Several different possible imaging appearances

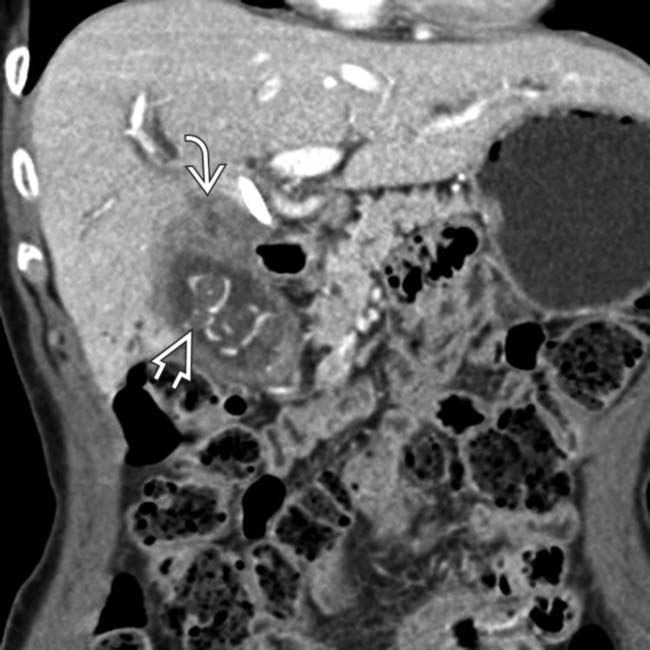
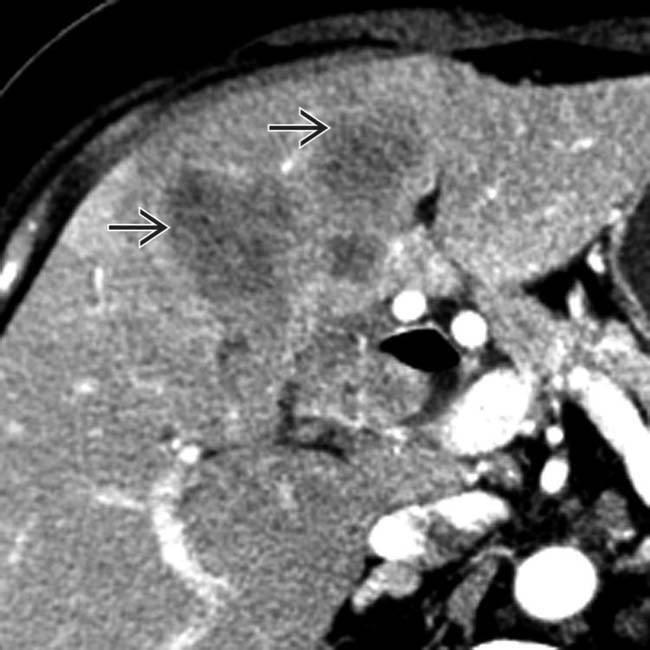
 arising from the GB and extending superiorly to invade the liver and porta hepatis. Note the presence of multiple gallstones
arising from the GB and extending superiorly to invade the liver and porta hepatis. Note the presence of multiple gallstones  , a known major risk factor for GB carcinoma.
, a known major risk factor for GB carcinoma.
 in the GB, in keeping with GB carcinoma. Such polyploid masses only account for roughly 20% of all GB cancers detected on CT.
in the GB, in keeping with GB carcinoma. Such polyploid masses only account for roughly 20% of all GB cancers detected on CT.
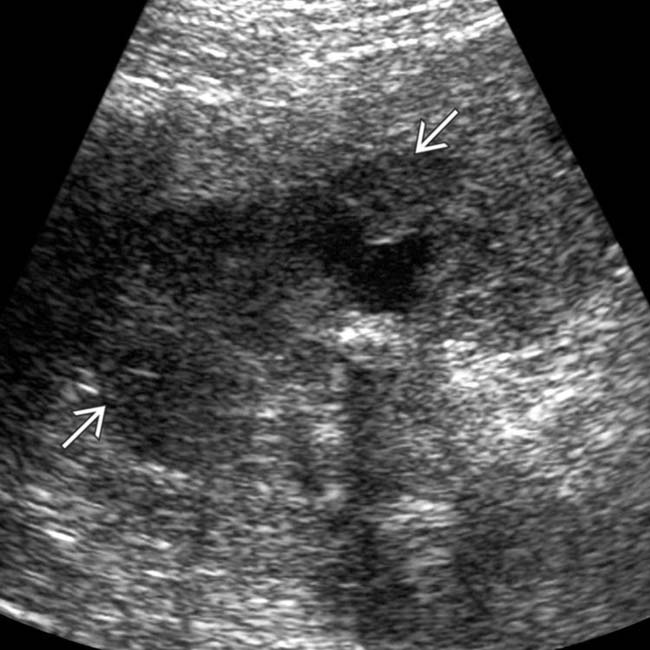
 filling the GB fundus, in keeping with a GB carcinoma. Note that the echogenic GB wall
filling the GB fundus, in keeping with a GB carcinoma. Note that the echogenic GB wall  is intact between the mass and liver, suggesting that there is no liver invasion.
