Hyperplastic, adenomatous, and hamartomatous

 in the duodenal bulb that is a prolapsed gastric antral polyp (adenoma).
in the duodenal bulb that is a prolapsed gastric antral polyp (adenoma).
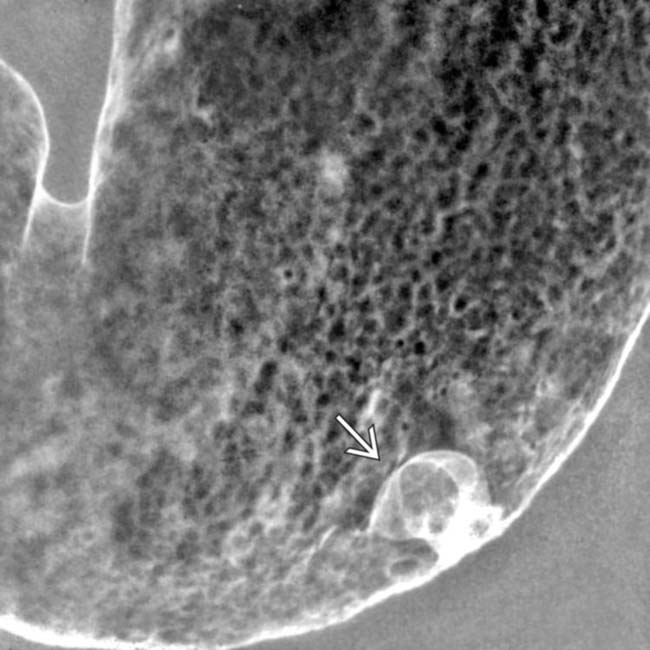
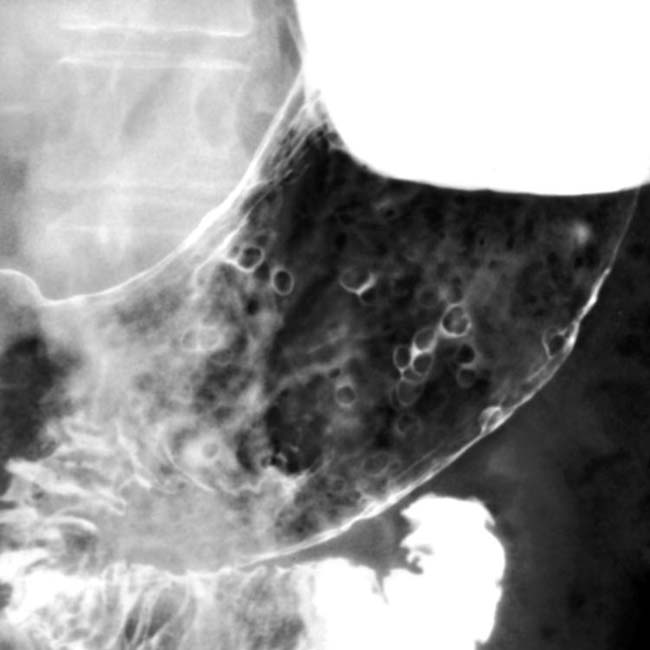
 in the gastric body. The appearance and age of the patient are typical for hyperplastic polyps.
in the gastric body. The appearance and age of the patient are typical for hyperplastic polyps.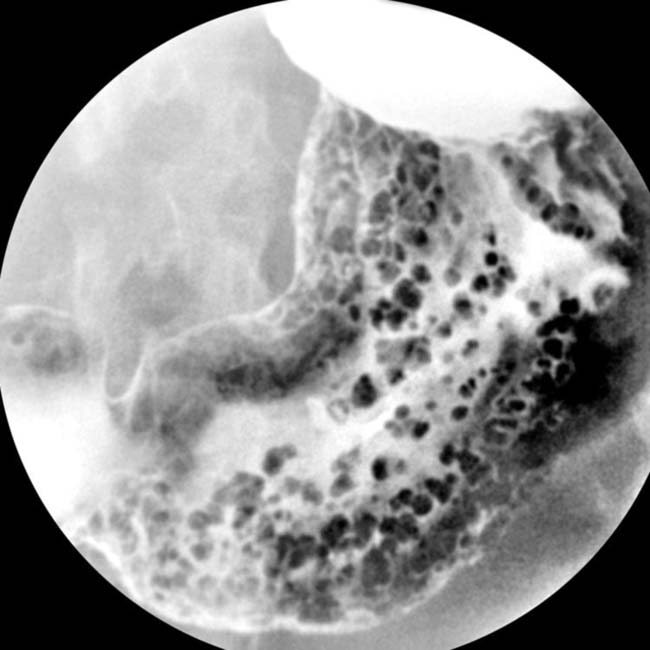
IMAGING
General Features
 at the GE junction.
