G
GABA See neurotransmitter.
galilean telescope See telescope, galilean.
galvanic nystagmus See nystagmus.
ganciclovir See antiviral agents.
ganglion An aggregation of nerve cell bodies found in numerous locations in the peripheral nervous system. Plural: ganglia.
ciliary g. A small reddish-grey body about the size of a pinhead situated at the posterior part of the orbit about 1 cm from the optic foramen between the optic nerve and the lateral rectus muscle. It receives posteriorly three roots: (1) the long, nasociliary or sensory root (or ramus communicans), which contains sensory fibres from the cornea, iris and ciliary body and some sympathetic postganglionic axons going to the dilator muscle; (2) the short (or motor root or oculomotor root) which comes from the Edinger–Westphal nucleus through the third nerve (oculomotor). It carries fibres supplying the sphincter pupillae and ciliary muscles; (3) the sympathetic root, which comes from the cavernous and the internal carotid plexuses. It carries fibres mediating constriction of the blood vessels of the eye and possibly mediating dilatation of the pupil. The ciliary ganglion gives rise to 6–10 short ciliary nerves. Syn. lenticular ganglion; ophthalmic ganglion.
See reflex, pupil light.
gasserian g. Sensory ganglion of the fifth nerve located in a bony fossa on the front of the apex of the petrous temporal bone. It receives the sensory portion of the fifth nerve (trigeminal) in the posterior part of the ganglion. From its anterior part the three divisions of the fifth nerve are given off: the ophthalmic (which contains the sensory fibres from the cornea and the eye in general), the maxillary and the mandibular nerves. Syn. semilunar ganglion; trigeminal ganglion.
See herpes zoster ophthalmicus.
lenticular g.; ophthalmic g. See ganglion, ciliary.
semilunar g. See ganglion, gasserian.
superior cervical g. One of the uppermost and largest ganglion in the two chains of sympathetic ganglia lying alongside the vertebral column. It is located just below the base of the skull between the internal carotid artery and the internal jugular vein. It gives rise to the internal carotid nerve, which forms the internal carotid plexus.
trigeminal g. See ganglion, gasserian.
gangliosidosis See disease, Sandhoff’s; disease, Tay–Sachs.
ganzfeld A visual stimulus that consists of completely homogeneous and colourless luminance conditions throughout. It is used especially when recording the standard electroretinogram.
gap junction See synapse.
Gardner Reversal-Frequency Test See test, developmental and perceptual screening.
gasserian ganglion See ganglion, gasserian.
gaussian approximation See ray, paraxial.
gaussian optics See optics, paraxial.
gaussian points See points, cardinal.
gaussian space See paraxial region.
gaussian theory See theory, gaussian.
gaze To fixate steadily or continuously.
See cardinal positions of gaze.
gene The unit of heredity which determines, or contributes to, one inherited feature of an organism (e.g. eye colour). Physically, a gene is composed of a defined DNA sequence, located at a specific place (locus) along the length of a chromosome and transmitted by a parent to its offspring. The DNA sequence of nucleotide bases (adenine, cytosine, guanine and thymine) encodes a specific sequence of amino acids corresponding to a particular protein. If the DNA sequence at one locus is identical on a pair of homologous chromosomes the organism is referred to as homozygous (homozygote) and if the DNA sequence is not identical it is referred to as heterozygous (heterozygote). The total effect of all genes influences the development and functioning of all organs and systems in the body.
See chromosome; genome; inheritance; mutation; pedigree.
gene-environment interaction A term used to indicate that an effect is due to a mixture of environmental factors (nurture) and genetic factors (nature). Most traits show gene-environment interactions, such as myopia, IQ test results, skin colour etc. Blood type and iris colour are predominantly genetically transmitted, whereas language is predominantly environmental.
See theory, biological-statistical; theory, nativist.
gene therapy A therapeutic method in which a defective gene is replaced by a normal copy of itself, thus restoring its function. There are several ways in which a new gene is carried into a diseased cell. A common method uses a retrovirus, an adenovirus or an adeno-associated virus as vectors to introduce genes into cells and DNA. This therapy has been used in the treatment of several eye diseases, especially retinoblastoma and retinitis pigmentosa, but so far with limited success.
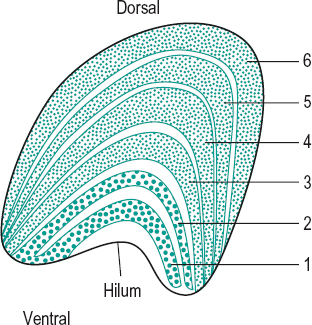
geniculate body, lateral (LGB) Ovoid protuberances lateral to the pulvinar of the thalamus in the diencephalon of the forebrain and into which the fibres of the optic tract synapse on their way to the visual cortex. However, because of the semidecussation of the optic nerve fibres in the optic chiasma, the lateral geniculate body in the right thalamus receives the fibres originating on the temporal retina of the right eye and the nasal fibres of the left. Each body appears, in cross-section, to consist of alternating white and grey areas. The white areas are formed by the medullated nerve fibres of the optic tract, while the grey areas consist largely of the nerve cells in which the fibres of the optic tract terminate (synapses) and from which arises the fibres of the optic radiations. There are six grey areas or layers of cells, with layer 1 being the most ventral and layer 6 the most dorsal (or posterior). Layers 1, 4 and 6 receive the crossed or nasal fibres from the contralateral retina, while layers 2, 3 and 5 receive the uncrossed or temporal fibres of the ipsilateral retina. The neural components of the LGB without the blood vessels and covering layer form the lateral geniculate nucleus (LGN).
