chapter 30 Gastroenterology
COMMON PRESENTATIONS
ACUTE ABDOMINAL PAIN1,2
Nature of pain
Mechanisms of abdominal pain
Type and chronicity of pain
Biliary ‘colic’ is continuous rather than intermittent, in the epigastrium or RUQ.
GENERALISED ABDOMINAL PAIN
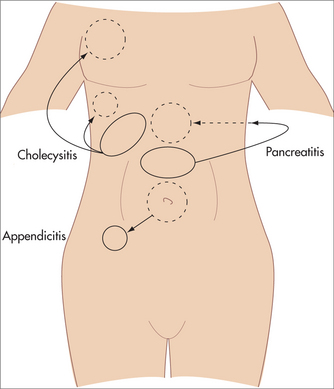
LOCALISED ACUTE ABDOMINAL PAIN
Left iliac fossa
CONSTIPATION
While the cause of constipation may be a simple matter of diet, drug side effect or behavioural bowel habit, constipation may be an indication of a serious underlying disorder.
Investigation
Therapeutics
DIARRHOEA
Acute diarrhoea
Investigation
Viral gastroenteritis/enteritis
Treatment
Bacterial gastroenteritis
Nausea, vomiting, diarrhoea and abdominal pain are common to most. Neurological, hepatic and renal complications can also occur. Rapid onset (hours) after ingestion of contaminated food suggests a pre-formed toxin, while a longer incubation period (1–3 days) suggests a bacterial or viral cause.
Enterotoxigenic E. coli
A leading cause of traveller’s diarrhoea. Adheres to the gut wall and produces enterotoxins.
Salmonella
Complications include osteomyelitis, bacteraemia, abscesses, meningitis and pneumonia.
Antibiotics are generally not advised.
If required, when disease is severe or patient is at risk of complications:
Shigella
Bacillus cereus
A form of food poisoning, usually related to ingestion of contaminated fried rice or rice that is cooked then improperly refrigerated, although a wide variety of foods have been implicated. Infection is associated with two distinct syndromes: a vomiting syndrome (ingestion of a pre-formed toxin) and a diarrhoeal syndrome resulting from the production of an enterotoxin.
Usually self-limiting over 20–36 hours, but will respond to quinolones if necessary.
Pseudomembranous colitis
Traveller’s diarrhoea
Common in visitors to developing countries. The most common pathogen is enterotoxigenic E. coli, although other pathogens can be responsible, including Shigella (10%), Salmonella (5%), Campylobacter (3%), Yersinia (2%), G. lamblia (4%), E. histolytica (1%), Cryptosporidium (3%) and viruses (3%).1
Treatment
Herbs and supplements for diarrhoea6
Ciguatera fish poisoning
Results from ingestion of a fish containing a neurotoxin (ciguatoxin) that originates in algae living in tropical waters, particularly the Pacific and Caribbean. Ciguatoxin is very heat resistant, so ciguatoxin-laden fish cannot be detoxified by conventional cooking. Symptoms start within 5 minutes to 30 hours of ingestion: nausea, vomiting, diarrhoea, photophobia, blurred vision, ataxia and paraesthesiae. Bradycardia, hypotension and heart block may occur. There is no proven effective treatment or antidote for ciguatera poisoning. The symptoms can last from weeks to years, and in extreme cases as long as 20 years, often leading to long-term disability.10 Most people do recover slowly over time. Often patients recover but redevelop symptoms in the future. Relapses can be triggered by consumption of nuts, alcohol, fish or fish-containing products, chicken or eggs, or by exposure to fumes such as those of bleach and other chemicals. Exercise is also a possible trigger.11
Chronic diarrhoea
Diagnosis
History and investigations are directed at finding a treatable cause of chronic diarrhoea.
Abdominal palpation, rectal examination and examination of stool are essential.
Investigations
If small bowel pathology is suspected, a Pillcam® (endoscopic capsule) may identify the cause.
A supervised exclusion diet may be helpful in cases of suspected food intolerance.
Therapeutics
Identify and treat any underlying cause.
Herbs
For relieving gut inflammation:
FAECAL INCONTINENCE
Faecal incontinence, or involuntary leakage of faecal material, is thought to occur in about 10% of adults but is reported in only one in eight cases.12 It can cause severe restriction of social interaction and lifestyle, and is a common precipitant for admission to residential aged care.
Investigations
GLOSSODYNIA (PAINFUL TONGUE)
Aetiology
HICCUPS
Aetiology
Persistent or intractable hiccups:
MOUTH ULCERS
Differential diagnosis
DYSPHAGIA
Aetiology
Diagnosis
Investigation
INDIGESTION, DYSPEPSIA AND HEARTBURN
Heartburn and regurgitation imply oesophageal disease and often occur together.
Symptoms of dyspepsia and GORD often overlap.
Causes of dyspepsia/indigestion
Investigation
GASTRO-OESOPHAGEAL REFLUX DISEASE
Aetiology
Therapeutics
First-line
NAUSEA AND VOMITING
Causes
Central nervous system disorders:
Metabolic and endocrine disorders:
Examination
Thorough physical examination is necessary to identify underlying causes for nausea and vomiting and to assess clinical consequences of vomiting, such as dehydration and malnutrition.
Therapeutics
HALITOSIS
Halitosis is an unpleasant odour on the breath that may be physiological or pathological (Box 30.1). Physiological causes may include ingestion of particular foods or medications. It is most commonly caused by action of microflora on oral debris around the teeth and gums. Gram-negative organisms cause putrefaction and release of chemicals, particularly sulfide compounds, in the alkaline oral environment.
BOX 30.1 Differential diagnosis of halitosis
The odour can vary depending on diet, time of day, time of menstrual cycle and state of hunger.
Treatment
Prevention
PERIANAL PAIN
Causes to consider are described below.