Gender Reassignment Surgery
Transsexualism is a bona fide psychosexual disorder in which a dissociation exists between the individual’s morphologic sex and the brain’s innate perception of that person’s gender identity. Over the past 50 years, attempts to correct the central nervous system abnormality have been totally unsuccessful; thus surgery designed to change the morphologic sex has been performed to correct the paradox. This surgery typically is done within centers that specialize in these unusual sexual disorders. No operative procedure should ever be performed without proper screening, including thorough psychological, psychiatric, and sociologic testing followed by medical evaluation and hormonal therapy (Fig. 104–1). Additionally, and most important, every surgical candidate must successfully complete at least a year’s trial of living and dressing in the desired sex of choice. At the end of the 1-year test period, the candidate again is thoroughly evaluated by a multidisciplinary team, which must unanimously agree that surgery is the appropriate therapy for that individual. Finally, the patient must be given an extensive and detailed informed consent, which explains that the surgery once performed is irreversible. Other persons (e.g., hermaphrodites) may undergo similar types of surgery. As in the case of transsexuals, the screening and evaluation process should be similarly stringent. Before surgery is conducted, as with transsexuals, a multidisciplinary committee, including the patient and the patient’s immediate family, should be included in the informed decision to perform gender reassignment surgery. The type of surgery in which the gynecologist will be involved is the male-to-female reassignment procedure. All patients will have been feminized by more than 12 months’ treatment with injections of estradiol (Fig. 104–2). Every patient also undergoes bowel preparation.
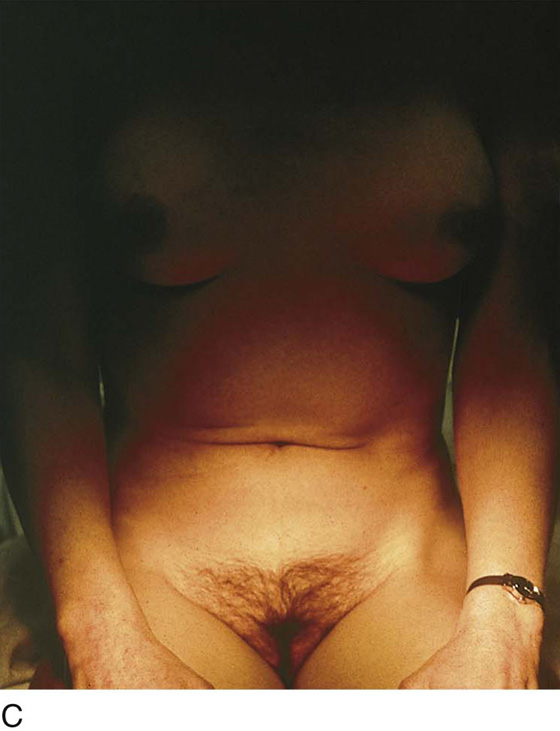
FIGURE 104–1 Excellent breast development may be seen in the majority of male-to-female transsexuals through the administration of injectable estrogen. Maximal action is observed between 3 and 6 months after injections are begun.
FIGURE 104–2 After cross-dressing, receiving hormonal therapy, and living as a woman for a period of a year, candidates for surgery are evaluated by a multidisciplinary committee. This person presents as an authentic-looking female.
