Chapter 7 Forehead Rejuvenation
Summary
Introduction
The plastic surgery armamentarium for forehead rejuvenation has expanded considerably during the past 15 years.1–12 Whereas the focus of rejuvenation in the past was focused mainly on the face and neck, it has now become widely recognized that rejuvenation of the forehead is essential to produce a natural, well-balanced result. There is now greater emphasis on minimizing incisions and long-term side effects, such as numbness, while achieving a superior aesthetic outcome with improved patient satisfaction. Less invasive techniques have also emerged.
This chapter reviews most of the techniques available for forehead rejuvenation.
Indications
Fat injection
Preoperative History and Considerations
Patient assessment
A proper forehead length and eyebrow position with a smooth and properly contoured forehead is an integral part of facial beauty (see Chapter 1). Any disturbance of this balance undoubtedly detracts from the pulchritude of the face.
Patients with eyebrow and eyelid ptosis either consciously or subconsciously may recruit the frontalis muscle to aid in opening their eyelids.14 These two conditions should be differentiated in one of the following two ways:
Fat Injection
Since the introduction of fat injection as the means to eliminate facial lines, there has been a longstanding debate about its efficacy and reliability. In 1911 Brunings3 injected small cubes of autologous adipose tissue under the skin during rhinoplasty, but there was significant absorption of the injected fat.2 Interest in fat injection for facial rejuvenation has recently re-emerged as a result of the refinement of techniques and more reliable outcomes.15
Operative Approach
Relevant surgical anatomy
The anatomic layers of the forehead are both continuous and analogous to the five layers of the scalp.16 There is a gradual decrease in sebaceous gland content of the skin in a cephalad direction.
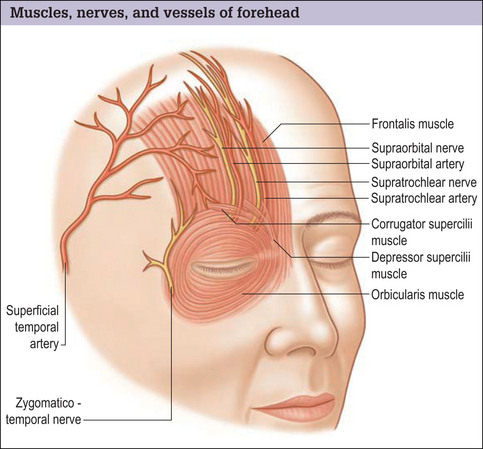
As with the scalp, the forehead skin is firmly adherent to the underlying epicranial layer. The epicranial layer is formed by the vertical fibers of the frontalis muscle anteriorly (Fig. 7.1) and the occipitalis muscle posteriorly. The galea aponeurotica spans these muscles.
Operative Technique
Complications
Fat injection is generally an uncomplicated procedure, but over- or under-injection may occur.
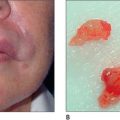
One serious complication of fat injection, which is extremely rare, is blindness.11,12 The loss of eyesight is probably related to embolization of the injected fat into the retinal artery. If this complication develops, immediate consultation with an ophthalmologist is necessary. Intentional overcorrection may result in longlasting glabellar fullness, which may ultimately resolve. This site is more privileged as a fat recipient site than most sites in terms of retention of the injected volume, and complete fat absorption is unlikely, which reduces the need for an overcorrection.
Fat Graft
Operative Approach
Since its introduction by Neubeur in 1893, the use of an autologous fat graft has been consistently popular.18 The degree of fat graft take is:
Operative technique
Complications
Fat graft may result in irregularities, infection, or accumulation of a small amount of blood around the graft, which may persist and cause the patient concern. These undesirable outcomes are unlikely.
