CHAPTER 17 Fractures of the Neck of the Radius in Children
INTRODUCTION
Fractures of the neck and head of the radius in children are relatively uncommon, constituting 4% to 7% of elbow fractures and dislocations.2,6,14,16,21,24 A review of the early literature reveals considerable controversy on the significance, treatment, and late results of this injury.12,23,24 However, as is explained in the body of this chapter, since the last edition of this text there has been a growing body of evidence indicating that open reduction and internal fixation should be avoided whenever possible, and that percutaneous reduction (and fixation if necessary) is much more likely to result in a favorable outcome.
Sex frequency varies from series to series, but overall, there seems to be a slight female preponderance. The typical patient age range for radial neck fractures is between 4 and 14 years, with a mean age between 10 and 12 years. Approximately 30% to 50% of patients have associated injuries to the elbow region (Figs. 17-1 and 17-2).10,18,32,39
The prognosis after this fracture seems to depend more on the severity of the injury, the associated injuries about the elbow, and the type of treatment than on the accuracy of the reduction.10,16,23,25 Although emphasis has been placed on the angulation of the radial head, it is actually the displacement of the fracture that is the more important component of the deformity.
The classic discussion on this subject was published by Jeffery,10 whose observations in 1950 clarified the nature of the fracture, the mechanism of injury, the radiologic assessment, the method of reduction, and the prognosis. Complete remodeling of a fracture was demonstrated with perfect function after a residual angulation of 50 degrees.
Closed reduction consistently produces better results than open reduction, even taking into account that more severe injuries are more likely to require operation.23,25 Recently, significant technical advances have been made, making possible the percutaneous reduction of even severely displaced or angulated fractures.1,8,20,31,34
MECHANISM OF THE FRACTURE
A fall on the outstretched arm produces a valgus thrust on the elbow that fractures the radial neck and often avulses structures on the medial side of the joint. The radial head tilts laterally because the forearm is usually supinated, but the exact direction of the tilt depends on the rotational position of the forearm at impact. This is the most common mechanism, but the fracture can also occur with posterior dislocation of the elbow, resulting in two types of displacement, depending on whether the radial head fractures during spontaneous reduction or in the course of dislocating. The first type of fracture10,11 (reduction injury) leaves the separated proximal radial epiphysis tilted 90 degrees posteriorly beneath the capitellum of the humerus (Figs. 17-3 and 17-4). This mechanism of injury has been confirmed in a report of an iatrogenic radial neck fracture that occurred during closed reduction of a posterior elbow dislocation.36 With the second type of fracture23 (dislocation injury), axial compression on the elbow results in anterior displacement of the radial head as the proximal radial epiphysis moving posteriorly is obstructed by the capitellum and fractures in the process (see Fig. 17-2). Less common injuries include anterior dislocation of the head of the radius with associated fracture of the radial neck; Montaggia equilavent injuries28; shear fracture through the neck of the radius with medial displacement of the shaft, which may become locked medial to the coronoid process of the ulna17; and osteochondral fracture of the epiphysis with an intra-articular loose body.
Associated injuries occasionally occurring with radial neck fracture include fracture of the olecranon, avulsion of the medial epicondyle of the humerus, dislocation of the elbow, and avulsion of the medial collateral ligament from the distal humerus.10 Associated injuries are not only important in themselves but also have implications for prognosis and treatment of the radial neck fracture (see Figs. 17-1 and 17-2).16,39
CLASSIFICATION
The fracture may be classified by the degree of angulation of the radial head,24,26 the mechanism of injury,10 the type of epiphyseal plate disruption,26,29 the amount of fracture displacement, or combinations of these.23 O’Brien24 divided these fractures into three groups according to the degree of angulation:
Type III: More than 60 degrees
It is important to recognize that the neck of the radius normally subtends an angle of 165 to 170 degrees with the shaft (see Chapter 2). The radius is not a straight bone, even in its proximal third.16,33 Thus, a measured angulation of 50 degrees may in reality represent only 35 to 40 degrees of true angulation. As in many pediatric injuries, comparison with the uninjured elbow is often helpful, or even essential, for accurate assessment of this feature.