is intact between the mass and liver, suggesting that there is no liver invasion.IMAGING
General Features
CT Findings
• Intraluminal polyploid GB mass (∼ 20% of cases), irregular focal or diffuse GB wall thickening (20-30% of cases), or mass completely replacing GB (2/3 of cases)
 May be difficult to differentiate from primary liver mass when large mass replaces GB and invades liver
May be difficult to differentiate from primary liver mass when large mass replaces GB and invades liver
 May be difficult to differentiate from Klatskin tumor (cholangiocarcinoma) when tumor invades porta hepatis
May be difficult to differentiate from Klatskin tumor (cholangiocarcinoma) when tumor invades porta hepatis
 GB cancer presenting as wall thickening (especially when diffuse) difficult to differentiate from chronic cholecystitis; look for irregular wall thickening, metastases, and locoregional enlarged lymph nodes
GB cancer presenting as wall thickening (especially when diffuse) difficult to differentiate from chronic cholecystitis; look for irregular wall thickening, metastases, and locoregional enlarged lymph nodes
 May be difficult to differentiate from primary liver mass when large mass replaces GB and invades liver
May be difficult to differentiate from primary liver mass when large mass replaces GB and invades liver May be difficult to differentiate from Klatskin tumor (cholangiocarcinoma) when tumor invades porta hepatis
May be difficult to differentiate from Klatskin tumor (cholangiocarcinoma) when tumor invades porta hepatis GB cancer presenting as wall thickening (especially when diffuse) difficult to differentiate from chronic cholecystitis; look for irregular wall thickening, metastases, and locoregional enlarged lymph nodes
GB cancer presenting as wall thickening (especially when diffuse) difficult to differentiate from chronic cholecystitis; look for irregular wall thickening, metastases, and locoregional enlarged lymph nodesDIFFERENTIAL DIAGNOSIS
Complicated or Chronic Cholecystitis
PATHOLOGY
General Features
• Etiology
 Risk factors (mostly related to chronic GB inflammation): Cholelithiasis, chronic cholecystitis, chronic infection (Salmonella), porcelain GB, GB polyps, abnormal pancreaticobiliary duct junction (seen with choledochal cysts), obesity
Risk factors (mostly related to chronic GB inflammation): Cholelithiasis, chronic cholecystitis, chronic infection (Salmonella), porcelain GB, GB polyps, abnormal pancreaticobiliary duct junction (seen with choledochal cysts), obesity
 Risk factors (mostly related to chronic GB inflammation): Cholelithiasis, chronic cholecystitis, chronic infection (Salmonella), porcelain GB, GB polyps, abnormal pancreaticobiliary duct junction (seen with choledochal cysts), obesity
Risk factors (mostly related to chronic GB inflammation): Cholelithiasis, chronic cholecystitis, chronic infection (Salmonella), porcelain GB, GB polyps, abnormal pancreaticobiliary duct junction (seen with choledochal cysts), obesity
CLINICAL ISSUES
Presentation
Treatment
• Stage I or II (T1-T2, N0, M0) tumors resectable with curative intent; stage III tumors (T3 or T1-2, N1) usually (but not always) unresectable; stage IV almost always unresectable (T4 or N2 or M1)

 and the adjacent descending duodenum
and the adjacent descending duodenum  . If considered resectable, such a cancer would undoubtedly require an extended cholecystectomy with radical resection.
. If considered resectable, such a cancer would undoubtedly require an extended cholecystectomy with radical resection.
 directly invading the liver
directly invading the liver  . In many cases, such as this, the site of origin for the mass can be difficult to determine.
. In many cases, such as this, the site of origin for the mass can be difficult to determine.