Transpalpebral Corrugator Resection
Operative Approach
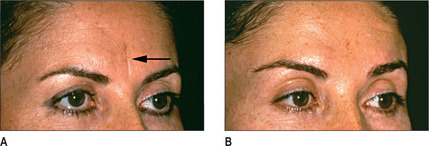
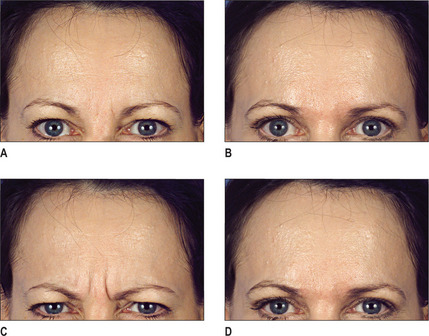
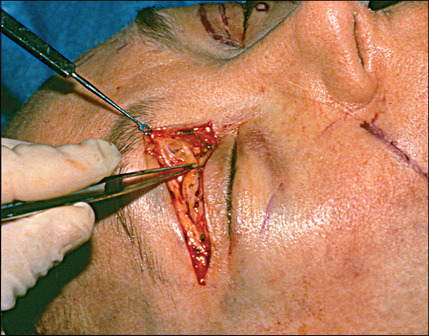
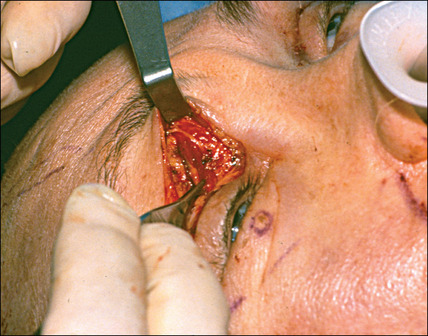
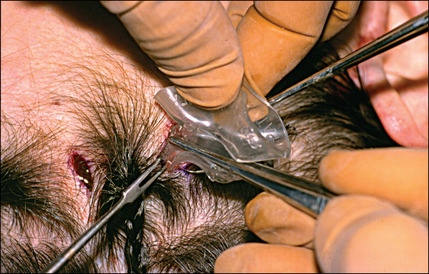
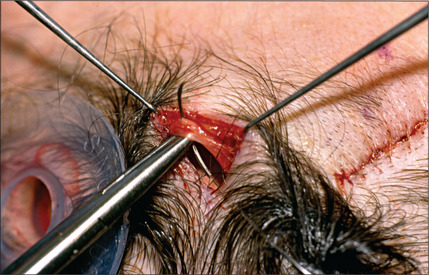
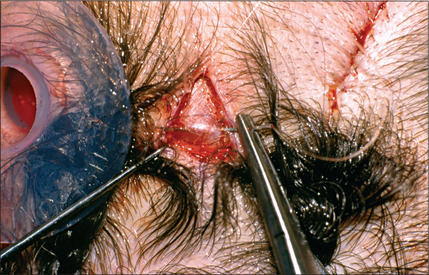
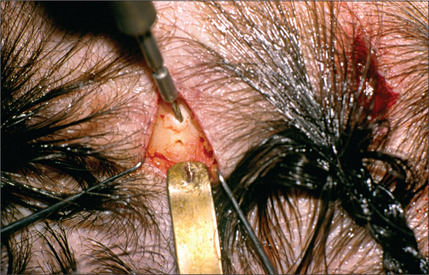
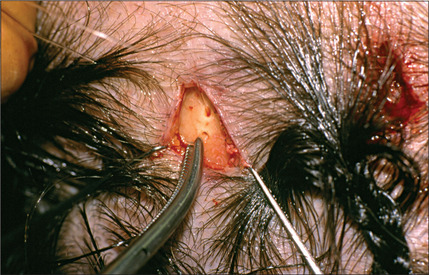
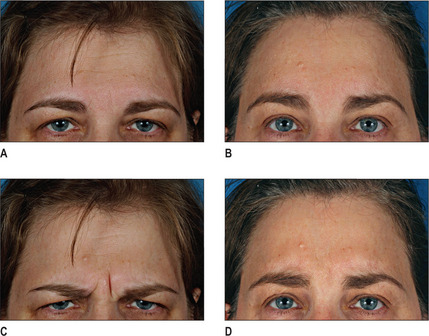
A transpalpebral incision may be used to resect the corrugator which usually results in disappearance of the frown lines (Fig. 7.4A-D).19,20 Transpalpebral corrugator resection may be performed concurrently with an endoscopic procedure to facilitate removal of the corrugator muscle. The advantages of this operation are its simplicity with direct and full exposure of nerves and muscles. The results are highly predictable and reproducible. When combined with a blepharoplasty, fat is readily available for replacement of the corrugator muscle.