The injury also may be classified according to the type of epiphyseal plate injury. Although some authors believe that the fracture may occur entirely through the metaphysis of the neck of the radius,12,38 this is unusual, both in the literature23 and in our experience.39
Type I: Rare and usually associated with dislocation of the radial head or elbow
Type II: The most common pattern of fracture through the neck of the radius
Type IV: Second in frequency39 and associated with a poor prognosis owing to marked displacement, irregularity of the radial head, and occasional radioulnar synostosis (Figs. 17-5 and 17-6)
We prefer the classification of Wilkins,27 which combines those of Jeffery10 and Newman.23 It is based primarily on the mechanism of injury, but it also describes the deformity to be corrected and suggests the severity of the injury and thus helps in formulating the prognosis.
TREATMENT
ASSESSMENT OF INJURY
The entire extremity should be thoroughly examined for open wounds, other injuries, and neurovascular impairment. A fall on the outstretched hand can result in injury at multiple levels. As in adults, injury about the wrist must be specifically excluded, and fracture of the scaphoid has been reported.10,11
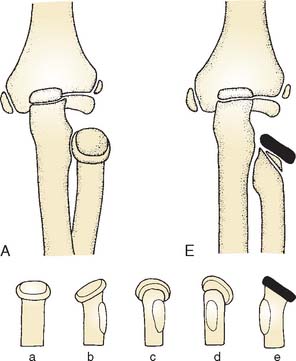
The precise degree of angulation can be accurately determined only by an anteroposterior radiograph with the forearm in the position of rotation at the moment of impact. Jeffery10 demonstrated that this is best achieved by taking radiographs in varying degrees of forearm rotation so that the radial head will cast shadows of different shapes. When the radial head forms as nearly perfect a rectangle as possible, the real degree of angulation can be determined. Oval shapes indicate that the radiographs have not been taken at a right angle to the plane of maximal angulation (Fig. 17-7). Although ob-taining these multiple views is not practical or necessary for the majority of fractures, in cases in which it is unclear whether or not fracture reduction is indicated, performing multiple radiographs as described can be very helpful. Comparison views of the uninjured forearm in the same degree of rotation are helpful in assessing the degree of angulation. Also, in children, normal variations in the radiographic appearance of the proximal radius must be considered when assessing injury.30 Again it is a basic principle of treating elbow fractures in children that radiographs of the injury may be compared with films of the opposite (uninjured) side.
INDICATIONS FOR REDUCTION
It is generally agreed that a radial neck fracture with angulation of more than 60 degrees or more than 3 mm of displacement will likely produce problems if it is not corrected.2,6,23,24,39 It is also agreed that in radial neck fractures, less than 30 degrees’ angulation can safely be accepted,10,25,33 and there is some support for the position that fractures less than 45 degrees’ angulation do not require open reduction.2,23,24,32,35,39 The proper treatment approach should be individualized based on the clinical circumstances of each patient when angulation is between 30 and 60 degrees. There is support both for and against open reduction of these fractures.6,18,25,26,32,39 Advocates of open reduction believe that, without it, significant loss of forearm rotation will ensue. Those who prefer closed reduction or acceptance of deformity believe that the complications of open reduction do not justify the risks, considering the minimal disability that is the legacy of fractures left with even 50 to 55 degrees of angulation.
Recently, two techniques have been developed that provide the benefits of improved fracture alignment yet have not caused the problems associated with open reduction. In several series, percutaneous reduction of radial neck fractures has been associated with fewer complications and less elbow stiffness as compared with open reduction (Fig. 17-8).1,20,31 Originally described using a Steinmann pin, we have also used a small elevator to percutaneously reduce the fracture with excellent success. After percutaneous reduction, fracture stability should be assessed by bringing the elbow through full range of motion including pronation and supination under fluoroscopic imaging. Frequently, the fracture is stable enough that internal fixation is not necessary and casting alone is sufficient. In situations in which redisplacement or angulation occurs, percutaneous pinning or intramedullary stabilization using the Metaizeau technique may be employed.
