CHAPTER 112 Functional Restoration Program Characteristics in Chronic Pain Tertiary Rehabilitation
INTRODUCTION
After most surgical and nonoperative primary and secondary treatment approaches have been exhausted, the majority of patients with occupational musculoskeletal disorders have returned to work and decreased their health utilization. Depending on the US state or federal workers’ compensation venue and musculoskeletal area, an average of about 10% of patients persist with workers’ compensation disability 3–4 months postinjury. The range is about 5–25%, with a smaller (but growing) group of patients persisting in ‘perpetual limited duty’ (or partial disability) in conjunction with the recent advocacy for ‘keeping patients on the job.’ In time, unless such patients are unable to return to full duty or significantly modified jobs, they too go on to persistent work adjustment problems with employers and increasing disability behaviors.
Certain musculoskeletal disorders have a predilection for becoming chronic disabling problems. Spinal disorders, particularly those affecting the low back, usually beginning as ‘sprains and strains,’ are more highly represented among chronic pain/disability work-related injuries than other musculoskeletal areas. Upper extremity non-neurocompressive complaints, particularly those termed repetitive motion or cumulative trauma disorders (CTD) also have a higher rate of developing chronicity, and CTD claims are known to be 1.8 times more expensive than non-CTD claims.1–7 By contrast, lower extremity injuries, particularly if they involve fractures, tend to resolve more completely within a usual tissue healing period. In many ways, the more subjective the diagnosis and mechanism of injury, the greater the likelihood of symptom persistence.
Chronic spinal disorder (CSD) pain is not merely a function of incomplete healing after injury. Traditional medical efforts to treat and rehabilitate chronic back pain have often been met with poor outcomes. Past failed efforts to identify the source of, or treat, CSDs have resulted in the identification of ‘psychogenic’ or ‘functional’ pain, terms attributed to pain for which no physical substrate could be found and, therefore, for which psychological or ‘nonorganic’ causes were suspected. Back pain has been found to be subject to diverse influences including psychological difficulties (e.g. anxiety, substance use, depression), and social losses (e.g. inability to work, family role changes, financial stresses). Turk and Rudy8 set forth the biopsychosocial model of pain asserting that pain is engendered not only by physical insult, but also by cognitive, affective, psychosocial, and behavioral influences. Based on this biopsychosocial theory, CSD treatment considerations now go beyond the physical source of the pain to consider psychological and socioeconomic variables as well.
Economic globalization may create dislocations of local economies. In industrialized countries such as the US, these dislocations cause major shifts in demand for workers in different labor-intensive industries. There are pressures on workers to develop skills to shift jobs within the changing job markets. Industry is incentivized to reject those workers unable to make the transition. There are similar incentives to minimize the appearance of unemployment and job dislocations by ‘disappearing’ less flexible employees from the national economy. When chronic disabling musculoskeletal disorders lead to long-term re-employment problems, employers may find it more convenient to convert them to ‘throwaway workers.’ This creates pressure to compensate such patients with public, rather than private financing. Since the 1960s, Social Security Disability Insurance (SSDI), more recently linked to medical benefits through Medicare, has been provided to such individuals under certain circumstances. There has been a recent exponential growth in acceptance of younger and potentially more able-bodied workers onto this national insurance scheme, which was initially intended for retirees. Although musculoskeletal problems have decreased as the reason for acceptance onto SSDI rolls, they remain above 35% of all accepted claims. The combination of musculoskeletal and mental health ‘stress claims,’ which are often intertwined, have become the majority of acceptances onto SSDI. Because of the young age (30–45 years) at which many of these workers are accepted for long-term payments, Social Security actuaries have referred to the problem as one of ‘early, early retirement.’ Current costs are US$100 billion/year for SSDI, up 150% since 1980. There are now nearly 9 million ‘disabled’ pre-retirement Americans on Social Security, more than double the number in 1980.9 There is huge variance from state to state, with twice as many claims accepted in the disability determination process, and three times as many after the administrative hearing process, in the high-acceptance states (New Hampshire, Maine) compared to low-acceptance states (District of Columbia, Texas). The younger the patient accepted, the more likely there is a musculoskeletal basis, and low back pain is the single largest cause of musculoskeletal disability. With disability payments currently representing 5% of the entire US budget, such payments are becoming an increasing drain on the Social Security funds that were initially intended solely for retirees. Failure of tertiary rehabilitation for chronic occupational spinal disorders leads inevitably to patients departing the employment statistics and transitioning to insurance schemes such as SSDI in ever-increasing numbers. Thus, tertiary rehabilitation becomes the leading prevention strategy against permanent loss of productivity and high social cost in US spinal disorder medical care.
