Chapter 10 Forearm, Wrist, and Hand Reduction
Forearm fractures
Overview
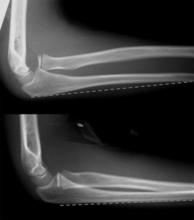
1. Fractures of both bones of the forearm (Figure 10-1) should be reduced anatomically (except in children younger than 12 years) to preserve forearm rotation.
2. A Monteggia fracture is a combination of a radial head dislocation and a fracture of the ulna. The vast majority of Monteggia fractures should be treated surgically.
a. Anatomic reduction of the ulnar fracture often results in spontaneous reduction of the radiocapitellar dislocation.
3. A Galeazzi fracture is a combination of a radial fracture and a distal radioulnar joint dislocation.
Precautions
Pearls
1. Patient positioning is key to obtaining appropriate traction. Strict positioning of the shoulder to 90 degrees and flexion of the elbow to 90 degrees allows perfectly longitudinal traction to be applied through the fracture site.
Improvisation
2. If supplies are limited, taping the forearm to a stiff board will suffice until definitive management can be arranged.
Basic Technique
Detailed Technique
1. Position the patient:
3. Prepare finger traps:
a. Attach a rolled gauze finger trap (Chapter 8) to the index and long fingers using a double-ring construct (Figure 10-5).
5. Obtain traction views (optional). Portable anteroposterior (AP) and lateral radiographs of the forearm, wrist, and elbow can be obtained in traction to evaluate the reduction.
7. Apply a splint (see Chapter 13) or a cast (see Chapter 13) while maintaining traction.
b. Flatten the ulnar border of the cast/splint with your shin (Figure 10-10) or a flat surface (Figure 10-11).
Distal radius fracture reduction
Overview
1. Many distal radius fractures, particularly in children, can be treated with closed reduction and casting (Figure 10-12).
Precautions
Pearls
1. Patient positioning is key to obtaining appropriate traction. Strict positioning of the shoulder to 90 degrees and flexion of the elbow to 90 degrees allows perfectly longitudinal traction to be applied through the fracture site.
Improvisation
1. Alternative reduction methods can be attempted if traction is not available or is ineffective.
a. Alternative 1: Use your thenar eminences to “contour” the forearm and apply traction if minimal displacement is present (Figure 10-13).
Detailed Technique
2. Prepare finger trap:
a. Attach a rolled gauze fingertrap (see Chapter 8) to the thumb using a single-ring construct (Figure 10-17).
4. Obtain traction films (optional). Portable AP and lateral radiographs of the distal radius should be obtained while the patient is in traction.
5. Perform a reduction maneuver.
a. The direction in which forces are applied depends on the type of distal radius fracture.
6. Holding your thumb on the fracture site, use your knee to help maintain the wrist in a flexed posture while traction is reapplied. This technique maintains the reduction.
Intercarpal dislocation
Precautions
Pearls
1. Patient positioning is key to obtaining appropriate traction. Strict positioning of the shoulder to 90 degrees and flexion of elbow to 90 degrees allows perfectly longitudinal traction to be applied through the fracture site.
2. Be patient! Allow at least 20 minutes for traction to result in exhaustion of countering muscles.
3. Forewarn patients that their fingers may hurt more than their wrist by virtue of the finger trap.
Detailed Technique
1. Position the patient supine on the stretcher with his or her shoulder girdle entirely off the side.
2. Prepare finger trap:
4. Perform a reduction maneuver.
5. Obtain postreduction views while the patient is in traction if possible. Portable AP and lateral radiographs of the carpals can be obtained while the patient is in traction.
6. Apply a sugar-tong splint (see Chapter 13) while maintaining the wrist in slight flexion and ulnar deviation.
Boxer’s fracture
Overview
Pearls
Detailed Technique
2. Perform a field block, nerve block, or hematoma block. An ulnar nerve block is reliable for fifth metacarpal fractures, but fourth metacarpal fractures may need a supplemental field or hematoma block.
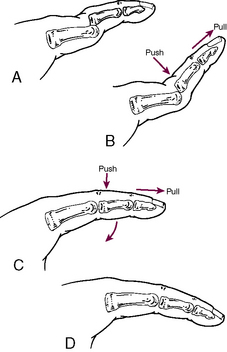
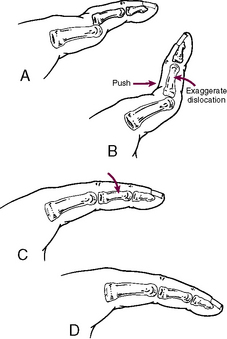
3. Perform a reduction maneuver (Figure 10-24).
Digital dislocations
Overview
2. Once reduced, most digital dislocations are stable at rest but should be protected from subsequent injury with a short course of splinting.
3. Radiographs often will demonstrate a concomitant intra-articular fracture.
a. A small fleck of bone off the dorsal or volar aspect of a joint represents a ligament or tendon avulsion and does not alter management.
b. A true fracture/dislocation involving more than 20% of the articular surface (Figure 10-26) may be inherently unstable and should prompt an urgent visit to a hand surgeon.
Pearls
1. A good block is essential to permit application of sufficient traction and force to reduce the dislocations.
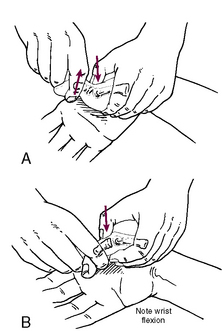
4. For thumb MP dislocations, placing the wrist and IP joint in flexion releases tension on the flexor pollicis longus and aids in the reduction (Figure 10-29).
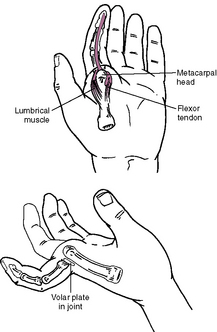
5. If a reduction cannot be achieved, consider the possibility that soft tissue (e.g., volar plate or tendons) is interposed or that the bone is buttonholed between two tendons (Figure 10-30).
Detailed Technique
4. Measure the aluminum foam splint and cut it to size (Figure 10-31). Only the involved joint should be splinted.
6. Contour the splint with an appropriate bend.
a. Dorsal dislocations (distal bone dislocates dorsally) can be splinted in flexion (Figure 10-33) or extension block splints (Figure 10-34).