Phytobezoar: Undigested vegetable matter


IMAGING
General Features
CLINICAL ISSUES
Presentation
Natural History & Prognosis
• Bezoars of any type most often occur in background of altered motility or anatomy of gastrointestinal tract

 of the bezoar. Prior gastric surgery is a predisposing factor for developing a bezoar.
of the bezoar. Prior gastric surgery is a predisposing factor for developing a bezoar.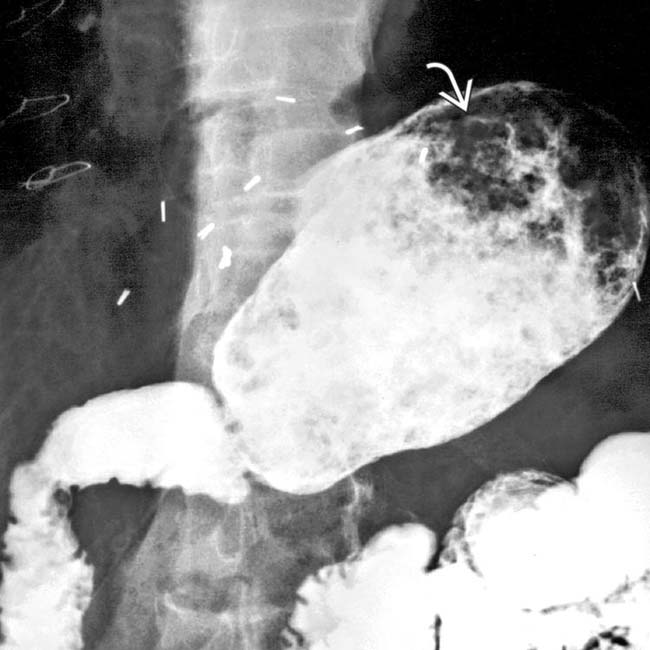