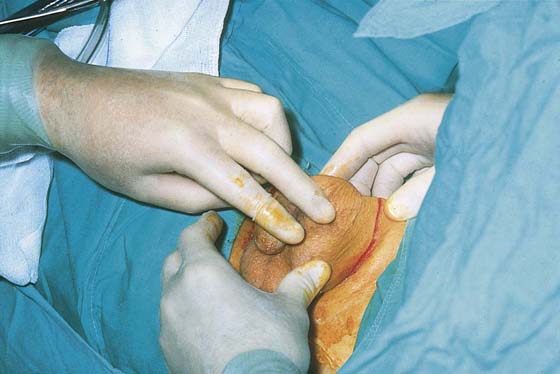
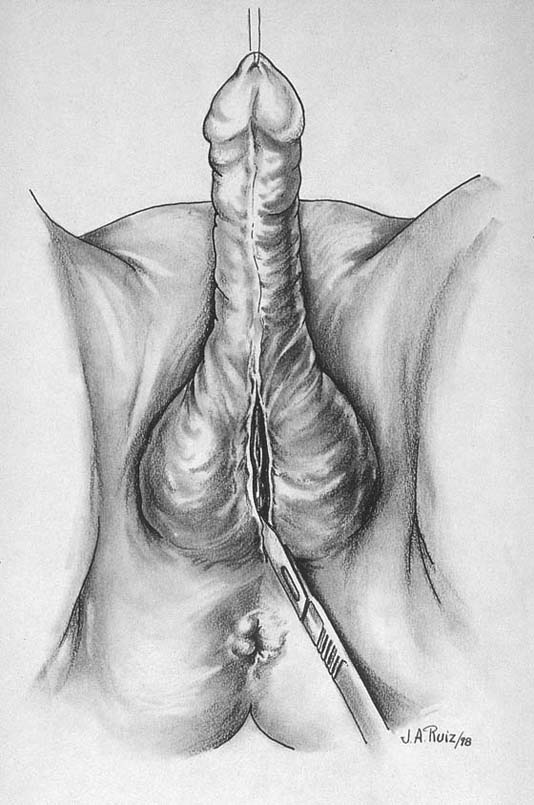
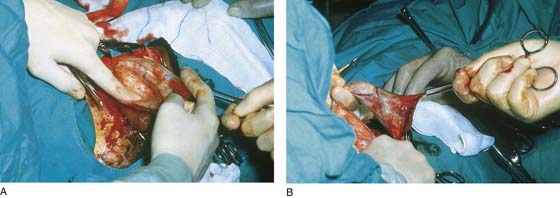
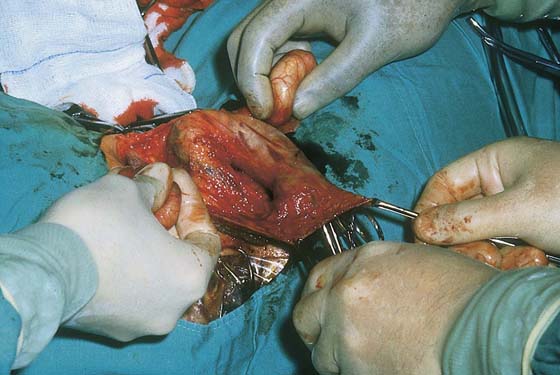
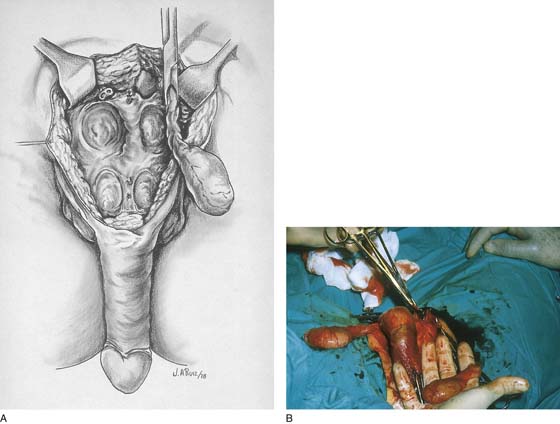
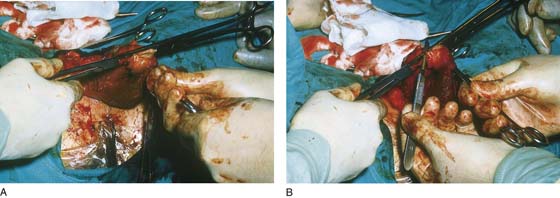
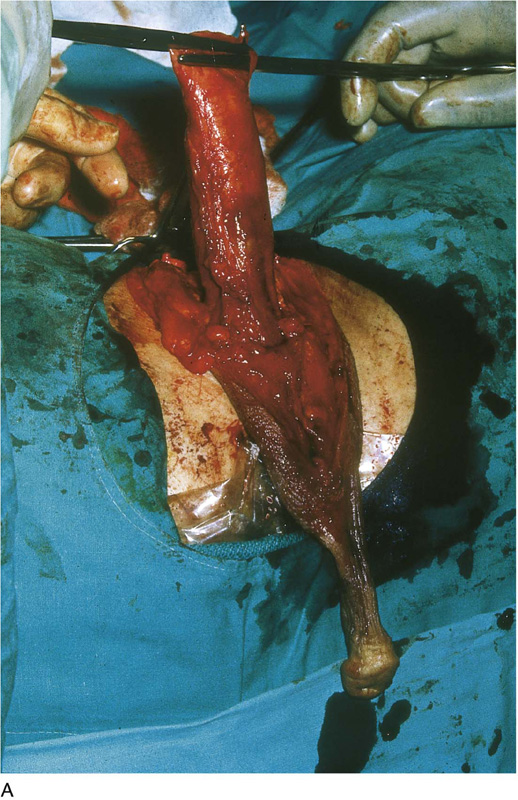
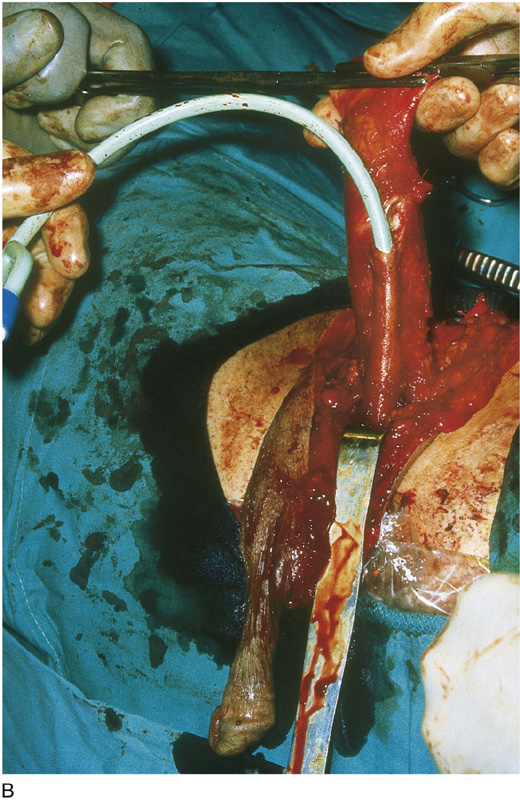
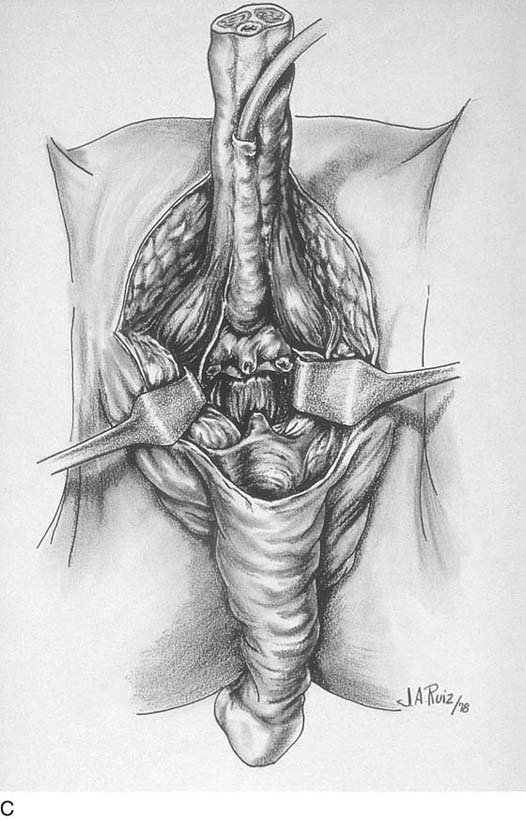
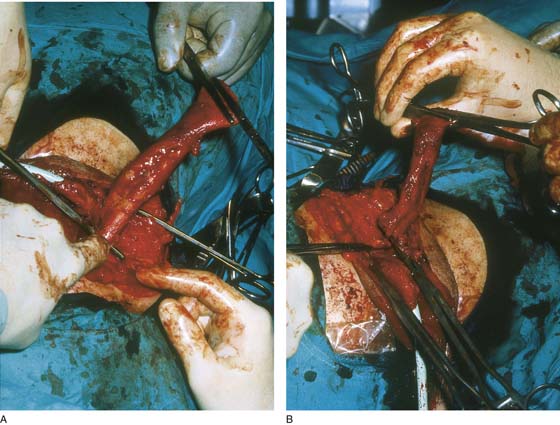
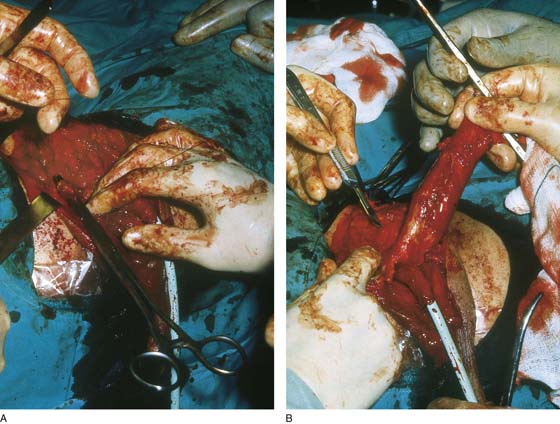
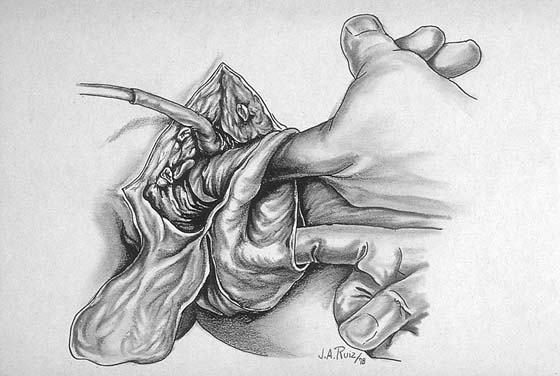
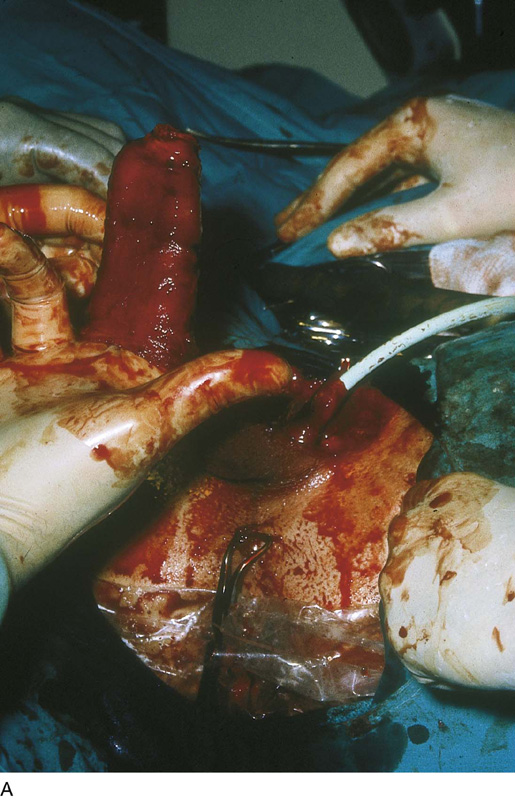
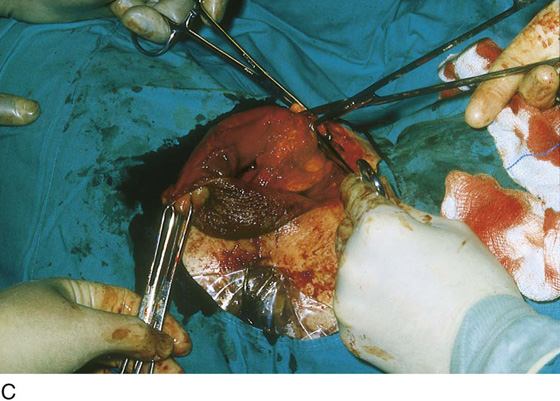
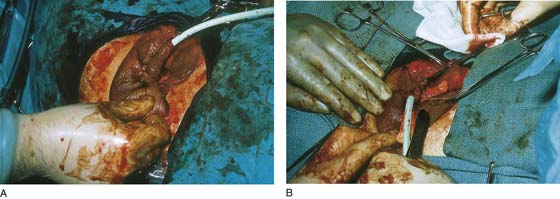
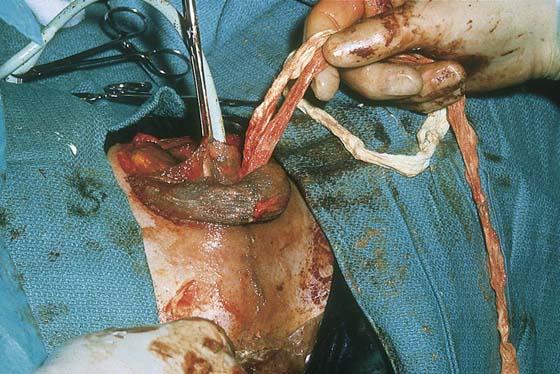
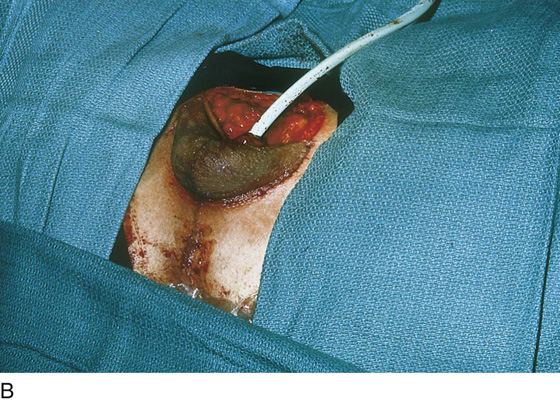
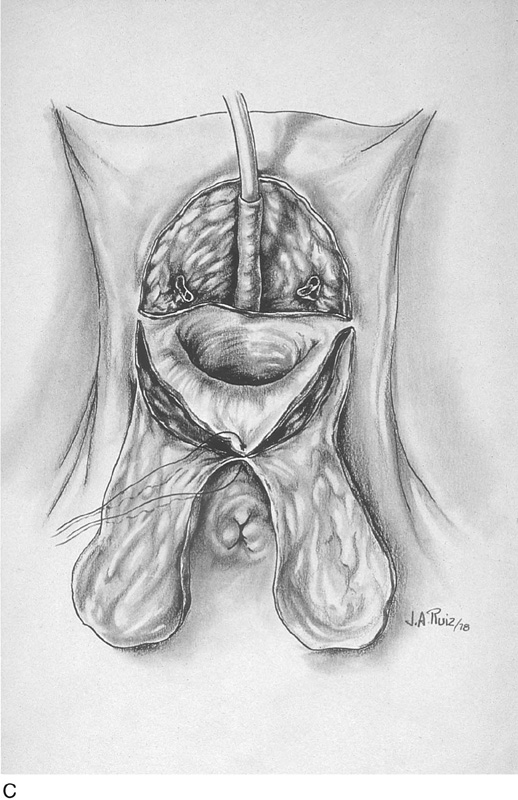
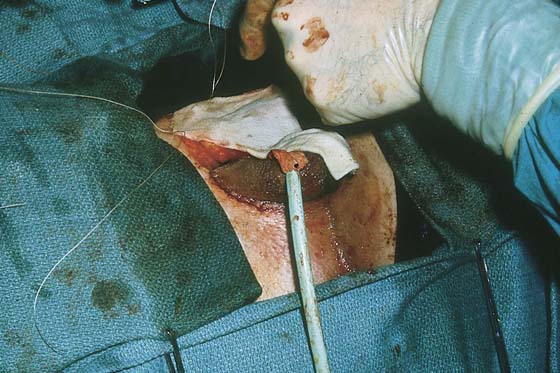
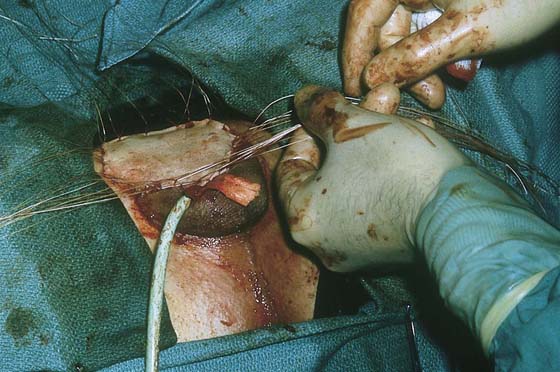