Because of the multifactorial and subjective nature of chronic pain, traditional therapy has been less than fully effective in treating and rehabilitating CSD patients. As a result, medical approaches have evolved to accommodate this costly and complex phenomenon. There are several risk factors that can be used to guide the treatment of spinal disorders and pain based on the levels of treatment described below. The severity of the dysfunction must be considered. The severity of a musculoskeletal dysfunction is related more to the patient’s chronicity and level of disability than to the presumed causative event. While diagnoses (e.g. degenerative disc disease, facet arthropathy, disc disruption, segmental instability) may be important in identifying surgically treatable pathology, their relevance fades in chronic pain conditions in which patients have generally failed to respond to invasive procedures, or have been deemed unsuitable for surgery. In addition to the psychological factors, inactivity and disuse may play a major role. They may lead to the deconditioning syndrome, in which the injured spinal region becomes a ‘weak link’ connecting the body’s functional units. Deficits of motion, strength, and endurance interfere with physical performance of otherwise unaffected joints and muscles.10–14 While the need for spine surgery is rarely so imminent that a trial of nonoperative therapy is not indicated, there is often a limited understanding of the levels and purposes of such care as a function of the severity of the problem.
Three levels of nonsurgical care
Secondary treatment applies to those individuals (approximately 20–30%) whose pain persists beyond 2–6 months after the initial pain onset (i.e. beyond a reasonable tissue healing period), and who have not responded to primary treatment. More precisely, patients in the postacute phase of injury (and some postoperative patients) are likely to qualify for secondary nonoperative treatment. The secondary level of treatment is geared mainly toward patient reactivation, providing treatment of medium intensity. This intensity level is based on prevention strategies for managing risk factors for developing disability, deconditioning, and chronicity. The secondary level of treatment includes reactivation therapies that involve exercise and education specifically designed to prevent physical deconditioning. The exercise therapy may be supplemented by spinal injections for nerve irritation not requiring surgical decompression (epidural steroids), trigger point injections, or sacroiliac joint injections.15–17 Facet injections may be provided either for pain of facet origin, known as the facet syndrome, or for segmental rigidity noted on physical examination.18–23 Pharmacologic agents may be useful, but trends are away from habituating medication, such as narcotics and benzodiazepine ‘muscle relaxants,’ towards antiinflammatory medications. Exercise and education is usually provided by physical and/or occupational therapists in treatments lasting 1–3 hours several times weekly. Such treatments may also be supplemented by consultative psychological, case management, and physician services in formal programs; such programs are currently termed work conditioning or work hardening, and may involve daily utilization of 4–8 hours/day.
The 5–8% of patients whose CSD pain persists beyond 4–6 months after the initial occurrence, and for whom disability predominates, are considered for referral to the tertiary level of treatment. Tertiary treatment at its best is a physician-directed, intensive, interdisciplinary team approach aimed at overcoming chronic pain and disability. The main goal of tertiary treatment is to ameliorate the permanent impairments and prevent the costly permanent disabilities related to CSDs that are the number one causes of total disability payments to claimants under age 45 for federal (public) or long-term (private) disability insurance schemes. Functional restoration programs are typically organized in a fashion similar to the traditional pain rehabilitation clinic, but these are more diverse and eclectic. The Commission for Accreditation of Rehabilitation Facilities (CARF) has guidelines that can be used as a minimum standard for tertiary care programs, currently termed Interdisciplinary Pain Rehabilitation programs. Because of the wide international reach of CARF, such programs may represent functional restoration for occupational injuries (as discussed in this case), or run the gamut to programs that are most involved in cancer care or are mainly an adjunct to pain physician injection therapies and other palliative procedures. Because tertiary care patients have been shown to have a history of psychosocial, as well as functional, disturbances (e.g. substance abuse, affective disorders, limited compliance), tertiary treatment programs address issues of both physical and psychosocial deterioration. Functional restoration is one mode of tertiary treatment that has arisen in response to the poor outcomes associated with the traditional pain clinic, particularly in occupation CSDs.