at the GE junction.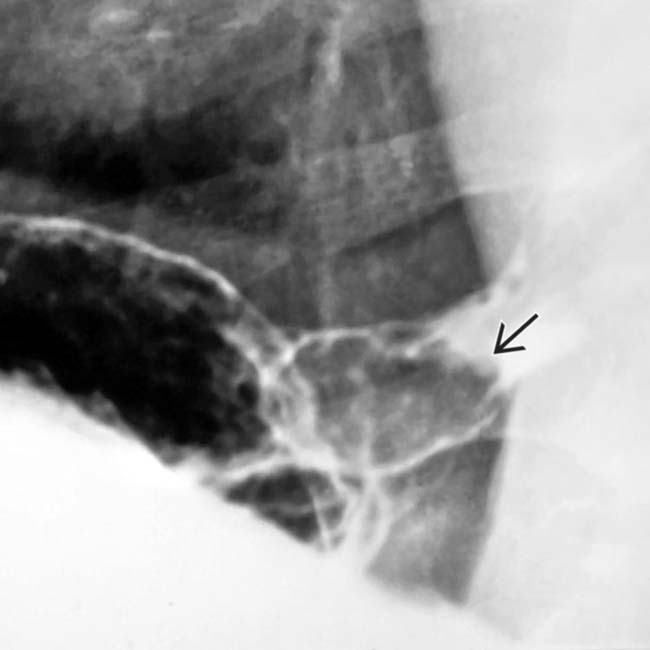
 prolapsing into the distal esophagus. Endoscopy and resection revealed an adenomatous gastric polyp.
prolapsing into the distal esophagus. Endoscopy and resection revealed an adenomatous gastric polyp.
 that was a benign adenoma. A band was placed around the base of the polyp, and it was resected at endoscopy.
that was a benign adenoma. A band was placed around the base of the polyp, and it was resected at endoscopy.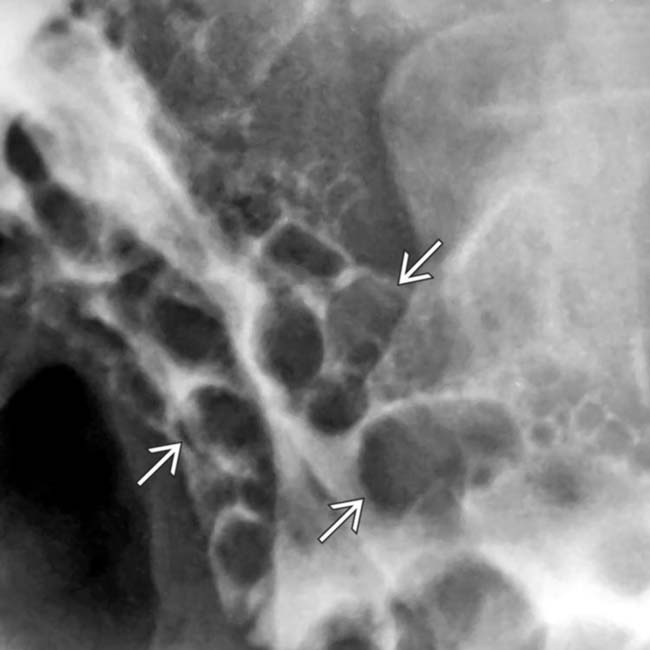
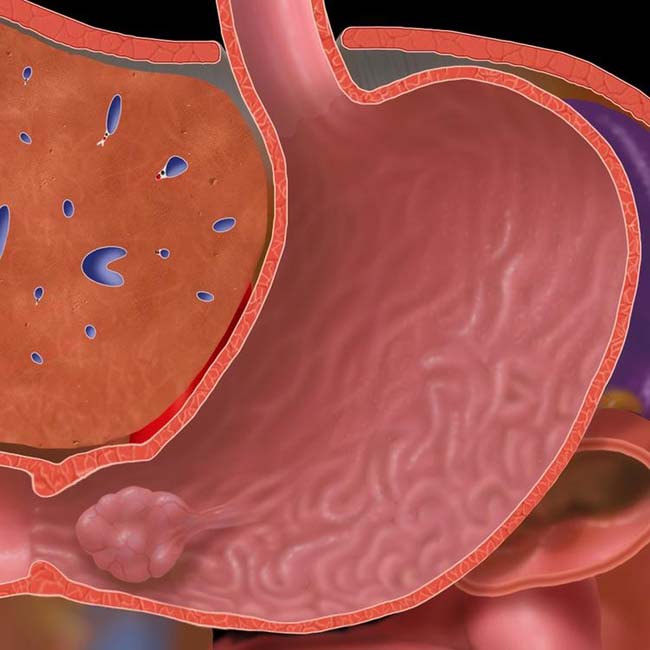
 arising from the gastric cardia and body. These have a smooth surface and most appear sessile.