The surgery is performed with the patient in the lithotomy position (Fig. 104–3). However, before positioning, a split-thickness graft is obtained utilizing a drum-type dermatome (Fig. 104–4). The full-drum graft is obtained from the buttock or thigh (Fig. 104–5). The donor site is then covered with a polyurethane-type dressing (Opsite). The external genitalia and abdomen are completely shaved of hair, and a Foley catheter is placed via the penile urethra into the urinary bladder. A hemispheric incision is made into the mons at the junction of the penile root and the mons. This is carried down to the upper lateral portion of the scrotum (Fig. 104–6). The incision alternatively may comprise a short vertical incision into the scrotum and ventral surface of the penile skin (Fig. 104–7). The incision is carried down to Colles’ fascia. By careful, nontraumatic sharp and blunt dissection, the penile skin is separated from the entire penile shaft to the level of the glans (Fig. 104–8A, B). The testes are dissected free from the scrotal skin (Fig. 104–9). The spermatic cords are doubly clamped, cut, and suture-ligated with 0 Vicryl, and the testes removed (Fig. 104–10A, B). The penile shaft proximal to the glans is clamped with a straight Zeppelin clamp, and the glans, together with the penile skin, is separated from the shaft (Fig. 104–11A, B). The urethra is recatheterized and is dissected from the bulb and shaft of the penis (Fig. 104–12A through C). On either side, the corpora cavernosa penis is isolated close to the pubic and ischial rami, clamped with two Zeppelin clamps, cut, and suture-ligated with 0 Vicryl or polydioxanone (PDS) (Fig. 104–13A, B). The entire corpora cavernosa penis is removed after it is sharply dissected from the urethral bulb (Fig. 