The site of the disorders: cervical and lumbar
The greatest assessment error for most clinicians is the failure to recognize the critical importance of socioeconomic factors in patients with chronic pain. It has been well established over the years that patients being paid for remaining disabled and nonproductive will behave differently from patients who are uncompensated.24–27 Similarly, patients likely to receive a bonus settlement for permanent impairment, even if they are not receiving direct disability indemnity benefits, will likely demonstrate some illness behaviors. Major Axis I psychiatric diagnoses (DSM-IV), such as substance use (often preexisting or iatrogenically abetted), or major depression, may strongly affect treatment progress and ultimate outcomes.28–30 This is particularly true if the clinician fails to recognize, or ignores, these crucial issues, dealing ‘only with the body and not the mind.’ Various treatment interventions have been designed to cope with the psychosocial and socioeconomic factors involved in total or partial disability. Psychosocial assessment is often necessary to identify these factors and guide treatment. In addition to psychosocial problems originating because of persistent pain and disability, latent psychopathology may also be activated by life disruption produced by pain/disability. As such, psychiatric interventions, including use of psychotropic drugs and detoxification from narcotic and tranquilizer habituation, are helpful. Primary and secondary treatment alone may be ineffective in dealing with these multifactorial chronic dysfunctions, so that programmatic care delivered by an interdisciplinary team is desirable, if available.
QUANTIFICATION OF PHYSICAL DECONDITIONING
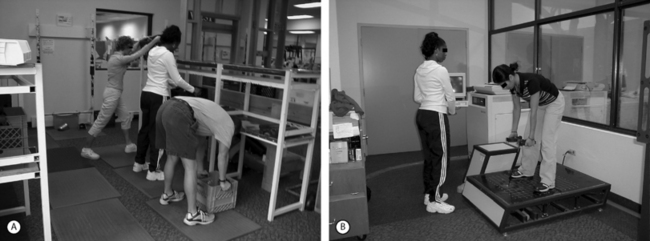
While a normal soft tissue, joint, or bony healing period will generally have occurred by the time a patient enters a period of chronic pain/disability, progressive deterioration of physical and functional capacity may still be in an early stage. Deconditioning occurs as a consequence of disuse and fear-related inhibition. The quantitative assessment of function is a vital aspect of developing an effective treatment program for disabling spinal disorders. In the extremities, there is relatively good visual feedback of physical capacity. Joints are easily seen and mobility subject to goniometric measurements, and the muscle bulk is subject to tape measurements. Right/left comparisons between a normal and abnormal side can frequently be made. In the spine, there is inadequate direct visual feedback of physical capacity. Yet, this deficiency has not been generally recognized by clinicians who often continue to rely on subjective self-report or physical measures that are either inaccurate or irrelevant. More accurate methods are necessary for objective quantification.31–34 This information is discussed in greater detail in another chapter. However, for the focuses of this chapter, the author wishes to illustrate several aspects of quantification of function. In Figure 112.1, one sees the dual inclinometer method being used to measure spinal sagittal motion. In Figure 112.2, sagittal spine strength is being tested. The measurements of localized mobility and strength in the injured spinal region is termed physical capacity as it documents the ‘weak link’ deconditioning of an injured or involved area. This is contrasted with the concept of functional capacity, representing whole-person measurements. For whole-person functional measurements, lifting is a useful tool to assess lumbar (floor-to-waist) and cervical (waistto-shoulder) functional regions. The progressive isoinertial lifting evaluation (PILE) test is a simple and inexpensive way to accomplish such measurement as seen in Figure 112.3A.35–37 Figure 112.3B demonstrates isokinetic and isometric (National Institute of Occupational Safety and Health) lift testing being performed.
