Chapter 23 Genitourinary Dysfunction
PELVIC ORGAN PROLAPSE, URINARY INCONTINENCE, AND INFECTIONS
 Pelvic Organ Prolapse
Pelvic Organ Prolapse
Pelvic organ prolapse (POP) refers to protrusion of the pelvic organs into the vaginal canal or beyond the vaginal opening. It results from a weakness in the endopelvic fascia investing the vagina, along with its ligamentous supports. Defects in vaginal support may occur in isolation (e.g., anterior vaginal wall only) but are more commonly combined. The nomenclature of POP has evolved such that cystocele, rectocele, and enterocele have been replaced by more anatomically precise terms (Figure 23-1).
APICAL VAGINAL AND UTERINE PROLAPSE
Complete procidentia (uterine prolapse through the vaginal hymen) represents failure of all the vaginal supports (Figure 23-2). Hypertrophy, elongation, congestion, and edema of the cervix may sometimes cause a large protrusion of tissue beyond the hymen, which may be mistaken for a complete procidentia. Vaginal vault prolapse or eversion of the vagina may be seen after vaginal or abdominal hysterectomy and represents failure of the supports around the upper vagina.
QUANTIFYING AND STAGING PELVIC ORGAN PROLAPSE
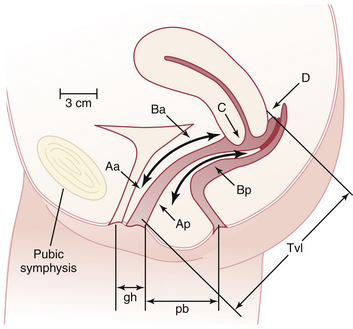
The preferred method to describe and document the severity of POP is the Pelvic Organ Prolapse Quantification (POP-Q) system. The extent of prolapse is evaluated and measured relative to the hymen, which is a fixed anatomic landmark. The anatomic position of the six defined points for measurement is denoted in centimeters above the hymen (negative number) or centimeters below the hymen (positive number). The plane at the level of the hymen is defined as zero (Figure 23-3).
Stages of POP can be assigned according to the most severe portion of the prolapse after the full extent of the protrusion has been determined. An ordinal system is used for measurements of different points along the vaginal canal and allows for better communication among clinicians. This staging system enables more objective tracking of surgical outcomes (Table 23-1).
| Stage | Characteristics |
|---|---|
| 0 | No prolapse |
| Aa, Ba, Ap, Bp are −3 cm and C or D ≤ −(tvl −2) cm | |
| 1 | Most distal portion of the prolapse −1 cm (above the level of hymen) |
| 2 | Most distal portion of the prolapse ≥ −1 cm but ≤ +1 cm (≤1 cm above or below the hymen) |
| 3 | Most distal portion of the prolapse > +1 cm but > +(tvl − 2) cm (beyond the hymen; protrudes no farther than 2 cm less than the total vaginal length) |
| 4 | Complete eversion; most distal portion of the prolapse ≥ +(tvl − 2) cm |
Aa, point A of anterior wall; Ba, point B of anterior wall; Ap, point A of posterior wall; Bp, point B of posterior wall; −, above the hymen; +, beyond the hymen; tvl, total vaginal length.
Reproduced with permission from Harvey MA, Versi E: Urogynecology and pelvic floor dysfunction. In Ryan KJ, Berkowitz RS, Barbieri RL, Dunaif A (eds): Kistner’s Gynecology and Women’s Health, 7th ed. St. Louis, Mosby, 1999. Copyright © 1999 Elsevier.
MANAGEMENT
Nonsurgical Treatment
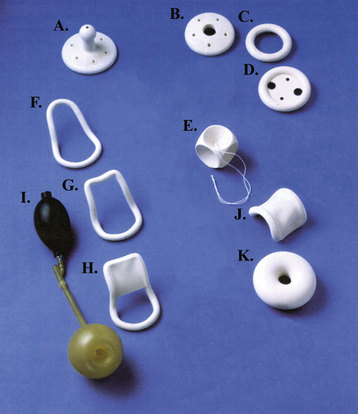
When only a mild degree of pelvic relaxation is present, pelvic floor muscle exercises may improve the tone of the pelvic floor musculature. Pessaries, which provide intravaginal support (Figure 23-4), may be used to correct prolapse by “propping up” the vagina. They can be considered when the patient is medically unfit or refuses surgery or during pregnancy and the postpartum period. They are also useful to promote healing of a decubitus ulcer before surgery for prolapse.
 Urinary Incontinence
Urinary Incontinence
 Stress Urinary Incontinence
Stress Urinary Incontinence
SUI is involuntary leakage of urine in response to physical exertion, sneezing, or coughing.