There are two main types of cells in the LGN: in layers 1 and 2 (those most ventral) the cells are substantially larger than in the other four layers and are called magno cells and the layers, magnocellular layers. The main input to these cells are the retinal rods and the magno ganglion cells. In the other four layers (those most dorsal) the cells are smaller and are called parvo cells and the layers, parvocellular layers. The main input to these cells are the retinal cones and the parvo ganglion cells. The cells of the parvocellular layers seem to be mainly responsible for transmitting information about visual acuity, form vision, colour perception and low contrast targets. The cells in the magnocellular layers seem to be mainly responsible for transmitting information about motion and flicker perception, stereopsis and high contrast targets. The magnocellular and parvocellular cells project to different cells in the primary visual cortex (V1), where they retain the same segregation as in the lateral geniculate bodies. The receptive fields of the cells in the LGN are circular with either an ‘on’ or ‘off’ centre with the opposite behaviour in the surround, but they are more sensitive to contrast than the retinal ganglion cells (Fig. G1).
See brachium; cell, M; cell, P;fibres, visual; pathway, visual.
general refraction formula See paraxial equation, fundamental.
geniculocalcarine tract See radiations, optic.
geniculostriate pathway See pathway, geniculostriate.
Gennari, line of See line of Gennari.
genome The complete set of genes in an individual. In humans it is estimated at approximately 30 000 genes and over three billion base pairs (two nucleotides joined together across a double helix) of DNA.
genotype The complete genetic constitution of an individual at a particular location (locus) in the genome. At many locations (loci) throughout the genome, the chromosomal DNA sequence differs subtly between individuals. Each of the various DNA sequences at one locus is called an allele: for instance, if there are three sequence variants present, then there are three alleles. Offspring inherit one homologous chromosome from each parent. Thus, a genotype comprises two alleles: the allele inherited from the father (carried on the paternal chromosome) and the allele inherited from the mother (carried on the maternal chromosome).
gentamicin See antibiotic.
geometrical axis; optics See under the nouns.
gerontoxon See corneal arcus.
Gerstmann syndrome See syndrome, Gerstmann.
giant cell arteritis See arteritis, temporal.
giant papillary conjunctivitis See conjunctivitis, giant papillary.
giantophthalmos Megalocornea associated with an enlargement of the anterior segment of the eye.
See keratoglobus.
Giles–Archer lantern See test, lantern.
glabella 1. A prominent area of the frontal bone situated above the root of the nose. 2. The skin between the eyebrows, which is usually hairless. Syn. intercilium.
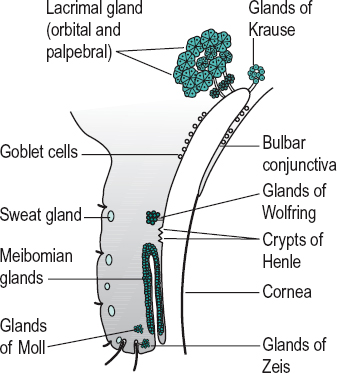
gland An aggregation of cells which secretes or excretes a substance. There are two main groups of glands: (1) The endocrine glands which have no duct and whose secretion (a hormone) is absorbed directly into the blood. Examples: adrenal gland, pineal gland, pituitary gland, thyroid gland. (2) The exocrine glands whose secretion reaches the surface by means of ducts. There are three main types of secretion by exocrine glands: the serous glands which secrete a watery substance rich in proteins (e.g. lacrimal gland, sweat glands), the mucous glands which secrete mucus, a viscous product (e.g. goblet cells), and the sebaceous glands which secrete a lipid substance (e.g. meibomian glands).
accessory lacrimal g’s. They are the glands of Krause and Wolfring. These glands are histologically identical to the main lacrimal gland, but are located within the eyelids. These glands are responsible for basal (not reflex) tear secretion and appear to be under sympathetic neural control.
g’s. of Ciaccio See glands of Wolfring.
ciliary sebaceous g’s. See glands of Zeis.
ciliary sweat g’s. See glands of Moll.
conjunctival g. Any gland that secretes a substance into the conjunctiva, such as the lacrimal, meibomian, Krause and Wolfring glands or a goblet cell.
g’s. of Henle These are not really glands. They are folds in the mucous membrane of the palpebral conjunctiva, situated between the tarsal plates and the fornices, in which there are goblet cells (Fig. G2). Syn. crypts of Henle (strictly speaking this term refers only to the pit-like depressions).
g’s. of Krause Accessory lacrimal glands of the conjunctiva having the same structure as the main lacrimal gland. They are located in the subconjunctival connective tissue of the fornix, especially the superior fornix (Fig. G2).
lacrimal g. A compound gland situated above and to the outer side of the globe of the eye. It consists of two portions: (1) a large orbital or superior portion; and (2) a small palpebral or inferior portion. It secretes the
See dacryoadenitis; dacryops; fossa for the lacrimal gland; nerve, zygomatic; tear duct.
g’s. of Manz Tiny glands located near the limbus. They secrete mucin. The existence of these glands in man is not established.
meibomian g’s. Sebaceous glands located in the tarsal plates of the eyelids whose ducts empty into the eyelid margin. They are arranged parallel with each other, perpendicular to the lid margin, about 25 for the upper lid and 20 for the lower. They secrete sebum. This sebaceous material provides the outermost oily (or lipid) layer of the precorneal tear film. It prevents the lacrimal fluid from overflowing onto the outer surface of the eyelid. It also makes for an airtight closure of the lids and prevents the tears from macerating the skin. The meibomian glands can be seen showing through the conjunctiva of fair-skinned people as yellow streaks (Fig. G2). Meibomian gland dysfunction (MGD) may be induced by blepharitis, chalazion, contact lens wear (particularly soft lenses) and ageing. The most common sign is a cloudy or absent secretion upon expression with symptoms of a mild dry eye. Hot compresses and lid massage will cure more than half of the patients; oral tetracycline will help in many of the others. Syn. palpebral follicles; tarsal glands.