PSYCHOSOCIAL AND SOCIOECONOMIC ASSESSMENT
Early efforts to distinguish between ‘functional’ (nonorganic) and ‘organic’ pain did not meet with success. The complex nature of chronic pain makes it difficult to categorize component factors as purely physical or psychological. Chronic pain must be understood as an interactive, psychophysiological behavior pattern wherein the physical and the psychological overlap. The focus of psychological evaluation of the patient with pain must shift away from ‘functional’ versus ‘organic’ distinctions to the identification of psychological behavioral motivators for each patient. These characteristics impact a patient’s disability and his or her response to treatment efforts. Treatment planning and the prediction of favorable treatment outcome are facilitated by first identifying and then controlling these factors.
TERTIARY INTERDISCIPLINARY FUNCTIONAL RESTORATION TREATMENT
Sports medicine concepts and physical training
The principles of sports medicine have come to be used generally to refer not merely to the rehabilitation of the competitive athlete. Instead, they have been modified to emerge as a conceptual and methodological framework for actively treating all individuals who wish to return to high levels of function. Its component parts are shown in Table 112.1. Much of the initial work was done with extremity injury, but these concepts now involve the spine as well.
Dynamic muscle training, which has been shown to be the most efficient method of training, can be employed in CSDs. It involves three basic modes: isotonic, isokinetic, and psychophysical (free weights).38 Isotonic exercises are those in which the same force is applied throughout the dynamic range and is often inappropriately used for exercises in which a changing lever arm actually alters the applied torque. This type of exercise is most often associated with the variable resistance devices, utilizing a cam to equalize muscular demands throughout the dynamic range of motion.
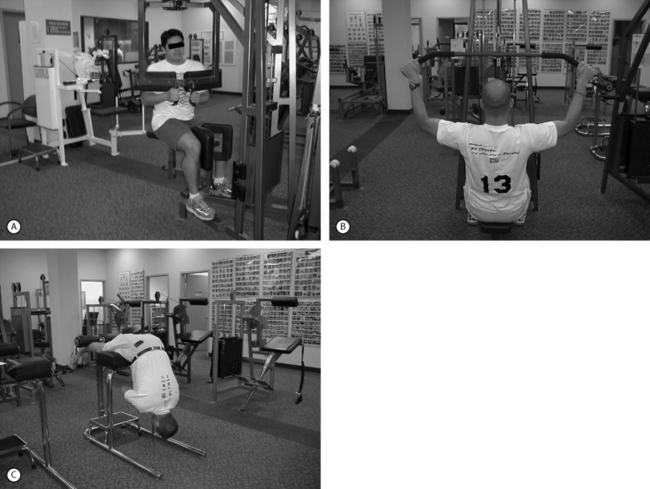
Strength training is generally done with weight machines. In the functional restoration program at PRIDE (Productive Rehabilitation Institute of Dallas for Ergonomics) the quantification of function using tests described in the previous chapter develops data that are fed into a computer system, which calculates suggested levels of training based on age, gender, body weight, and anticipated activity levels. A stepwise program to increase from the test-determined starting levels, checked periodically with repeat testing, is utilized. In Figure 112.4A, a torso rotation device to strengthen oblique spinal and abdominal musculature is utilized. Figure 112.4B shows a pull-down device for shoulder strength that also affects musculature in the cervical area (paraspinal muscles, trapezii, and scalene muscles). When a fitness maintenance program is developed for patients to continue with what they have learned during their rehabilitation, a Roman chair (Figure 112.4C) may be useful for extensor strengthening of all of the spine muscles from cervical to lumbar area, including the gluteal/hip muscles.