arising from the gastric cardia and body. These have a smooth surface and most appear sessile.
 . Endoscopy revealed multiple polyps with a villous adenoma histology.
. Endoscopy revealed multiple polyps with a villous adenoma histology.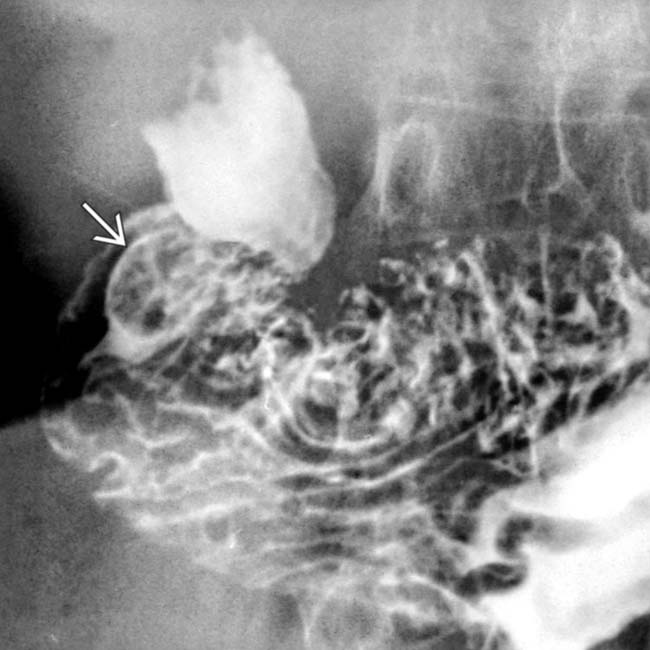
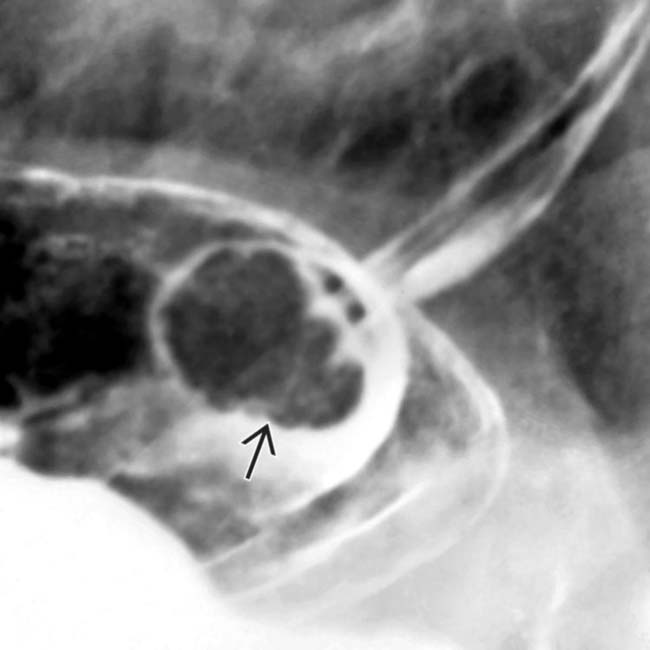
 in the antrum that periodically prolapsed through the pylorus. This case proved to be leiomyoma.
in the antrum that periodically prolapsed through the pylorus. This case proved to be leiomyoma.
































