Metaizeau and colleagues20 described a method of reducing and stabilizing displaced or angulated radial neck fractures using an intramedullary K-wire. An intramedullary pin or small-diameter flexible intramedullary nail is used to enter the radius in a retrograde fashion just proximal to the distal radial physis. Before insertion, a 30- to 45-degree bend is placed in the pin approximately 1 cm from the tip. Advancing the intramedullary pin proximally to the fracture site, the intramedullary pin is used to elevate the depressed or angulated fracture (Fig. 17-9). Rotation of the bent tip is then used to correct displacement. The intramedullary pin is cut proximally where it lies beneath the skin, along the surface of the radius. Often, the pin becomes symptomatic at the insertion site and may be removed after the fracture has completely healed, 3 to 9 months following surgery. Occasionally, radial neck fractures cannot be reduced by use of an intramedullary pin alone. Employment of an intramedullary pin in combination with percutaneous reduction techniques described earlier is a very effective means of reducing and stabilizing severely displaced or angulated fractures by minimally invasive methods. Percutaneous and intramedullary reduction and fixation techniques represent a significant advance in the treatment of radial neck fractures, providing the benefits of improved fracture reduction with minimal risk of avascular necrosis (AVN) and stiffness associated with open techniques.8,20
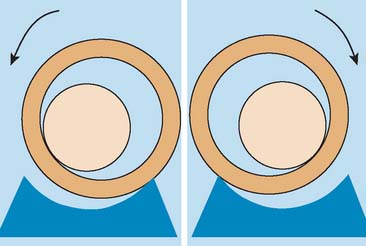
Displacement, rather than angulation, often leads to loss of forearm rotation. Angulation produces a defect at the joint surface and, therefore, does not obstruct rotation. Incomplete contact between articular surfaces is, theoretically, harmful, but enough remodeling usually occurs so that the incomplete contact appears to improve. Displacement, on the other hand, results in radial neck deformity and abutment on the edges of the radial notch (Fig. 17-10). This produces a cam effect during rotation, confirmed in cadaver studies.39 The radial neck was divided with a saw and fixed with Kirschner wires without angulation but with varying degrees of displacement. The observed effect on forearm rotation was that displacement greater than 3 mm resulted in loss of forearm rotation because of abutment of the radial head against the ulna.
Because closed or open reduction performed more than 5 to 7 days after injury leads to loss of forearm rotation and radioulnar synostosis,18,23,32,39 a fracture more than 1 week old is a relative contraindication to reduction. It is better to accept deformity.
PRINCIPLES OF TREATMENT
Review of the literature indicates that, regardless of the severity of the injury, closed treatment gives better results than open treatment. In addition, fractures treated with internal fixation tend to have poor results compared with those treated without internal fixation. In particular, transcapitellar fixation with a Kirschner wire passed through the capitellum of the humerus and across the joint into the head and medullary canal of the radius is associated with significant complications including septic arthritis, breakage of the wire within the joint, and nonunion (see Figs. 17-4 and 17-11).7,19 Thus, as little internal fixation as possible is recommended.2,39 When necessary, intramedullary fixaton using the Metaizeau technique seems to avoid the undesirable consequences associated with other internal fixation techniques. Finally, immobilization of the elbow for more than 3 to 4 weeks leads to stiffness, even in children.
Thus, the following principles apply to treating radial neck fractures:
RESULTS
When assessing the published results of radial neck fractures, it is apparent that pain from this injury is seldom disabling.9,21,32,35,39 Unsatisfactory results consistently are based on the degree of restriction of elbow and forearm motion.6,7,10,23,26 It may be that permanent stiffness develops, not only because of a mechanical block to rotation but also, possibly, because of reflex inhibition to avoid a painful arc of motion. Even when irregularity of the joint surface results in stiffness, there is usually surprisingly little pain. On the other hand, a “successful” open reduction with a perfect anatomic result also may be associated with significant loss of forearm rotation. Series of patients followed as long as 22 years confirms this impression: Pain is not a prominent feature and is not the reason for poor results.39
AVN of the radial head, radioulnar synostosis,1,18,23,39 and removal of the radial head are associated with poor results.1,22,35 The incidences of radioulnar synostosis and AVN of a substantial portion of the head of the radius are difficult to determine because of the small series of fractures of the neck of the radius in children. The problem is further complicated by the fact that these complications are associated with widely displaced fractures, those treated overenthusiastically, those treated late, and those concomitant with dislocations of the elbow. These injuries, in turn, make up a smaller part of the total number of fractures. It is enough to say that, in almost every reported series, these complications are mentioned. AVN and synostosis complicate 5% to 20% of fractures and usually follow open reduction and fixation.
