tiny incisions of the prostate. The prostate is not removed (Fig. 6-25). |
| vasovasostomy | vas/o vas deferens vas/o vas deferens -stomy making a new opening |
Anastomosis of the ends of the vas deferens as a means of reconnecting them to reverse the sterilization procedure. |
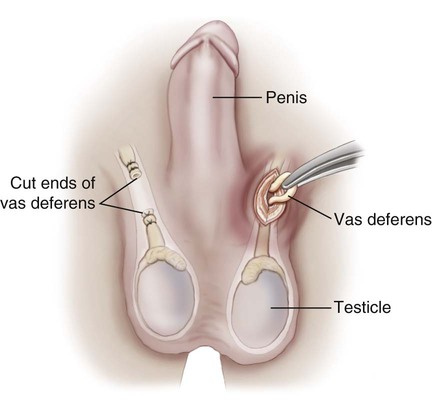
| vasectomy | vas/o vas deferens -ectomy cutting out |
Incision, ligation, and cauterization of both of the vas deferens for the purpose of male sterilization (Fig. 6-26). |
| vasography | vas/o vessel -graphy recording |
Imaging of the vas deferens to visualize possible blockages. |
| vasoligation | vas/o vessel -ligation tying |
A tying of the vas deferens as a sterilization procedure. |
| vesiculectomy | vesicul/o seminal vesicle -ectomy cutting out |
Cutting out the seminal vesicle. |
12. forming the glans penis _________________________________________________________________________
13. suspending a testis ______________________________________________________________________________
14. recording the epididymis and seminal vesicle _____________________________________________________
15. tying a vessel ___________________________________________________________________________________
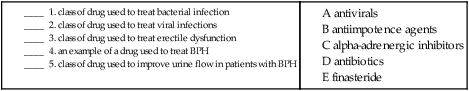
Pharmacology
alpha-adrenergic inhibitors: Block alpha-1 adrenergic receptors to relax smooth muscle in prostate to improve urinary flow. Examples include tamsulosin (Flomax) and terazosin (Hytrin).
androgen antagonists: Block receptors or inhibit synthesis of androgen hormones. Finasteride (Proscar) and dutasteride (Avodart) block the conversion of testosterone to the more potent hormone 5-alpha-dihydrotestosterone (DHT) to suppress growth of and even shrink the enlarged prostate. Saw palmetto (Serenoa repens) is an alternative medicine that has been shown to be effective in treating symptoms of BPH.
antibiotics: Treat bacterial infection. Penicillin G, tetracycline, and doxycycline all can be used to treat syphilis.
antiimpotence agents: Used to alleviate erectile dysfunction. Sildenafil (Viagra) and tadalafil (Cialis) are examples of oral agents. Alprostadil (Caverject) is injected directly into the corpus cavernosum of the penis.
antivirals: Treat viral infections. Acyclovir (Zovirax) is used to treat genital herpes virus.
Suffixes and Root Operations for the Male Reproductive System
| Suffix | Root Operation |
| -cision | Resection |
| -ectomy | Excision, resection |
| -ligation | Occlusion |
| -pexy | Repair, reposition |
| -plasty | Repair, supplement |
| -stomy | Repair |
| -tomy | Drainage |
Abbreviations for the Male Reproductive System
| Abbreviation | Definition |
| BPH | benign prostatic hyperplasia/hypertrophy |
| ED | erectile dysfunction |
| FTA-ABS | fluorescent treponemal antibody absorption |
| Gc | gonococcus |
| GCT | germ cell tumor |
| HPV | human papillomavirus |
| HSV-2 | herpes simplex virus-2, herpes genitalis |
| NGU | nongonococcal urethritis |
| PSA | prostate-specific antigen |
| STD | sexually transmitted disease |
| TUIP | transurethral incision of the prostate |
| TUR | transurethral resection (of the prostate) |
| TURP | transurethral resection of the prostate |
| VD | venereal disease |
| VDRL | Venereal Disease Research Laboratory |