See blepharitis, posterior; chalazion; film, precorneal; hordeolum, internal; keratoconjunctivitis sicca; meibomianitis; tarsus; Tearscope plus.
g’s. of Moll Sweat glands of the eyelids. They are situated in the region of the eyelashes (Fig. G2). Syn. ciliary sweat glands.
tarsal g’s. See glands, meibomian.
g’s. of Wolfring Accessory lacrimal glands of the upper eyelid situated in the region of the upper border of the tarsus (Fig. G2). Syn. glands of Ciaccio.
g’s. of Zeis Sebaceous glands of the eyelids which are attached directly to the follicles of the eyelashes. Their secretion contributes to the oily layer of the precorneal film (Fig. G2). Syn. ciliary sebaceous glands.
See blepharitis, marginal; hordeolum.
glare A visual condition in which the observer feels either discomfort and/or exhibits a lower performance in visual tests (e.g. visual acuity or contrast sensitivity). This is produced by a relatively bright source of light (called the glare source) within the visual field. A given bright light may or may not produce glare depending upon the location and intensity of the light source, the background luminance, the state of adaptation of the eye or the clarity of the media of the eye.
direct g. Glare produced by a source of light situated in the same or nearly the same direction as the object of fixation.
disability g. Glare which reduces visual performance without necessarily causing discomfort.
discomfort g. Glare which produces discomfort without necessarily interfering with visual performance.
eccentric g. See glare, indirect.
indirect g. Glare produced by an intense light source situated in a direction other than that of the object of fixation. Syn. eccentric glare.
g. source See glare.
g. tester An instrument for measuring the effect of glare on visual performance. There exist several (e.g. Brightness Acuity Tester (BAT), Miller–Nadler Glare Tester, Optec 1500 Glare Tester). Glare testing is valuable in patients with corneal and lenticular opacities before and after surgery and in elderly patients in whom adaptation to glare is usually more difficult. The Miller–Nadler Glare Tester consists of a glare source surrounding a Landolt C. The instrument contains 19 black Landolt C, all of the same size, 6/120 (or 20/400). Each Landolt C is presented in one of four orientations and from the highest to the lowest contrast at which the subject can no longer judge in which direction the letter appears. The contrast threshold is expressed in percentage disability glare.
The Brightness Acuity Tester (BAT) is a standardized glare source of light. It is presented in a hemisphere held over one eye. The light source can subtend a visual angle of 8 to 70 degrees at a vertex distance of 12 mm. The patient is asked to read a visual acuity chart through a small aperture in the hemisphere. The chart can be a low-contrast or high-contrast log MAR visual acuity chart or, for example, the Pelli–Robson contrast sensitivity chart.
veiling g. Glare caused by scattered light and producing a loss of contrast.
Glasgow acuity cards A visual acuity test composed of a set of cards contained in a flip card format. There are four letters on each card subtending the same visual angle, and of equal legibility. The progression of letter sizes from one card to the next is linear using a logarithmic scale, and the four letters are surrounded by a rectangle providing horizontal and vertical contour interaction. The test is performed at 3 m and is designed for children from three years of age and is particularly adapted for the management of amblyopia. Syn. log MAR crowded test.
glass 1. Material from which lenses and optical elements may be made. It is hard, brittle and lustrous and usually transparent. It is produced by fusing sand (silica) at about 1400°C with various oxides (potassium, sodium, etc.) and other ingredients such as lead oxide, lime, etc. Glass may be produced in various colours by the addition of different substances (e.g. metal oxides). 2. A lens.
See annealing; feathers; lens blank; strain; stria; surfacing.
absorption g. Glass which transmits only a certain portion of the incident light, the rest being absorbed.
Bagolini’s g. A plano lens on which fine parallel striations have been grooved. It produces a slight reduction in acuity but a punctate light source observed through this lens appears as a streak of light orientated at 90° from the striations. Two such lenses placed in front of the eyes with the striations oriented 90° apart are used to detect sensory and motor anomalies such as, retinal abnormal correspondence, suppression, etc. Syn. Bagolini’s lens; Bagolini’s striated glass.
See test, Bagolini lens.
cobalt-blue g. See lens, cobalt.
crown g. Glass characterized by low dispersion. The most commonly used crown glass in ophthalmic lenses, called ophthalmic crown or spectacle crown, has a refractive index n = 1.523 and a constringence or V-value of 59. There are other types of crown glass (e.g. dense barium crown n = 1.623, V-value 56; fluor crown n = 1.485, V-value 70).
g. cutter A tool with a diamond-tipped edge or hard steel to cut glass.
depolished g. See glass, ground.
flint g. Glass containing lead or titanium besides the usual ingredients and having a high dispersion (example: Tital, V-value 31) compared with crown glass and a high refractive index (n = 1.701). It is, however, a softer and heavier material than crown. It is used in ophthalmic lenses of high power as it can be made much thinner than a crown glass lens of the same power.