DIAGNOSTIC TESTS
Cotton Swab (Q-Tip) Test
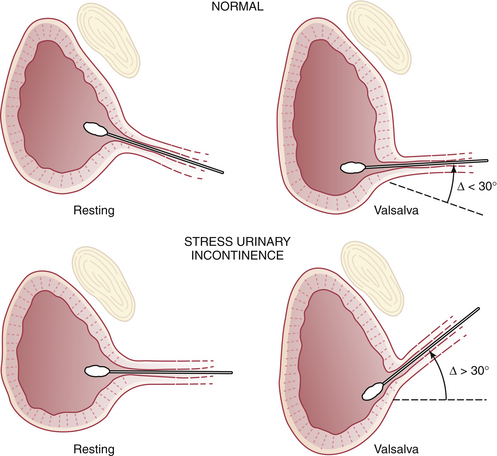
This test determines the mobility and descent of the urethrovesical junction on straining and allows differentiation from anterior vaginal laxity alone. With the patient in the lithotomy position, the examiner inserts a lubricated cotton swab into the urethra to the level of the urethrovesical junction and measures the angle between the cotton swab and the horizontal. The patient then strains maximally, which produces descent of the urethrovesical junction. Along with the descent, the cotton swab moves, producing a new angle with the horizontal. The normal change in angle is up to 30 degrees. In patients with pelvic relaxation and SUI, the change in cotton swab angle ranges from 30 to 60 degrees or more (Figure 23-5).
Cystometrogram
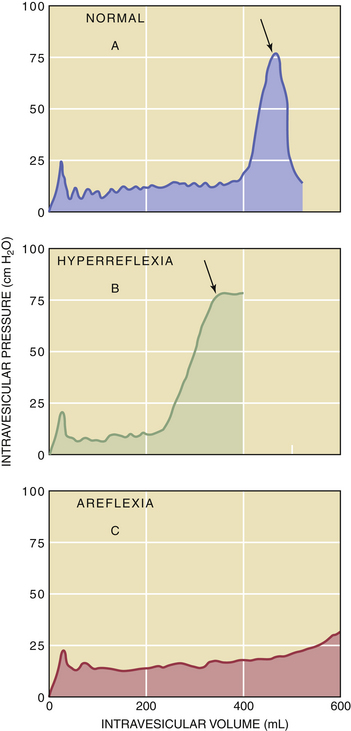
The first sensation of bladder filling should occur at volumes of 150 to 200 mL. The critical volume (400 to 500 mL) is the capacity that the bladder musculature tolerates before the patient experiences a strong desire to urinate. At this point, if the patient is asked to void, a terminal contraction may appear and is seen as a sudden rise in intravesical pressure. At the peak of the contraction, the patient is instructed to inhibit this reflex (indicated by arrows in Figure 23-6). A normal person should be able to inhibit this detrusor reflex and thereby bring down intravesical pressure (see Figure 23-6A). In a urologically or neurologically abnormal patient, the detrusor reflex may appear without the specific instruction to void, and the patient cannot inhibit it (see Figure 23-6B); this observation is referred to as an uninhibited detrusor contraction. Other terms for this disorder include overactive bladder, detrusor dyssynergia, detrusor hyperreflexia, irritable bladder, hypertonic bladder, unstable bladder, and uninhibited neurogenic bladder.
These cystometric procedures allow differentiation between patients who are incontinent as a result of uninhibited detrusor contraction and those who have SUI. Conversely, the hypotonic bladder accommodates excessive amounts of gas or water with little increase in intravesical pressure, and the terminal detrusor contraction is absent when the patient is asked to void (see Figure 23-6C).
TREATMENT
Intravaginal Devices
Larger sizes of pessaries (see Figure 23-4) have been used to elevate and support the bladder neck and urethra. They have been shown to be effective for SUI.
 Urge Urinary Incontinence and Overactive Bladder
Urge Urinary Incontinence and Overactive Bladder
The incidence of overactive bladder increases with age, approximating 30% in the geriatric patient population. In most patients, the exact etiology of bladder instability remains unknown, but a number of risk factors are associated with its development (Box 23-1).
 Urethral Syndrome
Urethral Syndrome
The urethral syndrome occurs in a patient with various lower urinary tract symptoms, including acute or chronic pain (see Chapter 21), in the absence of obvious bladder or urethral abnormality, and with no evidence of UTI. Any combination of symptoms may be present, the most common being urinary frequency, urgency, dysuria, postvoid fullness, incontinence, and dyspareunia.
 Urinary Tract Infection
Urinary Tract Infection
TERMINOLOGY
The terminology surrounding UTIs is rather complex and requires some definition.