Relevant surgical anatomy
Frontalis muscle
During animation, the frontalis muscle, which expresses attention, elevates the eyebrows and causes transverse wrinkling of the forehead.21 Its contraction provides a constant, cranially directed force vector on the eyebrows.
Orbicularis oculi muscle
Temporal and zygomatic branches of the facial nerve22 innervate the cephalic portion of the orbicularis oculi.
Corrugator supercilii muscle
Supraorbital and supratrochlear nerves
The supraorbital and supratrochlear nerves (see Fig. 7.1) are the terminal branches of the ophthalmic division of the trigeminal nerve (CN V) and provide sensory innervation to the forehead and scalp:
Operative technique
Endoscopic Rejuvenation
Operative Approach
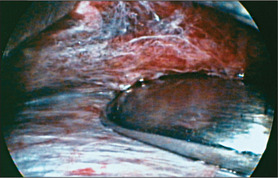
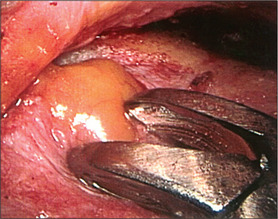
Operative technique

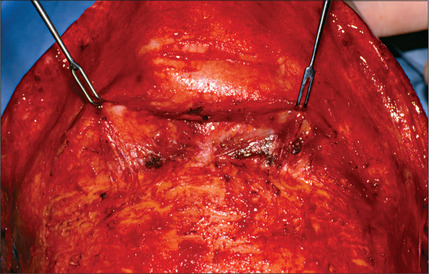
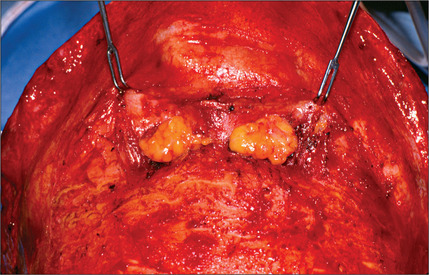
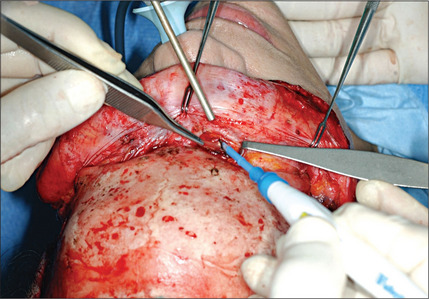
Fig. 7.13 Endoscopic forehead rejuvenation 5. Release of arcus marginalis and fibrous attachment of eyebrow.
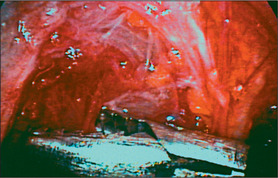
Fig. 7.14 Endoscopic forehead rejuvenation 6. Exposure and removal of the corrugator muscle using grasper.
