Chapter 51 Fundamentals of cutaneous surgery
Lask GP, Moy RL: Principles and techniques of cutaneous surgery, New York, 1996, McGraw-Hill.
Lawrence C: An introduction to dermatological surgery, London, 1996, Blackwell Science.
Wheeland RG: Cutaneous surgery, Philadelphia, 1994, WB Saunders.
Table 51-1. Recommended Maximum Total Dosages for 1% Lidocaine (10 mg/mL) with and without Epinephrine in Adults and Children
| ADULTS | CHILDREN |
|---|---|
| 4.5 mg/kg (300 mg or 30 mL), without epinephrine | 1.5–2.5 mg/kg, without epinephrine |
| 7.0 mg/kg (500 mg or 50 mL), with epinephrine | 3.0–4.0 mg/kg, with epinephrine |
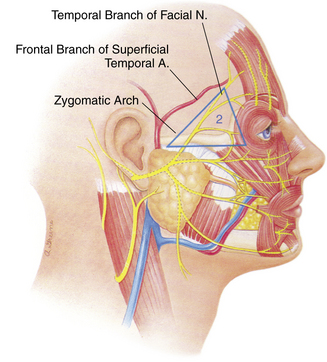
Chlorhexidine gluconate has a much faster onset of action and maintains its antimicrobial activity for up to 6 hours. It should not be used for preoperative skin preparation on the head and neck, due to possible ototoxicity and corneal erosions and opacifications with inadvertent exposure at these sites. Povidone-iodine is a better choice for the head and neck. However, chlorhexidine gluconate is preferable to povidone-iodine for the trunk and extremities, due to its more rapid onset of action, broader spectrum of antimicrobial coverage, and longer duration of activity.
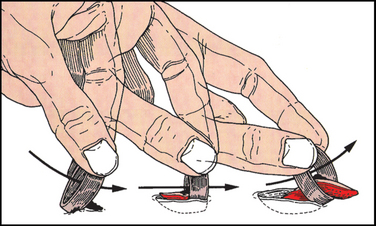
Figure 51-1. Schematic demonstrating the technique for a shave biopsy of skin.
(From Fewkes JL, Cheney ML, Pollack SV: Illustrated atlas of cutaneous surgery, New York, 1992, Gower Medical Publishing, with permission.)
Key Points: Fundamentals of Cutaneous Surgery