INCIDENCE AND PREVALENCE
After the age of 1 year and throughout adulthood, females are affected more frequently than males (10:1 ratio). Asymptomatic bacteriuria increases from an incidence in preschool children of 1% to 5% to a peak of about 10% in postmenopausal women. Urologic abnormalities are found in up to 70% of children with a UTI. Box 23-2 lists the risk factors for UTIs in premenopausal and postmenopausal women.
PERPETUATING FACTORS
The following factors encourage and perpetuate UTIs:
MANAGEMENT
Basic Principles of Antimicrobial Therapy
Single-dose therapy is an effective alternative to a 3- to 7-day course, especially in patients with acute uncomplicated cystitis. Single-dose therapy fails, however, in more than 50% of patients with an upper tract infection. Table 23-2 lists some common antibiotic regimens for uncomplicated cystitis along with their relative costs.
TABLE 23-2 COMMON TREATMENT REGIMENS FOR UNCOMPLICATED BACTERIAL CYSTITIS
| Antimicrobial Agent | Dose | Relative Cost∗ |
|---|---|---|
| SINGLE-DOSE TREATMENTS | ||
| Ampicillin† | 2 g | 1 |
| Amoxicillin† | 3 g | 1 |
| Nitrofurantoin | 200 mg | 1 |
| Fosfomycin tromethamine | 3 g (powder) | 3 |
| THREE-DAY COURSE | ||
| Ampicillin† | 250 mg 4 times daily | 1 |
| Amoxicillin† | 500 mg 3 times daily | 1 |
| Trimethoprim | 100 mg twice daily | 2 |
| Ciprofloxacin | 250 mg twice daily | 3 |
| SEVEN– TO 10-DAY COURSE | ||
| Nitrofurantoin | 100 mg at bedtime | 3 |
| Nitrofurantoin macrocrystals | 50-100 mg 4 times daily | 4 |
∗ Relative cost: 1-4, less to more expensive.
RECURRENT URINARY TRACT INFECTIONS
Prevention of hospital-acquired UTIs in patients is important.
Sixty percent of hospital-acquired infections in gynecologic patients involve the urinary tract and occur particularly in association with catheterization. The principles shown in Box 23-3 should be employed when drainage of the urinary bladder is performed.
American College of Obstetricians and Gynecologists (ACOG). Pelvic organ prolapse. Practice Bulletin No. 85. Washington, DC: ACOG; September 2007.
American College of Obstetricians and Gynecologists (ACOG). Urinary incontinence in women. Practice Bulletin No. 63. Washington, DC: ACOG; June 2005.
American College of Obstetricians and Gynecologists (ACOG). Treatment of urinary tract infections in nonpregnant women. Practice Bulletin No. 91. Obstet Gynecol. 2008;111:785-794.
Bhatia N.N., Bradley W.E. Neuroanatomy and neurophysiology of the lower urinary tract: Female incontinence. In: Raz S., editor. Female Urology. Philadelphia: WB Saunders; 1983:12-32.
Rahn D.D., Marker A.C., Corton M.M., et al. Does supracervical hysterectomy provide more support to the vaginal apex than total abdominal hysterectomy? Am J Obstet Gynecol. 197, 2007. 650e1–650e4

 Normal Pelvic Anatomy and Supports
Normal Pelvic Anatomy and Supports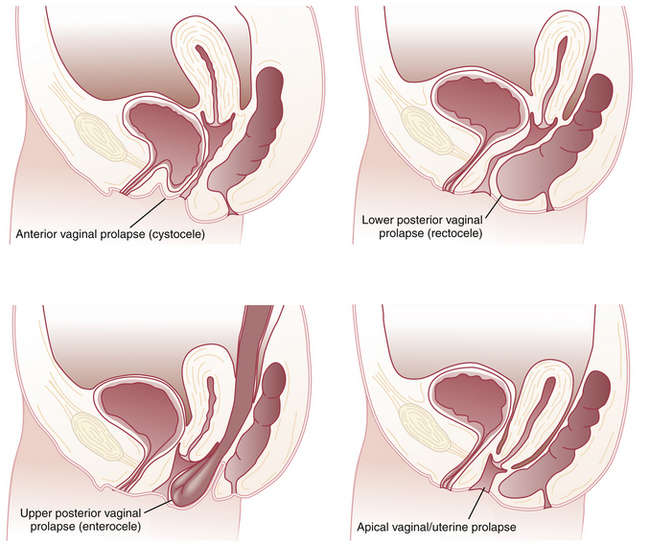

 Overflow Incontinence
Overflow Incontinence Urinary Fistula
Urinary Fistula