See doublet; lens, high index; triplet.
ground g. Glass that has been ground with emery, sandblasted or etched with fluoric acid to give it a matt surface. Such glass is usually translucent but not transparent. Syn. depolished glass.
magnifying g. See lens, magnifying.
opal g. A white or milky translucent glass used to diffuse light.
photochromic g. See lens, photochromic.
safety g. 1. Glass that has been ground and polished and then heated just below its softening point and rapidly cooled. Such treatment renders the glass highly resistant to fracture, and breakage causes it to crumble rather than shatter. Safety glass can also be produced chemically. In this process the lens is immersed in a molten salt bath (e.g. 99.5% potassium nitrate and 0.5% silicic acid at a temperature of 470°C for some 16 hours). The lens surface thus becomes compressed as larger potassium ions replace the smaller sodium ions which are in the glass. Chemically strengthened lenses have greater impact resistance and can be made thinner than air-tempered glass lenses. However, when broken the fragments of the chemically strengthened lenses are not as blunt as those of air-tempered glass lenses. Syn. toughened glass. 2. Non-shatterable laminated glass used in automobiles and goggles.
See lens, safety; polariscope; spectacles, industrial.
toughened g. See glass, safety.
glasses See spectacles.
glasses, field See binoculars.
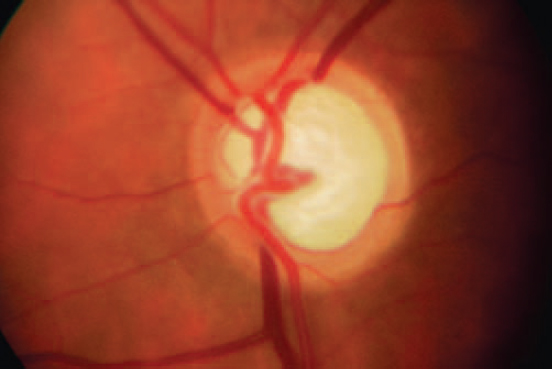
glaucoma A progressive neuropathy which leads to retinal ganglion cell death and optic nerve atrophy. Glaucoma is characterized by optic disc cupping and visual field defects, usually associated with elevated intraocular pressure. It is commonly divided into open-angle and angle-closure types. If the cause of the glaucoma is a recognized ocular disease or injury (e.g. corneal laceration), it is called secondary, whereas if the cause is unknown it is called primary. Glaucoma is present in about 1% of the Caucasian population over the age of 40 years and about 3% over the age of 70 years, but these figures vary among different populations, tending to be lower in white populations and higher in non-white populations.
See atrophy, optic; cup, glaucomatous; field, visual expander; neuroprotection; ratio, cup-disc; syndrome, Marfan’s; syndrome, Sturge–Weber; tritanopia.
absolute g. Final stage of the disease which has been either untreated or unsuccessfully treated. The eye is blind and hard, the optic disc is white and the pupil dilated.
acute angle-closure g. (AACG) A form of raised intraocular pressure in which the pressure within the eye increases rapidly due to blockage of the trabecular meshwork. Symptoms include: intense pain, redness, blurred vision, haloes around lights, as well as nausea. Findings on examination include: reduced visual acuity, greatly elevated intraocular pressure (in the range of 40–50 mmHg), corneal epithelial oedema, semi-dilated and fixed pupil, shallow anterior chamber and mild aqueous cell and flare. Elevated intraocular pressure often causes glaucomatous optic nerve damage, as well as iris atrophy and damage to the anterior epithelial cells of the lens (glaukomflecken). Immediate treatment is imperative and includes systemic acetazolamide as well as topical medication. Surgery is often necessary. Syn. acute glaucoma; congestive glaucoma.
angle-closure g. (ACG) Glaucoma in which the angle of the anterior chamber is blocked by the root of the iris which is in apposition to the trabecular meshwork and thus the aqueous humour cannot reach the drainage apparatus to leave the eye. (As the blockage persists, anterior synechia may result.) This condition occurs usually in anatomically shallow anterior chambers, as is often the case in hypermetropes. Angle-closure glaucoma can either be primary (PACG) or secondary following iritis, iridocyclitis, postoperative complications, traumatic cataract, tumours, etc. Moreover, angle-closure glaucoma is divided into acute and chronic. In chronic angle-closure glaucoma (CACG) there may never be an attack but intermittent periods of increased intraocular pressure caused by progressively extensive peripheral anterior synechia. Symptoms may be absent or there may be periodic episodes of mild congestion and blurred vision. Gonioscopy is essential to differentiate this condition from open-angle glaucoma. People most at risk are females, Chinese and South-East Asian and the average age at presentation is about 60 years. Anatomical predisposing factors are pupillary block and plateau iris. Treatment of angle-closure glaucoma is essentially surgical. However, initially therapeutic agents are used including miotics, hyperosmotic agents, which cause a rapid reduction of the IOP, beta-blockers and carbonic anhydrase inhibitors. Syn. closed-angle glaucoma; narrow-angle glaucoma. A subacute form of angle-closure glaucoma may occur as a result of episodes of elevated intraocular pressure caused by anterior synechia, intermittent pupillary block, or when in a dark room. Attacks tend to resolve spontaneously but treatment with prophylactic peripheral laser iridotomy is frequently undertaken.