104–14A, B). Next, a transverse incision is made between the base of the urethral bulb and the rectum (Fig. 104–15). By very careful dissection, a space is developed between the aforementioned structures and deeper internally between the prostate gland and the rectum. The space must accommodate the width of the operator’s index and center fingers loosely and must extend to a depth of 7 cm. Frequent rectal exams are performed during the critical tunneling phase. The full-thickness penile skin pedicle graft is inverted into the space, creating a full-thickness neovagina (Fig. 104–16A, B). The glans penis will be located at the vault and creates a pseudocervix (Fig. 104–16C). The urethra is shortened to approximately 3 to 4 cm and is recatheterized (Fig. 104–17A, B). The neovagina is packed with gauze (Fig. 104–18). The scrotum is sutured upward peripheral to the neovagina into Colles’ fascia (Fig. 104–19A, B). At a second stage of the operation, the scrotum will be sectioned and separated centrally at its lower pole to create two labia majora. At the 2-month interval (second-stage operation), it will have gained sufficient collateral circulation to obviate slough (Fig. 104–19C). The split-thickness graft is cut to cover the large mons defect and is sutured to the margins of the abdominal, penile, and scrotal skin (Fig. 104–20). A hole is cut above the neovaginal introitus, and the urethra is brought out through this orifice. The edges of the terminal urethra are sutured circumferentially to the margins of the previously described opening in the skin graft with 4-0 Vicryl (Fig. 104–21). The operation is now finished. A pressure dressing is placed over the graft site and is taped into place (Fig. 104–22).