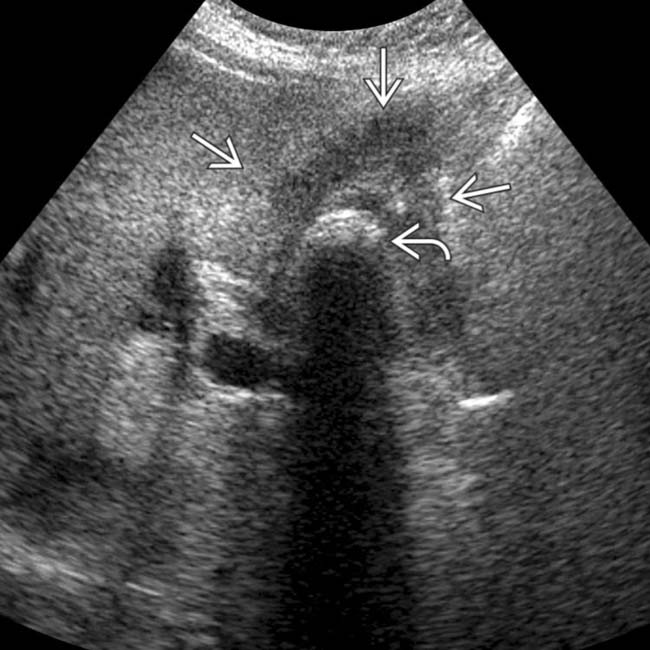
 and a shadowing stone
and a shadowing stone  . The mass is inseparable from the adjacent liver. CT (not shown) demonstrated local invasion of the central liver by GB carcinoma.
. The mass is inseparable from the adjacent liver. CT (not shown) demonstrated local invasion of the central liver by GB carcinoma.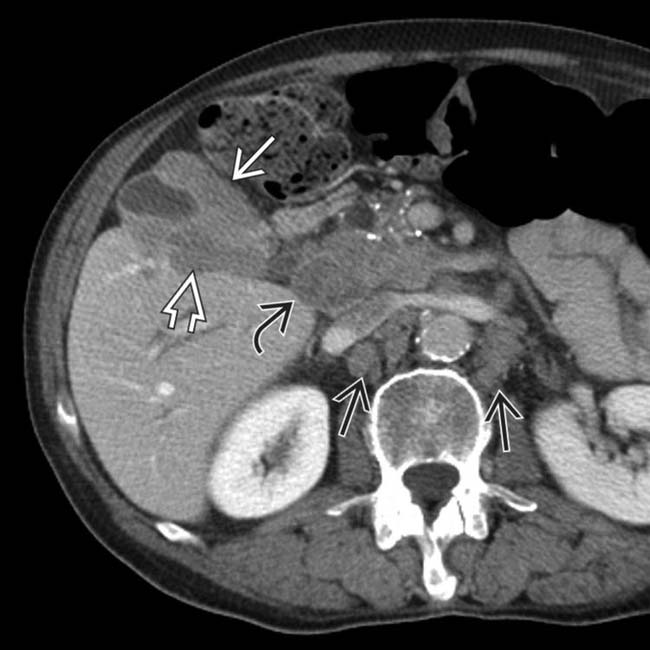
 , direct liver invasion
, direct liver invasion  , and peripancreatic/portocaval
, and peripancreatic/portocaval  and retroperitoneal
and retroperitoneal  adenopathy. Bulky lymphadenopathy in these locations is typical for GB carcinoma.
adenopathy. Bulky lymphadenopathy in these locations is typical for GB carcinoma.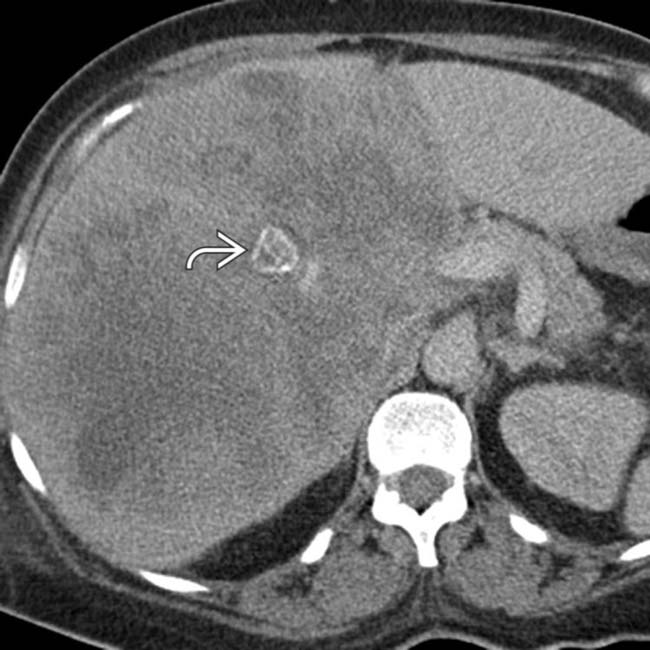
 at its center and the failure to visualize a GB. This was a GB cancer with extensive invasion of the liver.
at its center and the failure to visualize a GB. This was a GB cancer with extensive invasion of the liver.