See anisocoria; cornea plana; iridoschisis; iris bombé; iris, plateau; method, van Herick, Shaffer and Schwartz; method, Smith’s; test, provocative; test, shadow.
capsular g. See glaucoma, pseudoexfoliation.
chronic g. See glaucoma, angle-closure; glaucoma, open-angle.
ciliary block g. A secondary glaucoma, which occurs when aqueous fluid becomes misdirected into the vitreous cavity. The accumulating fluid then produces a displacement of the lens and iris, causing a narrowing of the anterior chamber angle with resultant raised intraocular pressure. This condition occurs most commonly following intraocular surgery, especially glaucoma surgery after the cessation of cycloplegic medications. Treatment consists of medical intervention (cycloplegics, β-adrenergic agents, carbonic anhydrase inhibitors and hyperosmotic agents) or puncture of the vitreous face with the Nd-YAG laser if medical treatment is unsuccessful. In phakic eyes, vitrectomy is sometimes required to open the anterior vitreous face. Syn. malignant glaucoma.
closed-angle g. See glaucoma, angle-closure.
compensated g. See glaucoma, open-angle.
congenital g. Glaucoma occurring with developmental anomalies that are manifest at birth and interfere with the drainage of the aqueous humour causing an increase in intraocular pressure. This in turn causes stretching of the elastic coats of the eye, enlargement of the globe as the sclera and cornea stretch, optic atrophy, marked cupping of the optic disc and loss of vision. Most noticeable is the enlargement of the cornea. Congenital glaucoma is inherited as an autosomal recessive condition with incomplete penetrance. Immediate treatment is essential. Syn. buphthalmos; hydrophthalmos; infantile glaucoma.
Glaucoma occurying after the age of about three years is more often referred to as juvenile glaucoma as it follows a course similar to adult glaucoma without enlargement of the globe.
See goniotomy; luxation of the lens; Peter’s anomaly; syndrome, Rieger’s; syndrome, Sturge–Weber.
congestive g. See glaucoma, angle-closure.
g. detection Tests that are used to diagnose glaucoma. They are: ophthalmoscopic viewing of the optic nerve head; tonometry; visual field assessment of typical glaucomatous defects; gonioscopy to assess the width of the anterior chamber; pachometry to measure central corneal thickness and anterior chamber depth as well as providing a correction factor for applanation tonometer results; and dimensional analysis of retinal structures including the thickness and topography of the retinal nerve fibre layer (RNFL) and of the optic nerve head, assessed by scanning laser polarimetry, confocal scanning laser ophthalmoscopy, optical coherence tomography, stereoscopic photography of the optic nerve head and red-free photography of the RNFL. Glaucomatous eyes lose retinal nerve fibres with consequent reduction in layer thickness and alteration of the topography of the optic nerve head. These changes frequently precede glaucomatous visual fields losses.
infantile g.; juvenile g. See glaucoma, congenital.
inflammatory g. A secondary glaucoma caused by an intraocular inflammation and characterized by elevated intraocular pressure, which may be transient. The most common cause is either active anterior uveitis or following previous episodes of inflammation. Glaucoma may occur as a result of trabecular meshwork blockage due to deposits of inflammatory debris, or because of complete posterior synechia (called seclusion pupillae) blocking the flow of aqueous causing iris bombe and angle-closure, or peripheral anterior synechia. The inflammatory process is treated along with a reduction of intraocular pressure.
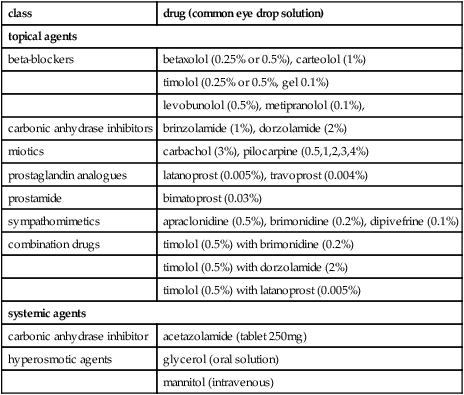
Table G1
Glaucoma medications
| class | drug (common eye drop solution) |
| topical agents | |
| beta-blockers | betaxolol (0.25% or 0.5%), carteolol (1%) |
| timolol (0.25% or 0.5%, gel 0.1%) | |
| levobunolol (0.5%), metipranolol (0.1%), | |
| carbonic anhydrase inhibitors | brinzolamide (1%), dorzolamide (2%) |
| miotics | carbachol (3%), pilocarpine (0.5,1,2,3,4%) |
| prostaglandin analogues | latanoprost (0.005%), travoprost (0.004%) |
| prostamide | bimatoprost (0.03%) |
| sympathomimetics | apraclonidine (0.5%), brimonidine (0.2%), dipivefrine (0.1%) |
| combination drugs | timolol (0.5%) with brimonidine (0.2%) |
| timolol (0.5%) with dorzolamide (2%) | |
| timolol (0.5%) with latanoprost (0.005%) | |
| systemic agents | |
| carbonic anhydrase inhibitor | acetazolamide (tablet 250mg) |
| hyperosmotic agents | glycerol (oral solution) |
| mannitol (intravenous) | |
See iridocyclitis, Fuchs’ heterochromic; syndrome, Posner–Schlossman.
low tension g. See glaucoma, normal-tension.
narrow-angle g. See glaucoma, angle-closure.