Postoperative Care
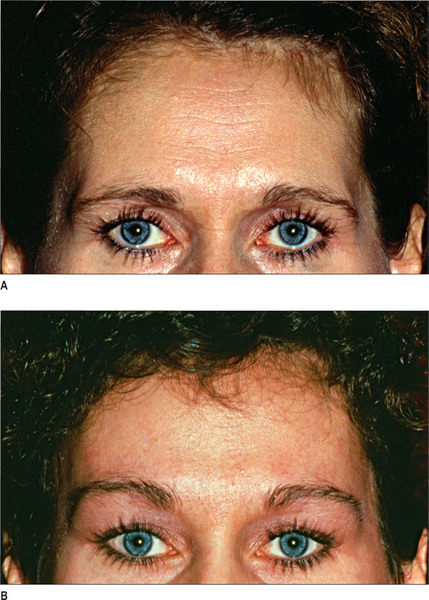
The drain is removed in 2 days and the sutures usually dissolve in approximately 7-10 days. With proper care, most patients are very pleased with the results (Fig. 7.20A-D).
Complications
An endoscopic forehead rejuvenation may result in inadequate or excessive elevation of the eyebrows, asymmetry, dimpling upon animation, undercorrection, overcorrection, or persistent paresthesia.27 A suboptimal endoscopic forehead rejuvenation result is often the consequence of under, or uneven, resection of the muscle. Uneven resection of the muscle may also cause dimpling of the forehead skin. Over-elevation of the eyebrows, most often medially due to aggressive medial soft tissue release, is the consequence of zealous dissection and aggressive repositioning of the eyebrows.27
Infection and hematoma are also complications of this surgery.
Coronal Forehead Lift
Operative Approach
Operative technique
Complications
Because of the need for further lateral dissection, the frontal branch of the facial nerves can be injured.24 Other possible complications include wide or depressed scars, recurrent brow ptosis, poor brow elevation, and intense itching of the scalp.29 The ear-to-ear coronal incision, which may result in alopecia, is the major drawback of this technique.30 Connell et al.10 warn their patients that unusual scalp sensations and intense itching may occur 3-6 months after surgery. The symptoms usually disappear after 6-9 months. Occasionally the patient may feel forehead tightness persisting for 12-18 months; regenerating sensory nerves are probably the cause of this sensation.
Adamson et al.1 noted that of the 40 patients who underwent coronal forehead lifts in his study, transient paresthesia (resolving within 6 months) occurred in 17%, a widened scar in 12%, transient frontal nerve paresis (lasting 3 weeks to 3 months) in 12%, and dysesthesia in 10%. Two patients experienced localized alopecia, and two sustained transient episodes of depression.
Postoperative Care
The sutures are allowed to dissolve. No particular postoperative care is necessary, except for application of antibiotic ointment directly on the incision and the drain site, which is continued for a period of 5-7 days. The drain is removed in 2 days and patients are allowed to wash their hair with shampoo and warm water on the third postoperative day.
Forehead Rhytidectomy with Pretrichial Incision
Forehead rhytidectomy with pretrichial incision has many advantages:
Operative Approach
Operative technique
The aesthetic goals are achieved predictably (Fig. 7.30).
Dissection in the submuscular plane
Complications
In a study of 30 patients with anterior incision forehead rejuvenation13 only two patients (who were smokers) experienced small areas of necrosis requiring revisions.
In another study by Vogel and Hoopes31, complications of subcutaneous forehead rhytidectomy included one small hematoma, temporary or clinically unnoticeable hypesthesia (66%), altered scalp sensibility (33%), persistent forehead hypesthesia or paresthesia (33%), and temporary (12%) or permanent (12%) alopecia.
To determine whether beveled or perpendicular incisions should be used when areas containing hair follicles are incised during brow elevation or facial rejuvenation, Camirand and Doucet4 studied 30 patients. For each patient, one half of the incision was beveled and the opposite half was perpendicular. Neither the patients nor the examiners were aware of the type of incision used for each side. The resulting scars were examined for visibility, nonlinearity, absence of hypopigmentation, and presence of hair in and in front of the scar. In 95% of the patients the scar on the side that was incised in a beveled fashion was judged to be more desirable.