 . The GB is also seen
. The GB is also seen  .
.
 .
.
 .
.
 and infiltrating along the portal vein
and infiltrating along the portal vein  .
.
 extending from the GB wall and invading the right lobe of the liver.
extending from the GB wall and invading the right lobe of the liver.
 .
.
 . Direct extension of GB carcinoma into the liver precludes surgical resection.
. Direct extension of GB carcinoma into the liver precludes surgical resection.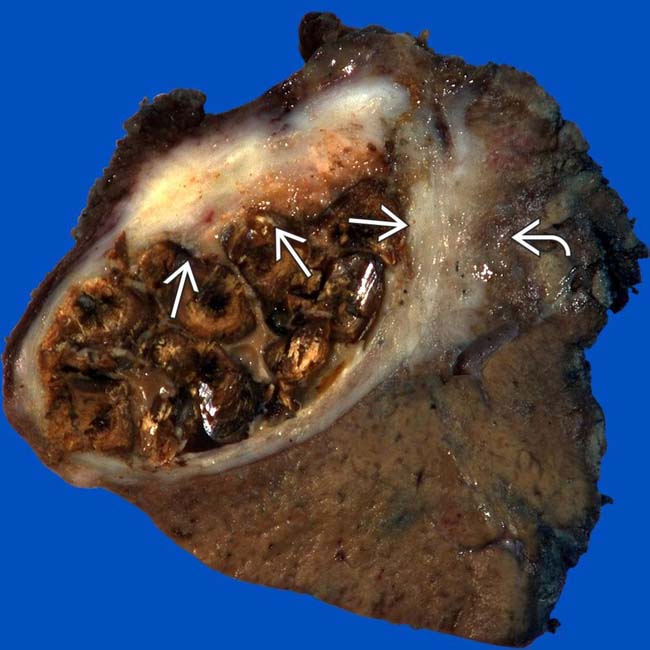
 and direct invasion of the adjacent liver by tumor
and direct invasion of the adjacent liver by tumor  , a typical pattern of local spread of GB carcinoma. The GB lumen is filled with stones.
, a typical pattern of local spread of GB carcinoma. The GB lumen is filled with stones.
































































 , several adjacent partially calcified stones
, several adjacent partially calcified stones  , and focal invasion of the medial segment
, and focal invasion of the medial segment  .
.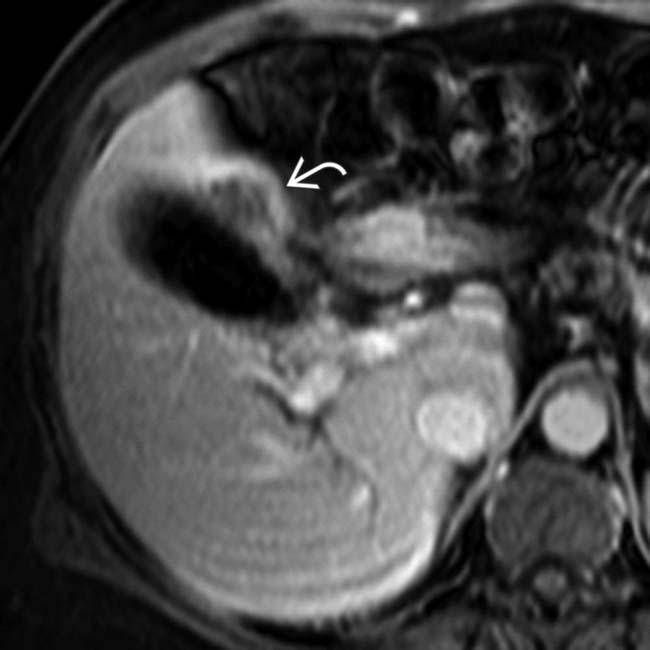
 . Recent work has suggested that delayed enhanced MR may play a role in staging early-stage (T1, T2) disease, although most patients with GB carcinoma present with at least transerosal (T3) tumor, as in this case.
. Recent work has suggested that delayed enhanced MR may play a role in staging early-stage (T1, T2) disease, although most patients with GB carcinoma present with at least transerosal (T3) tumor, as in this case.