malignant g. Elevated intraocular pressure occurring after filtration surgery for glaucoma in which the aqueous humour is diverted posteriorly pushing the vitreous body anteriorly and consequently shallowing the anterior chamber.
neovascular g. A secondary glaucoma due to new vessel formation on the anterior surface of the iris blocking the exit of the aqueous humour through the angle of filtration. It may occur as a result of central retinal vein occlusion (this type typically develops within three months and is sometimes called ‘ninety-day glaucoma’), or diabetes mellitus. Other causes include carotid artery occlusion, central retinal artery occlusion, retinal and choroidal tumours. The condition may initially be open-angle but eventually becomes angle-closure with severe loss of visual acuity, pain, congestion, high intraocular pressure, corneal oedema, aqueous flare, synechia and severe rubeosis iridis. The presence of new blood vessels on the iris and drainage angle distinguishes this condition from primary angle-closure glaucoma. Treatment includes topical steroids to decrease the inflammation, beta-blockers and carbonic anhydrase inhibitors to lower the intraocular pressure and laser treatment of the iris neovascularization and sometimes cyclodestructive procedures (e.g. cyclodiode laser therapy).
See ectropion uvea; neovascularization, iris.
ninety-day g. See glaucoma, neovascular.
normal-tension g. (NTG) An ocular condition in which there is a glaucomatous cupping (often accompanied by disc haemorrhages) and visual field defects with an intraocular pressure of 21 mmHg or less. It is commonly regarded as a variant of primary open-angle glaucoma and it is typically associated with cardiovascular disease or migraine. Treatment with prostaglandin analogues is usually considered the best choice but if there are progressive visual field losses surgery may be needed. Syn. low-tension glaucoma.
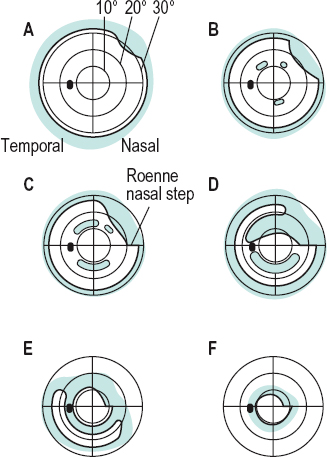
open-angle g. Glaucoma in which the angle of the anterior chamber is open and provides the aqueous humour free access to the drainage apparatus. It can occur: (1) As a primary open-angle glaucoma (POAG) (also called chronic simple glaucoma, compensated glaucoma, chronic glaucoma ). The increased intraocular pressure leads to atrophy and excavation of the optic disc and typical defects of the visual field. It is the most common type of glaucoma (opinions of prevalence vary between 0.5% and 3% of the Caucasian population over 40 years and 2%–3% over the age of 70 years). Because of its insidious nature it is difficult to detect. It tends to occur more often in people after the age of 40, in people who have a family history of the disease, in African-Caribbeans, in people who have high myopia and in people who have diabetes mellitus. It is characterized by an almost complete absence of symptoms. Haloes around lights and blurring of vision occur in some patients when there has been a sudden increase in intraocular pressure or when the disease is very advanced. The diagnosis of this disease is made by demonstrating that the eye has a characteristic visual field loss (Figs. G3 and G4) and exaggerated diurnal fluctuations in intraocular pressure (>5 mmHg). POAG has been found to be caused by mutation in genes at several loci, including myocilin gene (MYOC) on chromosome 1q, optineurin gene (OPTN) on chromosome 10p, WD repeat containing protein 36 gene (WDR36) on chromosome 5q22, and others. (2) The other form is secondary open-angle glaucoma in which the intraocular pressure is elevated as a result of ocular trauma or iridocyclitis, crystalline lens abnormalities, etc. Management of open-angle glaucoma is usually by medication, unless this proves ineffective and surgery may be necessary. Formerly, pilocarpine (or carbachol) or adrenaline (epinephrine) drops were the most commonly used drugs. Nowadays, β-adrenergic blocking agents such as timolol maleate or betaxolol, which act by reducing aqueous humour formation and do not affect pupil size or accommodation, are employed as the initial treatment. Also used are the carbonic anhydrase inhibitors (e.g. acetazolamide) the α-adrenergic agonist (e.g. brimonidine), and the prostaglandin derivatives (e.g. latanoprost), which enhance the uveoscleral outflow.
See atrophy, optic; cup, glaucomatous; hypertension, ocular; iris, plateau; pseudoexfoliation; spot, baring of the blind; test, provocative; test, shadow; vision, tunnel.
phacolytic g. An open-angle glaucoma secondary to a hypermature or mature cataract. It is due to a leakage of lens proteins into the anterior chamber that blocks the outflow of aqueous humour through the trabecular meshwork. It is characterized by an acute onset of pain and redness with high intraocular pressure.
phacomorphic g. A form of secondary angle-closure glaucoma in which the angle of the anterior chamber is closed due to swelling of the lens. Angle closure may be due to pupillary block or in some cases due to anterior pressure on the iris.
pigmentary g. A secondary open-angle glaucoma caused by pigment granules released from the posterior surface of the iris impeding the aqueous outflow through the trabecular meshwork. This type of glaucoma develops in about one-third of patients with the pigment dispersion syndrome, especially myopic males. The pigments are believed to appear as a result of a posterior bowing of the iris rubbing against the zonule. The intraocular pressure is elevated and sometimes high after a sudden release of pigment following mydriasis or strenuous physical exercise with corneal oedema, redness and haloes. Treatment is usually by medication but if this proves ineffective, surgery may be required.
primary g. See glaucoma, angle-closure; glaucoma, open-angle.
pseudoexfoliation g. A secondary glaucoma caused by greyish-white, flake-like basement membrane material and pigment impeding the aqueous outflow through the trabecular meshwork. It usually appears in elderly patients who present with high intraocular pressure, optic disc changes and visual field defects. It is frequently resistant to drug therapy and may require surgery (e.g. laser trabeculoplasty). Syn. capsular glaucoma.
