Gastrointestinal disorders
Malabsorption
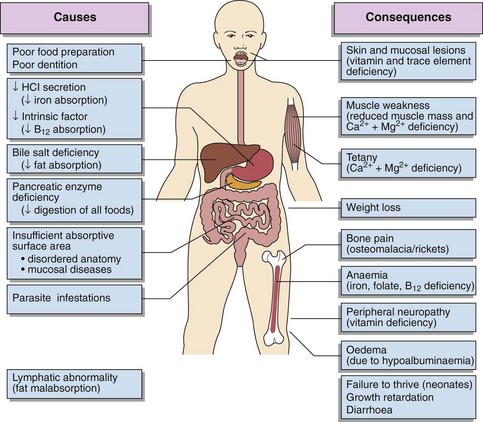
Failure of digestion is properly called maldigestion. The term ‘malabsorption’ describes impairment of the absorptive mechanisms, but in practice is used to encompass both disorders. Malabsorption is a condition that can occur at any stage of life from a variety of causes (Fig 56.1).
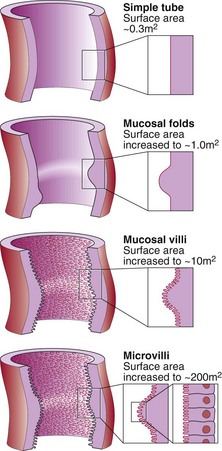
Figure 56.2 illustrates how the normal mucosal structure is designed to maximize absorptive capacity. While mucosal surface enzymes play an important role in digestion, the most important source of digestive enzymes is the exocrine pancreas. As with many other organs in the body, there is more than 50% reserve capacity in both the small intestine and exocrine pancreas. Thus, disorders in these organs are usually quite advanced before malabsorption can be detected by functional tests or is clinically manifest. As a result the role of functional tests of malabsorption has diminished and they have largely been abandoned.
Gastrointestinal disorders
Small intestine
The absorption of nutrients, which occurs at the mucosal microvillous surface of the enterocytes, is the major role of the small intestine (Fig 56.2).
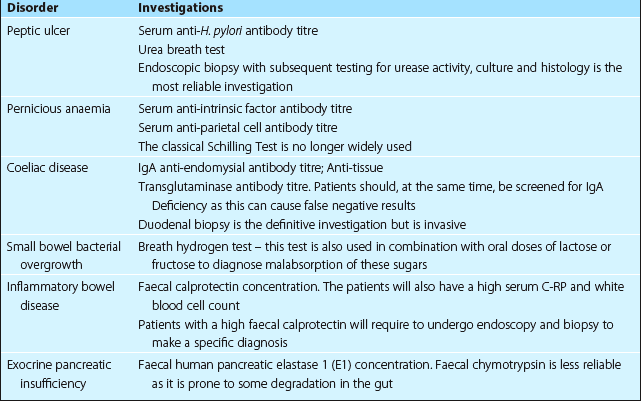
Mucosal disease is diagnosed by biopsy. Coeliac disease is the commonest cause of villous atrophy. The presence of auto-antibodies (Table 56.1) may indicate a likely diagnosis of coeliac disease but confirmation is made by biopsy.