FIGURE 104–3 Surgery is performed with the patient in the dorsal lithotomy position by a team consisting of a gynecologist, a plastic surgeon, and a urologist.
FIGURE 104–4 Before the patient is placed in the lithotomy position, a split-thickness graft is obtained using a drum-type dermatome.
FIGURE 104–5 A large split-thickness graft is retrieved from the drum. It is carefully wrapped in a moistened sterile gauze sponge and is placed in a secure location on the nurse’s instrument back table for later use.
FIGURE 104–6 A curved incision is made above the root of the penis and is carried laterally to the lateral lower margin of the scrotum. The incision is carried to the level of Colles’ fascia.
FIGURE 104–7 Alternatively, a midline incision bisecting the scrotum and into the lower ventral skin of the penis may be made (optional).
FIGURE 104–8 A. By blunt dissection, the penile skin is carefully separated from the fascia covering the penile shaft and scrotum. B. The skin is pulled downward to the level of its firm attachment to the glans penis.
FIGURE 104–9 The scrotal skin is bluntly pushed inferiorly. The testes are separated from the scrotum.
FIGURE 104–10 A. The spermatic cord is isolated, clamped, and cut. B. The testes are excised, and the cord is suture-ligated with 0 Vicryl.
FIGURE 104–11 A. Zeppelin clamps are placed across the terminal part of the penile shaft below the glans and retracted penile skin. B. The penile shaft is cut distal to the applied clamps separating the glans, which remains attached to the penile skin.
FIGURE 104–12 A. The penile shaft, now free from its skin and glans, is stretched to reveal the urethra and bulb groove. B. The urethra is dissected by means of Metzenbaum scissors from the corpora. A catheter is placed into the urethra and bladder. C. The drawing shows the empty sheath of penile skin with attached glans. The corpora cavernosa and the catheterized urethra and bulb are seen above the skin sheath.
FIGURE 104–13 A. Each corpus cavernosum is isolated at the ischiopubic ramus. Using a straight tonsil clamp, a tunnel is dissected between the corpora. Zeppelin clamps are applied over the bone, securing the right and left corpora cavernosa penis. B. The right and left corpora are cut over the clamp.
FIGURE 104–14 A. The corpus stump on the right is suture-ligated twice with 0 Vicryl. B. The urethra is shortened to the level of the bulb.
FIGURE 104–15 The levator ani is carefully cut between the bulb (anteriorly) and the rectum posteriorly, and the neovagina is tunneled bluntly. The cavity is dissected posteriorly to the atrophied prostate gland.
FIGURE 104–16 A. The full-thickness tube of penile skin is inverted and will form the neovagina. B. The penile skin tube is pushed into the space created through the levator ani muscles. The entire length of penile skin is pushed into the space. C. The glans penis sits at the deep end of the pedicle graft (penile skin tube). The glans will simulate a female cervix. On speculum exam, it looks and feels like a genuine cervix.
FIGURE 104–17 A. The urethra is further shortened and sculpted. B. The urethra is anchored to the connective tissue above the graft. Later, it will be brought through the split-thickness graft.
FIGURE 104–18 The neovagina is packed with petroleum gauze.
