Full-Thickness Macular Hole
Clinical Features:
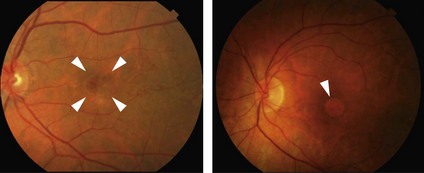
Classic symptoms are acute unilateral decreased vision and occasional metamorphopsia. An impending macular hole may be seen as a loss of the normal fovelar depression with a yellow spot or ring in the center of the macula. A full-thickness macular hole (FTMH) is seen as a well demarcated, round red spot in the center of the macula surrounded by a grey halo that represents a cuff of subretinal fluid around the hole (Fig. 10.2.1) An operculum may be seen above the hole. Yellowish deposits may be seen within the hole.
OCT Features:
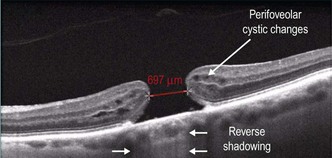
OCT features of macular holes include a full-thickness defect in the neurosensory retina (Figs 10.2.2 to 10.2.4). There may be cysts in the neurosensory retina surrounding the area of the hole. A cuff of subretinal fluid may be seen around the defect in the retina. The vitreous may be attached to the hole with vitreomacular traction or there may be an operculum seen in the posterior vitreous on OCT scanning. Chronic macular holes may show loss of the cuff of subretinal fluid. There may also be RPE atrophy seen in chronic holes.
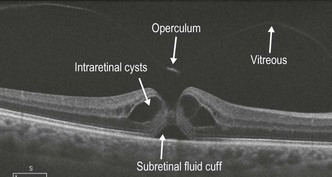
Figure 10.2.2 OCT scan through an acute macular hole showing intraretinal cysts, a cuff of subretinal fluid and an operculum . Note that the vitreous is detached from the fovea.
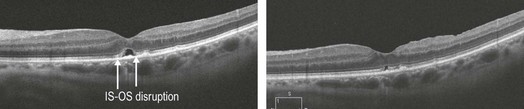
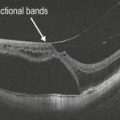
Figure 10.2.4 One week and one month post-vitrectomy for macular hole closure. Note the small area of subretinal elevation that decreases with time with restoration of the ELM and a small area of disruption in the IS–OS/ellipsoid layer. Various studies have shown that disruption in the ELM, IS–OS/ellipsoid layer, as well as the length of disruption of the cone outer segment tips correlates with level of post-operative visual acuity.
▶ Stage 0 macular hole: On OCT, this is an eye with VMA which has a FTMH in the contralateral eye. The risk of progression to a full-thickness hole in the eye with VMA may be close to 40%.
▶ Stage 1 macular hole: This is an eye with vitreomacular traction.
▶ Stage 2, 3 and 4 macular holes per Gass’s classification are now re-classified as small, medium or large macular holes with (stage 4) or without (stage 2 and 3) release of the vitreomacular adhesion.
▶ Small FTMH – aperture size less than or equal to 250 µm
▶ Medium-sized FTMH – aperture size between 250 µm and 400 µm
FTMH may further be sub-classified by presence or absence of ongoing VMT.
Management:
For stage 0 and 1 macular holes, the management is as described in the VMA/VMT section (Chapter 10.1). FTMHs are typically treated surgically, with excellent prognosis for closure and visual recovery for small and intermediate sized holes. Chronic (>2 years) holes show slightly lower closure rate with surgery, but the visual results are significantly less than acute FTMH. Small and medium-sized FTMH can be treated with intravitreal ocriplasmin with closure rates of approximately 50%.