See pseudoexfoliation; syndrome, pseudoexfoliation.
secondary g. Glaucoma occurring as a result of intraocular tumour, iritis, iridocyclitis, uveitis, rubeosis iridis, traumatic cataract, tumours, luxation of the lens, etc.
See epithelial downgrowth; hyphaemia; syndrome, Rieger’s; syndrome, ICE; syndrome, pseudoexfoliation.
simple g. See glaucoma, open-angle.
g. surgery See cyclodialysis; cyclodiode; filtration surgery; goniotomy; iridectomy; iridotomy; sclerectomy; sclerectomy, deep; trabeculectomy; trabeculoplasty; trabeculotomy; viscocanalostomy.
glaucomatocyclitic crisis See syndrome, Posner–Schlossman.
glaukomfleken See glaucoma, acute angle-closure.
glazing Strictly, the fitting of lenses to a frame or mount, but often to include the cutting and edging processes (British Standard).
glial cell of the retina See cell, glial; cell, Mueller’s.
glial veil See papilla, Bergmeister’s.
glioma, retinal See retinoblastoma.
globe of the eye See eyeball.
gloss Shiny appearance of a surface.
See matt surface.
glossmeter Instrument for measuring the ratio of the amount of light specularly reflected from a surface to that diffusely reflected.
See reflection, diffuse; reflection, regular.
glutamate See cone pedicle; neurotransmitter; rod spherule.
glycerin (glycerol) See hyperosmotic agent.
glycocalyx See mucin.
glycoprotein One of a group of conjugated proteins formed by a protein and a carbohydrate, the most important being the mucins (as found in the lens capsule, vitreous humour) and mucoids (as found in bones, cartilage, tendons).
glycosaminoglycan A complex macromolecule considered to be the ‘glue’ of the cornea. It is responsible for providing the plasticity and structural support needed for successful corneal function. Along with other molecules, it comprises the solid portion of the cornea (~22%, the remainder being water). The distribution and arrangement of glycosaminoglycans are responsible for corneal transparency and thickness.
goggles Type of spectacles, usually large with shields and perhaps padding, used as eye protectors from flying particles, dust, wind, chemical fumes or other external hazards.
See glass, safety; shield, eye; spectacles, industrial.
gold deposits See chrysiasis.
Goldmann lens See gonioscope.
Goldmann perimeter See perimeter, Goldmann.
Goldmann tonometer See tonometer, applanation.
Goldmann–Weekers adaptometer See adaptometer.
goniolens See lens, gonioscopic.
gonioprism, Allen–Thorpe A prism in which the base has been curved so that it can rest on the cornea in gonioscopic examination.
gonioscope Instrument used to observe the angle of the anterior chamber of the eye, usually consisting of a biomicroscope in conjunction with a prismatic contact lens (e.g. Allen–Thorpe gonioprism) or a contact lens and mirror (e.g. Goldmann lens). It facilitates the diagnosis of angle-closure and open-angle glaucoma, as well as the diagnosis of secondary glaucoma (Fig. G5).
See lens, gonioscopic; lens, Koeppe.
gonioscopy Observation of the angle of the anterior chamber of the eye with a gonioscope. When the angle is wide open all structures are visible (cornea, Schwalbe’s line, trabecular meshwork, scleral spur, ciliary body); when the angle is closed only the cornea is seen. The width of the angle can be described according to either Shaffer classification (grade 4, wide open (35°–45°): grade 3, moderately open (25°–34°); grade 2, moderately narrow (20°); grade 1, very narrow (10°); grade 0, closed (0°), or Spaeth classification, which categorizes the angle estimated in degrees, as well as the location of the iris insertion and iris curvature.
See method, van Herick, Shaffer and Schwartz.
direct g. Observation of the virtual, erect image of the angle of the anterior chamber as formed by a gonioscopic lens (e.g. Koeppe lens). The image can be viewed with a handheld magnification system with the patient in a supine position.
indentation g. Gonioscopy performed when the angle of the anterior chamber is closed in order to determine whether the closure is appositional or synechial. It is usually done with the four-mirror Zeiss lens by pressing the lens against the cornea forcing the aqueous into the peripheral part of the angle and pushing the iris posteriorly: If the angle is closed by apposition between the iris and cornea (appositional closure) the angle will open. If the angle is closed by adhesion between the iris and cornea (synechial closure) it will remain closed.
indirect g. Observation of the real, inverted image of the angle of the anterior chamber as formed by a gonioscopic lens, such as the Goldmann or Zeiss lens. The image is viewed through a biomicroscope. This is the most commonly used gonioscopic method.
goniotomy A surgical procedure aimed at lowering intraocular pressure by making an incision through the trabecular meshwork to ease the outflow of aqueous humour into Schlemm’s canal. This procedure is used principally in congenital glaucoma.