FIGURE 104–19 A. The empty scrotum is sutured around the entrance of the neovagina to the connective tissue (Colles’ fascia). B. The scrotum if not split will be left intact for 2 months and separated to form two labia at a short second operation. This delay is required to ensure an adequate blood supply to the skin. C. Alternatively, if the midline cut was made into the scrotum (see Figure 104–7), the two halves of the scrotum will become the labia majora.
FIGURE 104–20 The split-thickness graft obtained at the beginning of the surgery covers the denuded area above the neovagina. The urethra is brought through a cut made in the graft, and the edges of the terminal urethra are sutured to the skin graft (around the slit) with 3-0 or 4-0 Vicryl. Care is taken to make the skin opening large enough to prevent urethral stricture.
FIGURE 104–21 The graft is secured to the surrounding skin margins with interrupted 3-0 Vicryl stitches. The excess skin is trimmed.
FIGURE 104–22 Xeroform gauze and a uniform pressure dressing are secured over the graft by tying the long suture ends over the dressing.
During this time, the patient is placed on a low-residue diet, and a retention catheter remains in the bladder. The patient remains on ciprofloxacin (Cipro) 500 g twice a day for the 2-week period. Essentially, the operation recapitulates embryonic sexual differentiation, creating an unfused (female) status from a previously fused (male) condition. At 4 weeks postoperatively, the patient is fitted with a Silastic vaginal stent, which she must wear continuously until beginning actual intercourse (Fig. 104–23A through C). Healing is complete at 6 to 8 weeks. The cosmetic appearance after this surgery is very good (Fig. 104–24A through C). Similar surgery may be performed for hermaphrodites; however, the enlarged clitoris is too small for a full-thickness graft (Fig. 104–25).
FIGURE 104–23 A. Various sizes of Silastic vaginal stents will be placed into the neovagina after the wounds have healed, usually 6 weeks postoperatively. B. The patient is taught to lubricate the vagina and the stent and place the latter in the vagina. C. The stent remains in the vagina continuously until regular intercourse ensues. The stent is removed and is cleaned once or twice daily.
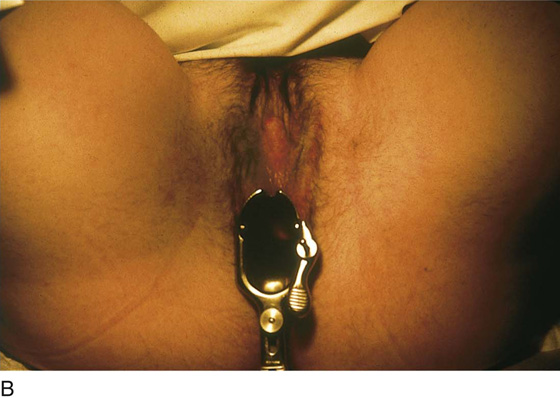
FIGURE 104–24 A. At 12 weeks postoperatively, the vulva and vagina appear cosmetically authentic. B. This standard Graves speculum easily negotiates the neovagina. C. This male-to-female transsexual appears to be a morphologically normal female.
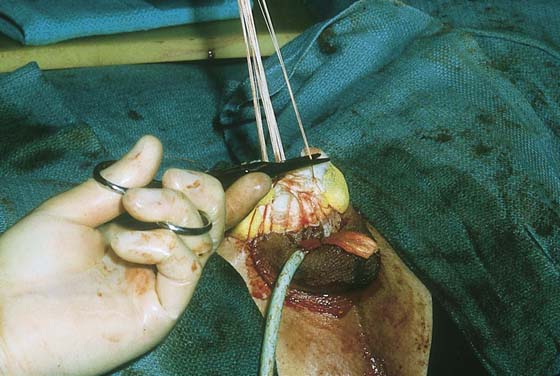
FIGURE 104–25 The hermaphrodite pictured here has a micropenis (clitoris). This individual’s karyotype is XY. The urethra opens at the base of the micropenis.