The unanticipated good results subsequent to acceptance of considerable deformity is related to remodeling of the deformity.4,9,10,18 This is surprising, because the plane of the fracture lies at right angles to the plane of motion of both the elbow and the radioulnar joints. This would seem to be an exception to the rule that remodeling in the child can be expected only if the fracture deformity is in the same plane of motion as the nearby joint. This remodeling may explain why younger children do better after fracturing of the neck of the radius than do older children.
Premature fusion of the proximal radial epiphysis does occasionally occur, but it does not appear to influence the final result.23,24 It does not lead to significant shortening of the radius nor to valgus deformity at the elbow.10,23 This is because most of the growth occurs at the distal end, and, initially, the fracture stimulates distal radius growth.
Thus, the result depends largely on the degree of restriction of motion. Composite loss of pronation, supination, flexion, and extension greater than 90 degrees leads to functional disability and a poor result. Results are directly related to the severity of the injury, concomitant injuries about the elbow, and how much physical intrusion is necessary to reduce the fracture.7,9
COMPLICATIONS
COMPLICATIONS RELATED TO THE INJURY
Radioulnar Synostosis
The dreaded complication of radioulnar synostosis (see Fig. 17-2)1,18,23,24,25,39 is associated with widely displaced fractures and is often associated with dislocation of the elbow.
Premature Fusion of the Epiphyseal Plate
Premature fusion is common but of little consequence.4,9,10,18,26
Avascular Necrosis
AVN is most common (Fig. 17-12)12,18,23,32,39 after open reduction but can occur with widely displaced fractures treated by closed reduction. Although this complication probably occurs to a certain extent in many of these serious injuries, the eventual effect is determined by the degree of loss of blood supply.
Enlargement of the Head of the Neck of the Radius and Increase in Diameter of the Neck of the Radius
This complication, which is often seen, is accompanied by compensatory enlargement of the capitellum of the humerus.23,24,26 Because growth is stimulated by the increased vascularity during the healing phase, the event is of little significance.
Ectopic Calcification
Ectopic calcification is also frequent, but it is usually limited and has little effect on the outcome.23,25,26,33,39
Impaction or Shear Injury to the Articular Surface of the Radial Head
This complication is difficult to diagnose because it occurs in fractures that produce less angulation and because the joint injury is not directly visualized,24 but it can lead to elbow stiffness and premature physeal closure. A shear injury to the head of the radius can produce an intra-articular free osteochondral fragment containing articular cartilage and a “variable amount” of epiphysis.
COMPLICATIONS RELATED TO TREATMENT
Avascular Necrosis
AVN can complicate not only widely displaced fractures but also those with lesser degrees of displacement treated by open reduction (see Fig. 17-12).12,16,18,23,39 The risk of AVN can be reduced by carefully preserving the soft tissue attachments. It is seldom seen with closed treatment.
Radioulnar Synostosis
Radioulnar synostosis also may result from less severe injuries that have undergone the trauma of open reduction or late closed reduction (see Fig. 17-2).3,10 If complete dislocation of the radial head or a dislocation of the elbow is initially unrecognized, reduction should probably be attempted up to 3 months after the injury (see Fig. 17-3). In this setting, the parents must be warned that significant stiffness will result.
Infection
Postoperative infection39 is always a concern with open procedures and can result in dissolution of the articular surface and ankylosis.
Nonunion
Nonunion is rare, but when it occurs, it is almost always after open reduction (see Fig. 17-11).37 Poor results are inevitable,4,26,39 but there may be surprisingly little pain, and excision should be deferred until skeletal maturity. Bone grafting should be considered with caution because radioulnar synostosis frequently develops. Healing of the nonunion has not necessarily led to improvement of clinical symptoms.
A rare cause of nonunion may be complete reversal of the head of the radius when the fracture surface faces the capitellum of the humerus and the articular surface faces the distal fragment.25 The radial head should be returned to its proper orientation, even if it has lost all its soft tissue attachments. It should not be excised.