The disadvantages of forehead rhytidectomy with pretrichial incision are the additional time required for dissection and detailed repair, and the potential for a visible scar at the hair junction on the frontal area.13
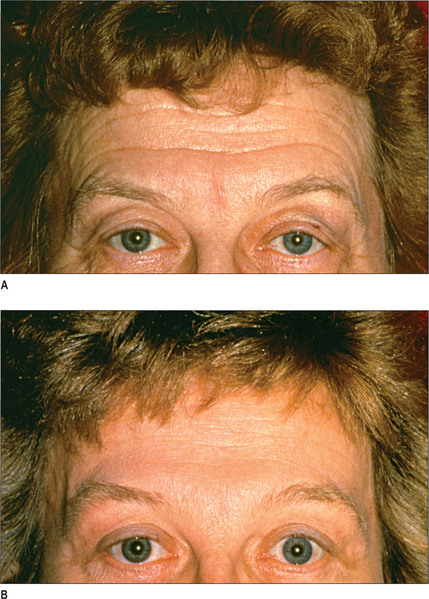
Shortening of the Elongated Forehead
The main advantage of this technique is that it is very efficacious and produces gratifying results (Fig. 7.31A&B); however, it is tedious and time consuming to perform.
Operative Approach
The forehead may become elongated as a consequence of senescence or genetic predisposition. It can also be the consequence of hair loss or may result from a coronal forehead lift. Slight or moderate elongation of the forehead can be corrected by the pretrichial incision described above. For a patient who exhibits significant forehead elongation, exceeding 1.5-2 cm beyond what is considered aesthetically pleasing, a scalp advancement is performed.32 This procedure can be combined with a forehead lift or can be utilized merely to shorten the forehead on a patient who has previously undergone an open forehead rejuvenation that has elongated the forehead.
Operative technique
Postoperative Care
If a drain is placed it is removed 2 days postoperatively. The Laser-Seal dressing is removed after 5 days. The results are usually very gratifying (Fig. 7.35).
Conclusion
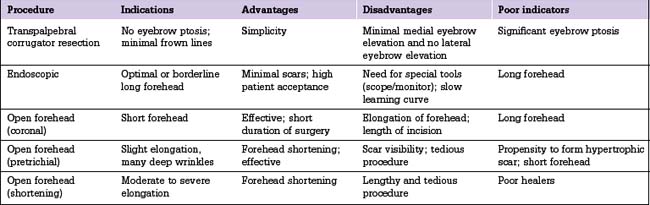
Multiple techniques are available for forehead rejuvenation (Table 7.1). For patients who seek temporary improvement of forehead wrinkles, injectable material is the optimal treatment. More lasting results may be obtained from the injection of fat or fat grafting.
1. Adamson P.A., Cormier R., McGraw B.L. The coronal forehead lift – modifications and results. J Otolaryngol. 1992;21:25-29.
2. Billings E.Jr, May J.W.Jr. Historical review and present status of free fat graft autotransplantation in plastic and reconstructive surgery. Plast Reconstr Surg. 1989;83:368-381.
3. Bruning P. Contribution a l’etude des greffes adipeuses. Bull Acad Roy Med Belgique. 1914;28:440.
4. Camirand A., Doucet J. A comparison between parallel hairline incisions and perpendicular incisions when performing a face-lift. Plast Reconstr Surg. 1997;99:10-15.
5. Carruthers A., Kiene K., Carruthers J. Botulinum A exotoxin use in clinical dermatology. J Am Acad Dermatol. 1996;34:788-797.
6. Carruthers J.D., Carruthers J.A. Treatment of glabellar frown lines with C. botulinum-A exotoxin. J Dermatol Surg Oncol. 1992;18:17-21.
7. Chajchir A., Benzaquen I. Fat-grafting injection for soft tissue augmentation. Plast Reconstr Surg. 1989;85:921-934.
8. Chajchir A., Benzaquen I., Moretti I. Comparative experimental study of autologous adipose tissue processed by different techniques. Aesthetic Plast Surg. 1993;17:113-115.
