Chapter 10 FOOD ALLERGIES AND INTOLERANCES
DEFINITIONS
Food allergy
An adverse reaction to food resulting from an immune-mediated response to a food protein. Food allergic reactions are usually either IgE mediated (immediate hypersensitivity e.g. urticaria) or non-IgE (cell) mediated (delayed hypersensitivity e.g. food protein enteropathy). Some allergic diseases are associated with demonstrable IgE to foods and other allergens but a causative link has not been firmly established (e.g. eosinophilic gastroenteropathy). Isolated gastrointestinal food allergies are usually either delayed or IgE-associated.
CLINICAL SYNDROMES
IgE-mediated immediate hypersensitivity
A relatively small number of foods, including cow’s milk, hen’s egg, wheat, peanut and shellfish cause the majority of IgE-mediated immediate hypersensitivity reactions. Symptoms usually occur within minutes of ingestion of the food and very rarely occur more than 2 hours following the ingestion. Symptoms involving the gastrointestinal system include abdominal pain, nausea, vomiting and diarrhoea. Immediate hypersensitivity reactions rarely involve the gastrointestinal system in the absence of other systems. The most severe form of IgE-mediated allergy is called anaphylaxis and is defined as the involvement of any two organ systems and the respiratory or cardiovascular system. Anaphylaxis is a medical emergency and can be fatal in some cases.
Food protein enterocolitis
Cell-mediated (T cell) hypersensitivity is similar to, but more severe than, food protein enteropathy. It usually begins in infancy and is most often caused by cow’s milk, but between 30% and 50% are also sensitive to soy. Chronic ingestion of the causative protein causes vomiting, bloody diarrhoea and lethargy that may lead to dehydration and acidosis. The clinical picture may mimic sepsis including an elevated blood neutrophil count. Re-exposure to the causative protein leads to a dramatic, but delayed (± 2 hours) recurrence of symptoms that may lead to shock in up to 20% of cases. The diagnosis is made through an elimination diet, re-challenge with the suspected food under medical supervision and examination of the stool for blood, white cells and eosinophils (colitis). A rise in the blood neutrophil count over 3500 cells/mL may be observed. Biopsy is usually not necessary for the diagnosis. Treatment is by avoidance of the causative food and the use of hydrolysed formula. This condition usually resolves between 2 and 3 years of age.
ASSESSMENT
History
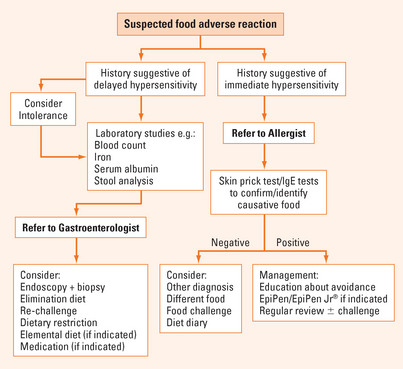
The clinical history remains the most important diagnostic tool in the assessment of a patient with a suspected adverse reaction to a food. Information relating to the temporal relationship of the symptoms with ingestion of the food may help to differentiate immediate from delayed hypersensitivity reactions. Most IgE-mediated adverse reactions to foods occur within 2 hours following the ingestion of a food, although a very small proportion of IgE-mediated reactions may be delayed for up to 6 hours. Non-IgE mediated adverse reactions occur much later, even up to 72 hours after the ingestion of a food. Other important factors in the history include previous exposure to the suspected food, with or without a reaction, the reproducibility of the adverse reaction on re-exposure to the food, the amount of food ingested and the severity of the adverse reaction. The severity of the reaction on history may help to determine further management, e.g. anaphylaxis may require the prescription of self-injectable adrenaline (EpiPen® and EpiPen Jr®). In some cases it may be recommended that the patient keep a diet diary. This may be particularly useful in cases of suspected delayed adverse reactions where the causative food, or the definite relationship between a food and the onset of symptoms, is difficult to determine.
Tests for immediate hypersensitivity
Specific IgE levels
Food-specific IgE is measured in kilounits per litre (kU/L) of serum. Most commercial assays have a range of 0.35–100 kU/L. The sensitivity of a negative food-specific IgE assay (<0.35 kU/L) is >95%, but the specificity of a positive test (>0.35 kU/L) is poor. Various diagnostic cut-off levels of food-specific IgE have been proposed but, like skin prick testing, one should be cautious about diagnosing immediate hypersensitivity to food based only on a specific IgE cut-off in the absence of a supportive history and when specific IgE levels have also not been shown to correlate with the severity of a reaction.
MANAGEMENT
Treatments for the specific disorders are mentioned above. In general the management of food adverse reactions involves the avoidance of the causative food. A very important aspect of the management of food adverse reactions is the appropriate education of the patient or, in the case of children, their parents or carers. Patients should be told the estimated risk of a severe, life-threatening reaction, especially in the case of IgE-mediated food allergy. They should know how to administer emergency medications (e.g. an EpiPen®), if needed, and how to access medical care urgently. Most importantly, patients need to understand that avoidance is the mainstay of treatment. They should be educated to check for the presence of the causative food in all new foods, which may often involve thorough reading of food labels. Additional support, such as liaising with schools or child care in the case of children, is often necessary. Finally, all patients with food adverse reactions should receive regular medical review to ensure that management strategies, such as restricted diets, are still necessary and appropriate.
SUMMARY
Food allergy of all types may affect up to 6% of children and 4% of adults (Figure 10.1). The clinical syndromes induced are:
In general, management involves avoidance of the causative food. Appropriate education of the patient or, in the case of children, their parents is pivotal.
Bock SA, Sampson HA. Evaluation of food allergy. In: Leung DYM, Sampson HA, Geha RS, et al, editors. Pediatric allergy principles and practice. St Louis: Mosby; 2003:478-487.
Moneret-Vautrin AD. Gastroinestinal allergy in adults. Eur J Gastroenterol Hepatol. 2005;17:1293-1297.
Sampson HA. Update on food allergy. J Allergy Clin Immunol. 2004;113(5):805-819.
Sampson HA, Sicherer SH, Birnbaum AH. AGA technical review on the evaluation of food allergy in gastrointestinal disorders. Gastroenterology. 2001;120:1026-1040.