AUTHOR’S PREFERRED METHOD OF TREATMENT
If the elbow region is too swollen to palpate the radial head, an assistant should stabilize the humerus and flex the elbow to 90 degrees. The forearm is rotated to full supination without applying varus strain to the elbow. Thumb pressure is applied to the anterolateral aspect of the head of the radius just lateral and distal to the cubital fossa. At the same time, the forearm is gradually rotated to the neutral position and then into full pronation. A variation on this technique has been recently described by Neher.22 The reduction is verified radiographically, preferably with a C-arm fluoroscope. The patient’s arm is placed in an above-elbow splint or cast for 3 weeks, and a follow-up radiograph is taken after 1 week.13
If reduction is still inadequate, the arm is prepared and draped, and an attempt is made to achieve a percutaneous reduction.1,5,31,34 Under fluoroscopic control, a Steinmann pin or small elevator is introduced through the skin, and the radial head is pushed into proper position (see Fig. 17-8). If reduction is achieved and is stable, with the elbow flexed 90 degrees and the forearm in a natural position, a long arm cast is applied. Radiographs confirm the maintenance of reduction. If the radial neck fracture reduction cannot be achieved, cannot be maintained, or is unstable, then an intramedullary pin is placed using the Metaizeau technique (see Fig. 17-9).
Only in the rare situation in which percutaneous reduction and the Metaizeau technique are not successful should open reduction be performed. A 5-cm incision is made, commencing on the lateral aspect of the capitellum and angling posteriorly over the radial head. This is the central portion of Kocher’s posterolateral incision at the interval between the extensor carpi ulnaris and the anconeus muscles. To avoid damaging the posterior interosseous nerve, no incision should be made distal to the bicipital tuberosity of the radius. The elbow joint is entered anterior to the anconeus muscle. Do not interfere with the orbicular ligament even if torn, or stiffness may result. The radial head is reduced into its proper position and is often sufficiently stable to make internal fixation unnecessary. If the radial head is unstable, the child’s bone is often soft enough to allow use of a heavy absorbable suture on a stout cutting needle to hold it in place, introducing the needle at the articular margin of the radial head and passing it across the fracture into the neck of the radius and through the cortex. If this does not seem feasible, one or two fine, smooth Kirschner wires are inserted at the articular margin of the radial head, across the fracture, and just through the cortex of the radial neck (see Fig. 17-12). They should be bent external to the skin, cut external to the skin, and a dressing sponge or gauze placed beneath the pins to facilitate removal in 3 weeks.
A growing child’s radial head must never be excised. Excision results in pain, increased carrying angle, radioulnar synostosis, or distal radioulnar dysfunction (see Fig. 17-5).2,3,15 If stable reduction cannot be achieved, less than optimal reduction should be accepted. Delayed radial head resection is not usually necessary but can be performed at skeletal maturity.
Immobilization following open reduction is as described for closed treatment and should be continued for no more than 3 to 4 weeks. If Kirschner wires have been used, they should be removed at this time. Reha bilitation and follow-up are exactly as described for closed treatment.
1 Bernstein S.M., McKeever P., Bernstein L. Percutaneous reduction of displaced radial neck fractures in children. J. Pediatr. Orthop. 1993;13:85.
2 Blount W.P. Fractures in Children. Baltimore: Williams & Wilkins, 1955;56.
3 Bohrer J.V. Fractures of the head and neck of the radius. Ann. Surg. 1933;97:204.
4 Conn J., Wade P.A. Injuries of the elbow. A ten year review. J. Trauma. 1961;1:248.
5 Dormans J.P., Rang M. Fractures of the olecranon and radial neck in children. Orthop. Clin. North Am. 1990;21:257.
6 Dougall A.J. Severe fracture of the neck of the radius in children. J. R. Coll. Surg. Edinb. 1969;14:220.
7 Fowles J.V., Kassab M.T. Observations concerning radial neck fractures in children. J. Pediatr. Orthop. 1986;6:51.
8 Gonzàlez-Herranz P., Alvarez-Romera A., Burgos J., Rapariz J.M., Hevia E. Displaced radial neck fractures in children treated by closed intramedullary pinning (Metaizeau technique). J. Pediatr. Orthop. 1997;17:325-331.
9 Henriksen B. Isolated fractures of the proximal end of the radius in children. Epidemiology, treatment and prognosis. Acta Orthop. Scand. 1969;40:246.
10 Jeffery C.C. Fractures of the radius in children. J. Bone Joint Surg. 1950;32B:314.
11 Jeffery C.C. Fractures of the neck of the radius in children. Mechanism of causation. J. Bone Joint Surg. 1972;54B:717.
12 Jones E.R.L., Esch M. Displaced fractures of the neck of the radius in children. J. Bone Joint Surg. 1971;53B:429.
13 Kaufman B., Rinott M.G., Tangman M. Closed reduction of fractures of the proximal radius in children. J. Bone Joint Surg. 1989;71B:66.