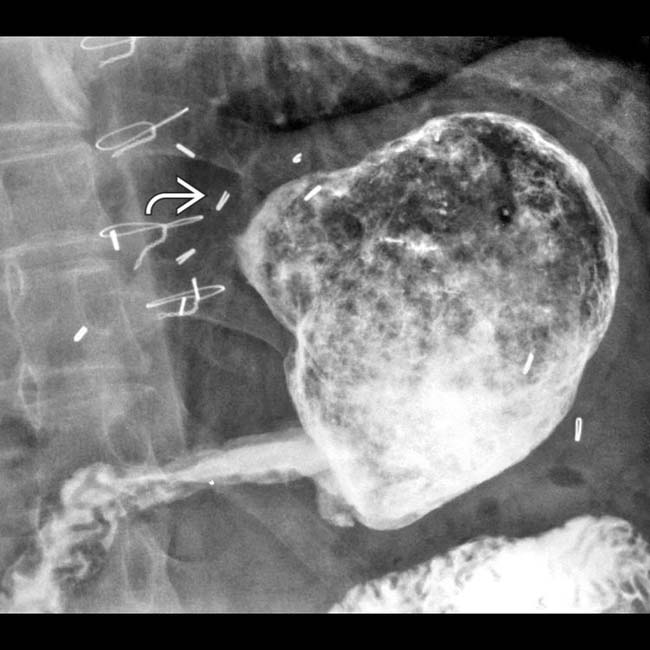
 in the stomach.
in the stomach.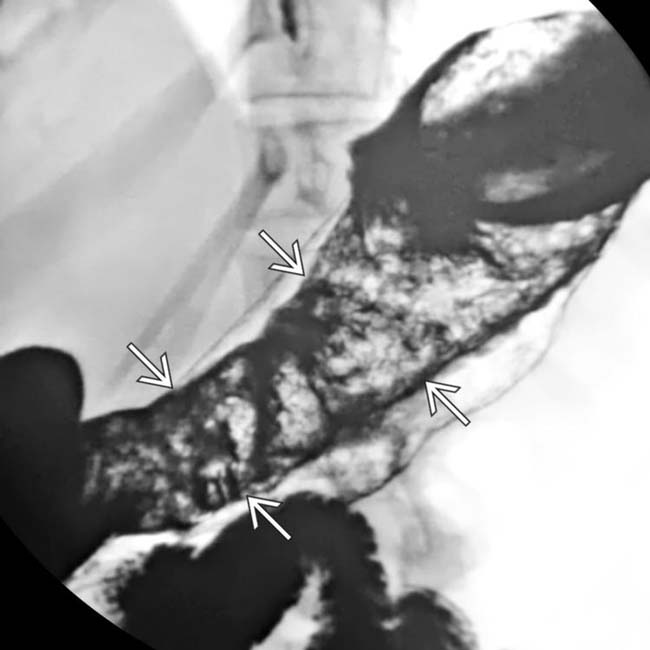
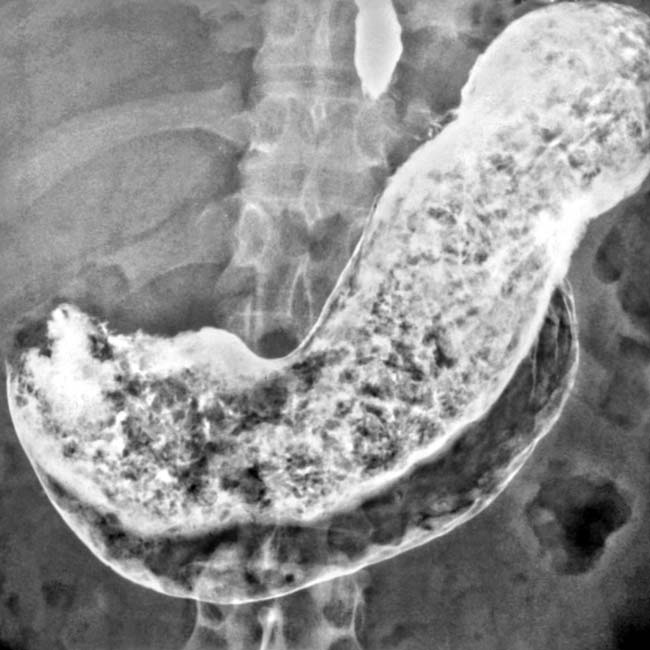
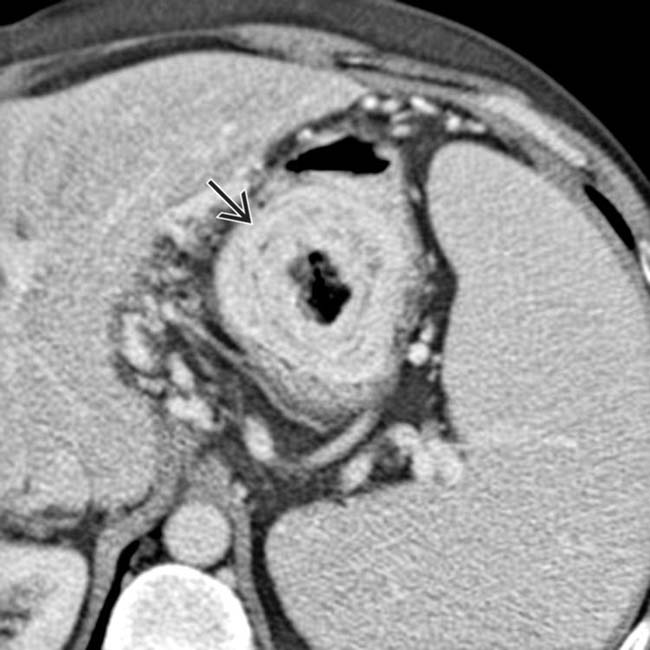
 corresponds to the shape of the stomach.
corresponds to the shape of the stomach.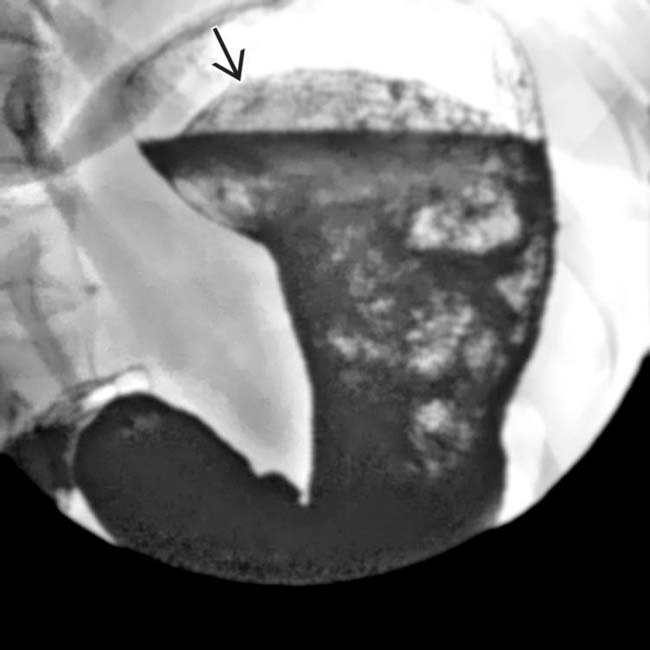
 within the stomach that conform to the shape of the stomach. Notice that the rounded top of the mass is floating within the stomach.