Table G2
Structures of the angle of the anterior chamber as seen by gonioscopy in an individual in whom the angle is open and none of the structures is obscured by the iris
| structure (anterior to posterior) | anatomy/physiology | normal appearance |
| Schwalbe’s line | posterior termination of Descemet’s membrane | not always discernible off-white ridge; pigment may collect on it |
| trabecular meshwork | site of aqueous flow; covers internal part of Schlemm’s canal | variable degree of pigmentation |
| scleral spur | strip of scleral tissue | thin white line |
| ciliary body band | anterior face of ciliary body in the angle recess | pigmented seen more easily if iris is moved backward |
gonococcal infection See conjunctivitis, acute; ophthalmia neonatorum.
Gradenigo’s syndrome See syndrome, Gradenigo’s.
grades of binocular vision See vision, Worth’s classification of binocular.
gradient method; test See AC/A ratio.
gradient-index lens See lens, gradient-index.
grading scale A method used to present an assessment and recording of the severity of a condition. Grading scales are usually organised in five stages of increasing severity, from grade 0 (normal) to grade 4 (severe). There are many grading scales assessing a variety of conditions. Commonly used scales are: van Herick’s technique and Shaffer classification of the width of the angle of the anterior chamber using a slit-lamp or gonioscope, respectively; Efron grading scales for contact lens complications, a set of 16 anterior ocular complications such as, conjunctival redness, corneal neovascularization, corneal oedema, epithelial microcysts, corneal infiltrates, papillary conjunctivitis, etc. Other grading scales are used to evaluate cortical cataract, nuclear cataract, subcapsular cataract, inflammatory cells and flare in the anterior chamber, retinal arteriovenous crossings, cup-disc ratio, etc.
von Graefe’s test See test, diplopia.
graft, corneal Corneal tissue of a donor used to replace a diseased or opaque cornea.
See keratoplasty.
Gram stain A procedure for detecting and identifying bacteria and certain other microbes. Microorganisms, such as those found in corneal or conjunctival samples, are stained with crystal violet, rinsed in water, treated with iodine solution, decolorized with ethyl alcohol or acetone and counterstained with a contrasting dye, usually safranin, a pink dye. The preparation is then rinsed with water, dried and examined. Microorganisms that retain the crystal violet stain are said to be Gram-positive, while those that retain the counterstain are said to be Gram-negative. Common Gram-negative bacteria include Acinetobacter, Chlamydia trachomatis, Enterobacter, Escherichia coli, Haemophilus influenzae, Moraxella lacunata, Neisseria gonorrhoeae, Proteus vulgaris, Pseudomonas aeruginosa. Common gram-positive bacteria include Mycobacterium chelonae, Mycobacterium fortuitum, Staphylococcus aureus, Staphylococcus epidermidis, Streptococcus pneumoniae, Streptococcus pyogenes.
See bacteria.
gramicidin See antibiotic.
Granit–Harper law See law, Granit-Harper.
granular dystrophy See dystrophy, granular.
granuloma Growth appearing like a nodule, consisting essentially of granulation tissue and occurring as a result of localized inflammation. It can appear on the conjunctiva, the iris, the lacrimal gland, or the orbit.
Grassman’s laws See laws, Grassmann’s.
graticule Graduated transparent scale engraved or photographed, placed in the front focal plane of the eyepiece of an optical instrument for direct observation of the apparent image size or position in the field of view. Example: the focusing screen of a focimeter. Syn. reticule.
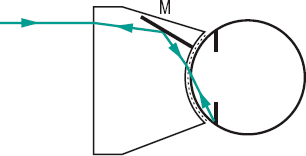
grating A series of black and white parallel bars of equal width used to measure visual acuity, contrast sensitivity, and resolution of optical systems. The grating can be either square-wave (also called Foucault grating or Foucault pattern), in which the luminance across a bar is constant, or sine-wave, in which the luminance varies sinusoidally (Fig. G6).
See cycle per degree; function, contrast sensitivity.
grating, diffraction See diffraction.
Gratiolet, optic radiations of See radiations, optic.
Graves’ disease See disease, Graves’.
Grayson–Wilbrant dystrophy See dystrophy, Reis–Buckler’s.
green The hue sensation evoked by stimulating the retina with rays of wavelength 490–560 nm and situated between blue and yellow. The complementary colour of green is a non-spectral colour situated in the red-purple region.
green blindness See deuteranopia.
gregorian telescope See telescope.
grey A colour said to be achromatic or without hue. It varies in magnitude from white to black. Note: also spelt gray.
grid, Amsler See chart, Amsler.
grid, Hering–Hermann See Hering–Hermann grid.
grid, Javal’s A test for simultaneous binocular vision and for detecting ocular suppression. It consists of five equally spaced opaque, parallel bars crossed by two perpendicular bars. It is held between the reader’s eyes and a page of print. The bars being perpendicular to the lines of the text occlude some letters (along vertical strips) to one eye, but these letters are seen by the other eye. If binocular vision is present no difficulty is experienced in reading the page. This instrument represents the most common type of bar reader.
Groenouw’s nodular type 1 corneal dystrophy See dystrophy, granular.
Grotthus’ law See law, Draper’s.
ground See figure.
Gullstrand’s reduced eye See eye, reduced.
Gullstrand’s schematic eye See eye, schematic.
Gunn’s crossing sign See sign, Gunn’s crossing.
guttata, cornea See cornea guttata.
gyrus One of the prominent rounded elevations between the sulci or grooves on the surface of the hemispheres of the brain. There are numerous gyri. Those associated with the visual association areas are the angular and lingual gyri. Plural: gyri.