14 Landin L.A., Danielsson L.G. Elbow fractures in children. An epidemiological analysis of 589 cases. Acta Orthop. Scand. 1986;57:309.
15 Lewis R.W., Thibodeau A.A. Deformity of the wrist following resection of the radial head. Surg. Gynecol. Obstet. 1937;64:1079.
16 Lindham S., Hugosson C. The significance of associated lesions including dislocation in fractures of the neck of the radius in children. Acta Orthop. Scand. 1979;50:79.
17 Manoli A. Medial displacement of the shaft of the radius with a fracture of the radial neck. Report of a case. J. Bone Joint Surg. 1979;61A:788.
18 McBride E.D., Monnet J.C. Epiphyseal fractures of the head of the radius in children. Clin. Orthop. 1960;16:264.
19 Merchan E.C.R. Displaced fractures of the head and neck of the radius in children: open reduction and temporary transarticular internal fixation. Orthopedics. 1991;14:697.
20 Metaizeau J.-P., Lascombes P., Lemelle J.-L., Finlayson D., Prevot J. Reduction and fixation of displaced radial neck fractures by closed intramedullary pinning. J. Pediatr. Orthop. 1993;13:355.
21 Murray R.C. Fractures of the head and neck of the radius. Br. J. Surg. 1977;9:114.
22 Neher C.G., Torch M.A. New reduction technique for severely displaced pediatric radial neck fractures. J. Ped. Orthop. 2003;23:626.
23 Newman J.H. Displaced radial neck fractures in children. Injury. 1977;9:114.
24 O’Brien P.I. Injuries involving the proximal radial epiphysis. Clin. Orthop. 1965;41:51.
25 Rang M. Children’s Fractures. Philadelphia: J. B. Lippincott Co., 1974;112.
26 Reidy J.A., Van Gorder G.W. Treatment of displacement of the proximal radial epiphysis. J. Bone Joint Surg. 1963;45A:1355.
27 Rockwood C.A.Jr., Wilkins K.E., King R.E.. Fractures in Children, Vol. 3. J. B. Lippincott Co., Philadelphia, 1984;510.
28 Ruchelsman D.E., Klugman J.A., Madan S.S., Chorney G.S. Anterior dislocation of the radial head with fracures of the olecranon and raidal neck in a young child: A Monteggia equivalent fracture-dislocation variant. J. Orthop. Trauma. 2005;19:425.
29 Salter R.B., Harris W.R. Injuries involving the epiphyseal plate. J. Bone Joint Surg. 1963;45A:587.
30 Silberstein M.J., Brodeur A.E., Graviss E.R. Some vagaries of the radial neck and head. J. Bone Joint Surg. 1982;64A:1153.
31 Steele J.A., Kerr Graham H. Angulated radial neck fractures in children. A prospective study of percutaneous reduction. J. Bone Joint Surg. 1992;74B:760.
32 Tibone J.E., Stoltz M. Fractures of the radial head and neck in children. J. Bone Joint Surg. 1981;63A:100.
33 Vahvanen V., Gripenberg L. Fracture of the radial neck in children. A long-term follow-up study of 43 cases. Acta Orthop. Scand. 1978;49:32.
34 van Rhijn L.W., Schuppers H.A., van der Eijken J.W. Reposition of a radial neck fracture by a percutaneous Kirschner wire. A case report. Acta Orthop. Scand. 1995;66:177.
35 Vocke A.K., Von Laer L. Displaced fractures of the radial neck in children: Long-term results and prognosis of conservative treatment. J. Pediatr. Orthop. Part B. 1998;7:217.
36 Ward W.T., Williams J.J. Radial neck fracture complicating closed reduction of a posterior elbow dislocation in a child: case report. J. Trauma. 1991;31:1686.
37 Waters P.M., Stewart S.L. Radial neck fracture nonunion in children. J. Pediatr. Orthop. 2001;21:570.
38 Weber B.G., Brunner C.H., Freuler F. Treatment of fractures in children and adolescents. Berlin: Springer-Verlag, 1980;172.
39 Wedge J.H., Robertson D.E. Displaced fractures of the neck of the radius in children. J. Bone Joint Surg. 1982;64B:256.