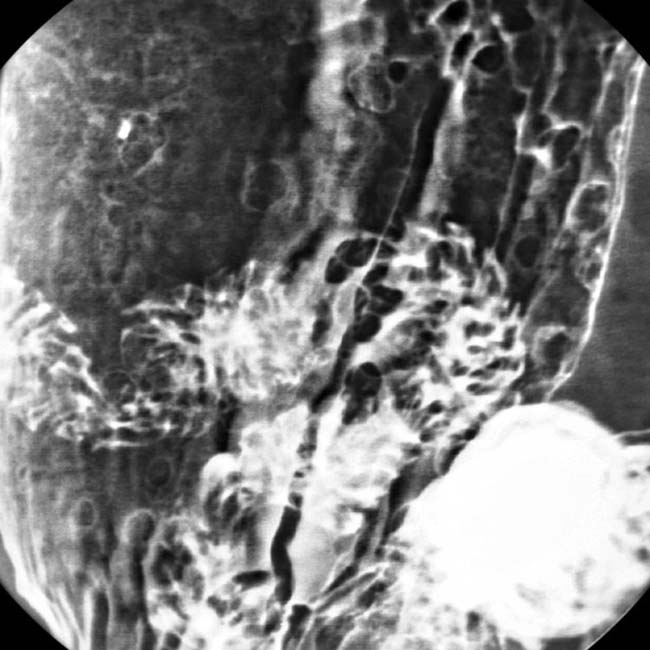
 in the gastric body.
in the gastric body.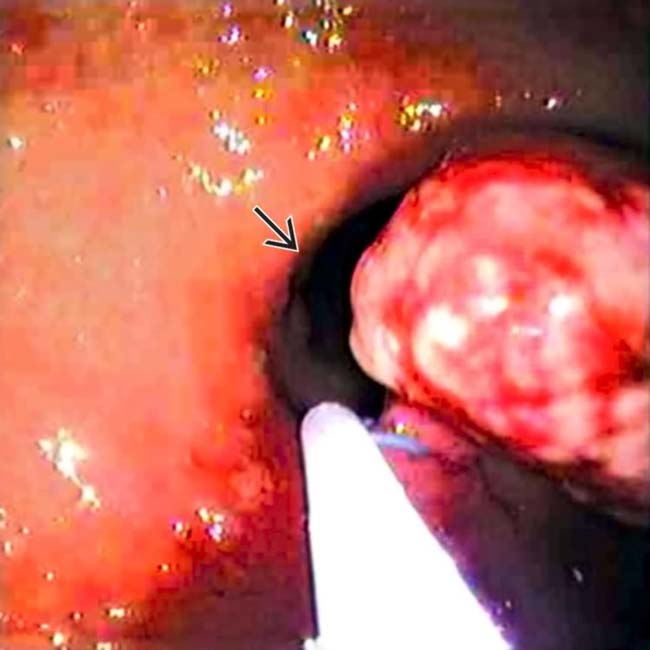
 .
.

 .
.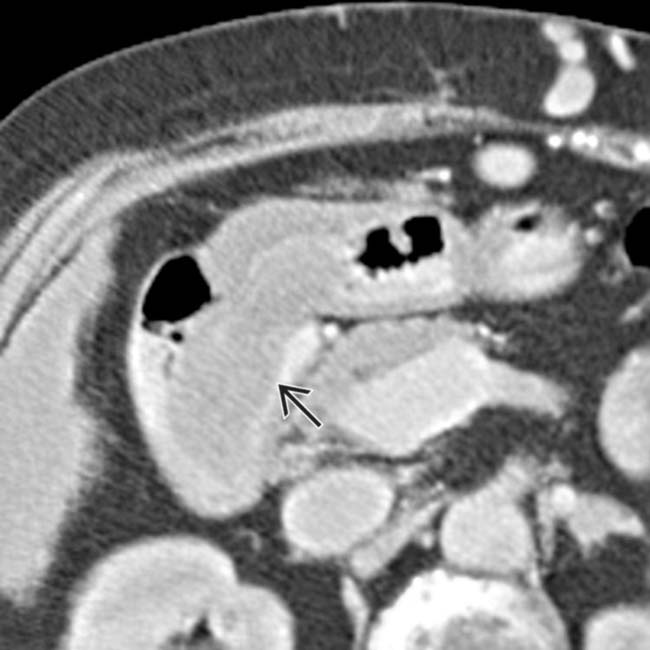
 prolapsed into the duodenum.
prolapsed into the duodenum.