within the stomach that conform to the shape of the stomach. Notice that the rounded top of the mass is floating within the stomach.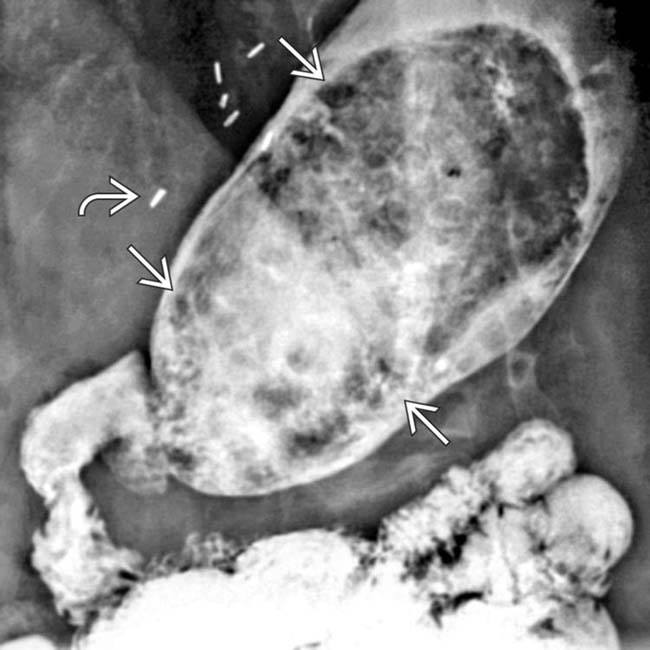
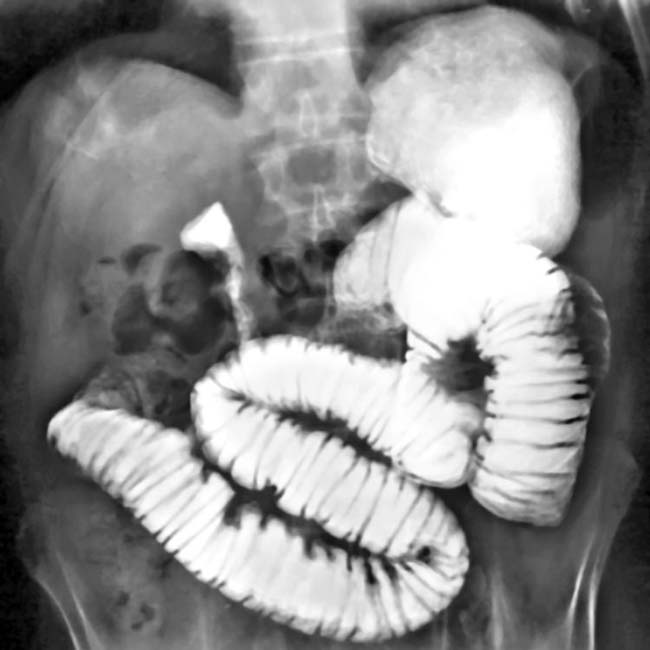
 from a vagotomy and the antrectomy with duodenal anastomosis (Billroth 1 procedure) are shown in a middle-aged man with phytobezoar. There is a solid mass
from a vagotomy and the antrectomy with duodenal anastomosis (Billroth 1 procedure) are shown in a middle-aged man with phytobezoar. There is a solid mass  with a gastric shape composed of gas and undigested plant material.
with a gastric shape composed of gas and undigested plant material.












 in the stomach due to a phytobezoar.
in the stomach due to a phytobezoar.





























































 as well as the bezoar.
as well as the bezoar.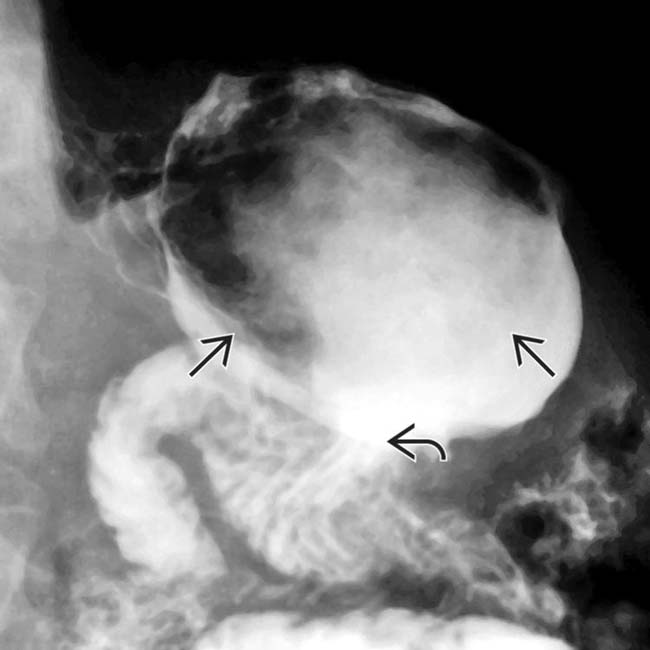
 . The bezoar
. The bezoar  is the fixed filling defect within the stomach.
is the fixed filling defect within the stomach.