In the physical therapy areas, patients train the injured ‘weak link’ area of the spine. This area must be isolated and focused on by the therapists in a supervised environment, because patients are generally inhibited by fear-avoidance or prolonged disuse. Most training devices are therefore specific to a certain injured part of the body (e.g. cervical spine, lumbar spine, knees, etc.). In the occupational therapy area, patients focus on coordinating the injured ‘weak link’ with other body parts to achieve full-person functional activities. The performance of such functional activities predominates, encouraging such capabilities as lifting, bending, reaching, climbing, or twisting. An obstacle course of multiple devices used to demand patient agility in performing functional tasks can be very useful. Figure 112.5A demonstrates a patient who combines functional tasks, including lifting, carrying, and climbing, with a relatively simple stair device. Figure 112.5B shows wall-mounted devices that can be used to enhance upper extremity motion for patients with cervical CSDs with radicular problems, or associated upper extremity disorders. In the later stages of functional restoration, the occupational therapists supervise a ‘ready room’ allowing actual simulation of work tasks, such as truck driving, clerical work, construction work (carpentry, electrical, plumbing, etc.) and other manual tasks.
Psychosocial interventions in functional restoration
Behavioral stress management training
The patient’s ultimate socioeconomic outcomes depend on the maintenance of treatment goals. Under treatment supervision, patients generally achieve a much higher level of physical and functional capacities, which must be continued in a fitness maintenance program (FMP). The patient is educated on an individualized FMP, based on the training level they have achieved by the program’s conclusion. Follow-up objective physical quantification leads to feedback to the patient on maintenance of physical capacity, which can be correlated with job demands. Relevant pieces of durable medical equipment (DME) (see Fig. 112.4C) or memberships in appropriately equipped fitness centers, may be suggested.
1 Mayer T, Gatchel R, Polatin P, et al. Outcomes comparison of treatment for chronic disabling work-related upper extremity disorders and spinal disorders. J Occup Environ Med. 1999;41:761-770.
2 Vender M, Kasdan M, Truppa K. Upper extremity disorders: A literature review to determine work-relatedness. J Hand Surg. 1995;20A(4):534-541.
3 Association of Schools of Public Health/National Institutes for Occupational Safety and Health. Proposed national strategies for the prevention of leading work-related diseases and injures. Part 1. Washington, DC: Association of Schools of Public Health, 1986;19.
4 Bureau of Labor Statistics. Workplace injuries and illnesses in 1994 (USDL Publication No. 95–508). US Department of Labor, Washington DC, 1995. Available: osh/osnr0001.txt.
5 Bureau of Labor Statistics. Workplace injuries and illnesses in 1996 (USDL Publication No. 97–453). US Department of Labor, Washington, DC, 1997. Available: osh/osnr0005.txt.
6 Brogmus G, Sorock G, Webster B. Recent trends in work-related cumulative trauma disorders of the upper extremities in the United States: An evaluation of possible reasons. J Occup Environ Med. 1996;38(4):401-411.
7 Webster B, Snook S. The cost of compensable upper extremity cumulative trauma disorders. J Occup Med. 1994;36(7):713-727.
8 Turk D, Rudy T. Toward a comprehensive assessment of chronic pain patients. Behavioral Res Ther. 1987;25:237-249.
9 Charting the future of Social Security Disability Programs. The need for fundamental change, Social Security Advisory Board Report. Washington, DC: Congressional Printing Office, January 2001.
10 Beals R. Compensation and recovery from injury. West J Med. 1994;140:233-237.
11 Keeley J, Mayer T, Cox R, et al. Quantification of lumbar function, part 5: reliability of range of motion measures in the sagittal plane and an in vivo torso rotation measurement technique. Spine. 1986;11:31-35.
12 Kishino N, Mayer T, Gatchel R, et al. Quantification of lumbar function, part 4: isometric and isokinetic lifting simulation in normal subjects and low back dysfunction patients. Spine. 1985;10:921-927.
13 Mayer T, Smith S, Keeley J, et al. Quantification of lumbar function, part 2: sagittal plane trunk strength in chronic low back pain patients. Spine. 1985;10:765-772.
