CHAPTER 13 Gastrointestinal Disorders
II. Peptic Ulcer Disease
A. Pathology
1. Peptic ulcers occur when the digestive juices that help food digest damage the walls of the stomach or duodenum. The most common cause is infection with a bacterium called Helicobacter pylori, or H. pylori. Another cause is the long-term use of nonsteroidal anti-inflammatory drugs (NSAID) such as aspirin and ibuprofen (e.g., Motrin, Advil) (Table 13-1). Spicy foods do not cause ulcers, but can aggravate them and make them worse.
E. Treatment
1. Because many ulcers are caused by H. pylori bacteria, an approach to peptic ulcer treatment that eradicates the bacteria and reduces the level of acid in the digestive system is used. The result of the treatment is pain relief and ulcer healing.
2. Histamine H2 antagonists or H2 blockers
3. Antibiotics
5. Proton pump inhibitors (PPI)
a) Superior to H2 blockers in the healing, recurrence, and prevention of ulcers. Used preferentially with antibiotics in H. pylori eradication and ulcer treatment regimens.
c) Adverse effects and precautions
III. Gastroesophageal Reflux Disease
Table 13-1 Characteristics of H. pylori versus NSAID-induced ulcers
| H. pylori | Nonsteroidal anti-inflammatory drugs (NSAIDs) |
|---|---|
| Direct mucosal damage caused by hypergastrinemia | Direct mucosal damage associated with prostaslandin inhibition |
| Ulcers are superficial; chronically inflamed | Ulcers are deep; no inflammation |
| Symptoms: epigastric pain (may be nocturnal), nausea, indigestion, fatigue | Patients are usually asymptomatic; complications cause bleeding perforation |
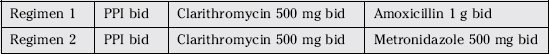
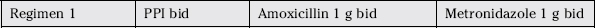
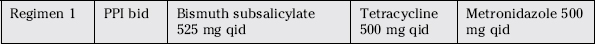
Box 13-1 Treatment Regimens for H. Pylori
• Combination therapy of a proton pump inhibitor (PPI) plus two antibiotics is generally recommended for treating H. pylori.
C. Signs and symptoms
5. Several factors may worsen symptoms of the condition including spicy foods, fatty foods, chocolate, caffeine, tomato sauce, carbonated beverages, mint, alcoholic beverages, large meals, lying down after eating, some medications (e.g., sedatives, tranquilizers, or blood pressure drugs), and cigarette smoking.
IV. Inflammatory Bowel Disease
D. Signs and symptoms
1. The symptoms of these two illnesses are similar, which often makes it difficult to distinguish between the two. In fact, about 10% of colitis (inflamed colon) cases cannot be diagnosed as either ulcerative colitis or Crohn’s disease. When physicians cannot diagnose the specific IBD, the condition is called indeterminate colitis.
2. IBD causes chronic inflammation in the gastrointestinal tract and may lead to complications, such as colon cancer. The most common symptoms of both ulcerative colitis and Crohn’s disease are diarrhea (ranging from mild to severe), abdominal pain, decreased appetite, and weight loss. If the diarrhea is extreme, it may lead to dehydration, increased heartbeat, and decreased blood pressure. As food moves through inflamed areas of the gastrointestinal tract, it may cause bleeding.
E. Treatment
3. Pharmacologic therapy
V. Irritable Bowel Syndrome
| Ulcerative colitis | Crohn disease | |
|---|---|---|
| Anatomic sites | Colon and rectum | Any part of the GI tract |
| Lesions | Continuous and superficial | Discontinuous |
| Depth of involvement | Mucosa and submucosa inflammation | Transmural inflammation |
| Pathologic findings | Polyps | Obstruction due to inflammation Perforation Perianal fistulas |
D. Signs and symptoms
1. In patients with IBS, the muscles of the colon, sphincters, and pelvis do not contract properly. As a result, patients experience constipation or diarrhea. This causes symptoms of abdominal pain, cramping, bloating, and a sense of incomplete stool movement. Symptoms may improve after the patient has a bowel movement.
E. Treatment
2. Pharmacologic
b) Diarrhea-predominant IBS
VI. Nausea and Vomiting
A. Pathophysiology
1. Three stages
2. The brain and the GI tract are involved in the processes of nausea and vomiting, which include chemoreceptor trigger zone (CTZ) in the brain, the vestibular system, visceral afferents from the GI tract, and the cerebral cortex. The stimulation of the CTZ sends impulse to the vomiting center. The CTZ contains dopamine, histamine, acetylcholine, serotonin receptors, and neurokinin-1.
C. Signs and symptoms
1. Nausea is a subjective sensation that is difficult to define. It is an unpleasant feeling in the abdomen often associated with the sense of being ill and the urge to vomit. Other related symptoms include increased salivation, loss of color, sweating, tachycardia (increased heart rate), and the urge to defecate.
D. Treatment
2. Medications
a) 5-HT3 antagonists
(3) Examples
(b) Granisetron (Kytril): Adults: 2 mg PO daily in single or divided doses (q12h) within 1 hour of chemotherapy on days chemotherapy is given
PATIENT PROFILE
Allergies: No known drug allergies (NKDA)
Alcohol use: Minimal, socially only
Exercise: Walking several days per week, some weight training
Levothyroxine 75 mcg PO once daily (hypothyroidism diagnosed 2 years ago, stable)
PATIENT PROFILE QUESTIONS
1. Certain patients with symptoms consistent with heartburn or gastroesophageal reflux (GERD) are not initial candidates for self-treatment. Which of the following are considered reasons for physician referral?
2. Which of the following would represent the BEST choice for an initial nonprescription (OTC) regimen for NB?
3. NB should also inform her physician of her use of a proton-pump inhibitor (PPI) at her next doctor visit, which is scheduled in 3 weeks. Why might she need to tell her doctor about her heartburn and treatment?
I. Both her choice of antacid (Tums) and a PPI could interfere with her levothyroxine prescription and the maintenance of euthryoid status.
REVIEW QUESTIONS
(Answers and Rationales on page 359.)
8. Which of the following statements is/are correct?
9. True or False: Increases in blood urea nitrogen (BUN) and serum creatinine (SCr) generally indicate liver damage.
10. Which of the following medications is indicated for treatment of chronic idiopathic constipation in adults?
19. Which of the following conditions requires consideration of the sodium, magnesium, or phosphate content of a laxative before administration?
27. Which of the following is no longer the most appropriate agent to use in the treatment of peptic ulcer disease?
37. Which of the following acts as a saline cathartic?
The following is a case study. Read the case study and answer the questions after.