9. Coleman S.R. Long-term survival of fat transplants: controlled demonstrations. Aesthetic Plast Surg. 1995;19:421-425.
10. Connell B.F., Lambros V.S., Neurohr G.H. The forehead lift: techniques to avoid complications and produce optimal results. Aesthetic Plast Surg. 1989;13:217-237.
11. Dreizen N.G., Framm L. Sudden unilateral visual loss after autologous fat injection into the glabellar area. Am J Ophthalmol. 1989;107:85-87.
12. Egido J.A., Arroyo R., Marcos A., et al. Middle cerebral artery embolism and unilateral visual loss after autologous fat injection into the glabellar area. Stroke. 1993;24:615-616.
13. Guyuron B., Davies B. Subcutaneous anterior hairline forehead rhytidectomy. Aesthetic Plast Surg. 1988;12:77-83.
14. Hinderer U.T., Urriolagoitia F., Vildosola R. The blepharoperiorbitoplasty: anatomical basis. Ann Plast Surg. 1987;18:437-453.
15. Coleman S.R. Facial recontouring with lipostructure. Clin Plast Surg. 1997;24:347-367.
16. Michelow B., Guyuron B. Rejuvenation of the upper face: a logical gamut of surgical options. Clin Plast Surg. 1997;24:199-212.
17. Guyuron B., Majzoub M.D. Facial augmentation with core fat graft: a preliminary report. Plast Reconstr Surg. 2007;120(1):295-302.
18. Neuber G. Fat transplantation. Verl Dtsh Ges Chir. 1893;22:66.
19. Guyron B., Michelow B., Thomas T. Corrugator supercilii muscle resection through blepharoplasty incision. Plast Reconstr Surg. 1995;95:691-696.
20. Knize D.M. Transpalpebral approach to the corrugator supercilii and procerus muscles. Plast Reconstr Surg. 1995;95:52-62.
21. McGregor L. A synopsis of surgical anatomy, 4th edn, Bristol: John Wright & Sons; 1942:1-4.
22. Isse N., Fodor P.B. Forehead rejuvenation. In: Isse N., Fodor P.B., editors. Endoscopically assisted plastic surgery. St Louis: Mosby, 1996.
23. Gross C.M., editor. Gray’s anatomy of the human body, 28th edn. Philadelphia: Lea & Febiger. 1968:382-385.
24. Lorenc Z.P., Ivy E., Aston S.J. Neurosensory preservation in endoscopic forehead plasty. Aesthetic Plast Surg. 1995;19:411-413.
25. Guyuron B., Rose K. Harvesting fat from the infra temporal fossa. Plast Reconstr Surg. 2004;114:245-247.
26. Guyuron B., Kopal C., Michelow P.J. Stability after endoscopic forehead surgery using single-point fascia fixation. Plast Reconstr Surg. 2004;116:1988-1994.
27. Guyuron B. Endoscopic forehead rejuvenation. I. Limitations, flaws, and rewards [reply]. Plast Reconstr Surg. 2007;119:1116-1119.
28. Camirand A. Hairline incisions. Plast Reconstr Surg. 1999;103:736-737.
29. Ramirez O.M. The anchor subperiosteal forehead lift. Plast Reconstr Surg. 1995;95:993-1003.
30. Vasconez L.O., Core G.B., Gamoa-Bobadilla M., et al. Endoscopic techniques in coronal brow lifting. Plast Reconstr Surg. 1994;94:788-793.
31. Vogel J.E., Hoopes J.E. The subcutaneous forehead lift with an anterior hairline incision. Ann Plast Surg. 1992;28:257-265.
32. Guyuron B., Behmand R.A., Green R. Shortening of the forehead. Plast Reconstr Surg. 1999;103:218-223.