14 Mayer T, Tencer A, Kristoferson S, et al. Use of noninvasive techniques for quantification of spinal range-of-motion in normal subjects and chronic low-back dysfunction patients. Spine. 1984;9:588-595.
15 Benzon H. Epidural steroid injections for low back pain and lumbosacral radiculopathy. Pain. 1986;24:277-295.
16 Dilkem T, Burry H, Grahame R. Extradural corticosteroid injection in management of lumbar nerve root compression. Br Med J. 1973;16:635-637.
17 Weinstein SM, Herring SA, Derby R. Epidural steroid injections. Spine. 1995;20:1842-1846.
18 Dreyfuss P, Dreyer S, Herring S. Lumbar zygapophyseal (facet) joint injections. Spine. 1995;20:2040-2047.
19 Jackson R, Jacobs R, Montesano P. Facet injection in low back pain: a prospective statistical study. Spine. 1998;13:966-971.
20 Mayer T, Robinson R, Pegues P, et al. Lumbar segmental rigidity: can its identification with facet injections and stretching exercises be useful? Arch Phys Med Rehabil. 2000;81:1143-1150.
21 Mayer T, Gatchel R, Keeley J, et al. A randomized clinical trial of treatment for lumbar segmental rigidity. Spine; In press.
22 Mooney V, Robertson J. The facet syndrome. Clin Orthop. 1976;115:149-156.
23 Schwarzer A, Aprill C, Derby R, et al. Clinical features of patients with pain stemming from the lumbar zygapophyseal joints. Is the lumbar facet syndrome a clinical entity? Spine. 1994;19:1132-1137.
24 Rainville J, Hartigan C, Wright A. The effect of compensation involvement on the reporting of pain and disability by patients referred for rehabilitation of chronic low back pain. Spine. 1997;22:2016-2024.
25 Greenough C, Fraser R. The effects of compensation on recovery from low back injury. Spine. 1989;14:947-955.
26 Hadler N, Carey T, Garrett J. The influence of indemnification by workers’ compensation insurance on recovery from acute backache. Spine. 1995;20:2710-2715.
27 Sanderson P, Todd B, Holt G, et al. Compensation, work status, and disability in low back pain patients. Spine. 1995;20:554-556.
28 Polatin P, Kinney R, Gatchel R, et al. Psychiatric illness and chronic low back pain: The mind and the spine – Which goes first? Spine. 1993;18:66-71.
29 Dersh J, Gatchel R, Polatin P. Chronic spinal disorders and psychopathology: research findings and theoretical considerations. Spine J. 2001;1:88-94.
30 Dersh J, Gatchel R, Polatin P, et al. Prevalence of psychiatric disorders in patients with chronic work-related musculoskeletal pain disability. J Occup Environ Med. 2002;44:459-468.
31 Gatchel R, Mayer T, Hazard R, et al. Functional restoration: Pitfalls in evaluating efficacy [editorial]. Spine. 1992;17:988-995.
32 Hazard R. Spine update: Functional restoration. Spine. 1995;20:2345-2348.
33 Hazard R, Fenwick J, Kalish S, et al. Functional restoration with behavioral support: A one-year prospective study of chronic low back pain patients. Spine. 1989;14:157-165.
34 Mayer T, Gatchel R, Mayer H, et al. A prospective two-year study of functional restoration in industrial low back injury: An objective assessment procedure. JAMA. 1987;258:1763-1767.
35 Mayer T, Barnes D, Nichols G, et al. Progressive isoinertial lifting evaluation, Part I: A standardized protocol and normative database. Spine. 1988;13:993-997.
36 Mayer T, Barnes D, Nichols G, et al. Progressive isoinertial lifting evaluation, Part II: A comparison with isokinetic in a disabled chronic low back pain industrial population. Spine. 1988;13:998-1002.
37 Mayer T, Gatchel R, Barnes, et al. Progressive isoinertial lifting evaluation: an erratum notice. Spine. 1990;15:5.
38 Eriksson E. Sports injuries of knee ligaments. their diagnosis, treatment, rehabilitation and prevention. Med Sci Sports. 1976;8:133-144.