Chapter 34 Fluids and Electrolytes
1 How do you estimate the extent of dehydration in children?
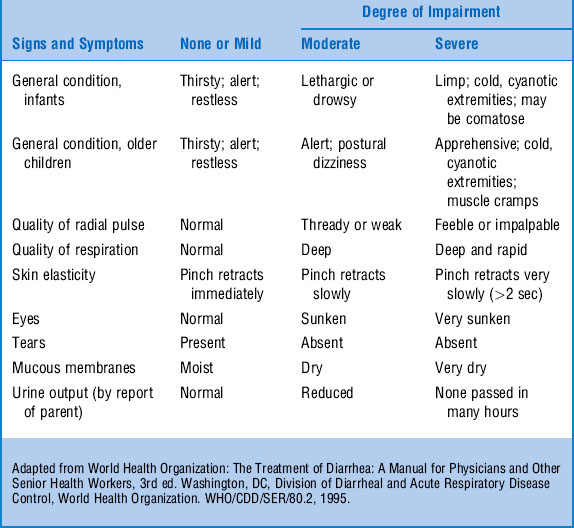
Since serial weights on the same scale are rarely available in the emergency department (ED) setting, rely on the physical examination to estimate the degree of fluid loss (Table 34-1).
2 What are the most reliable clinical examination findings that help you predict how dry a child has become?
Steiner MJ, DeWalt DA, Byerley JS: Is this child dehydrated? JAMA 291:2746–2754, 2004.
8 At what rate should fluids run on a child who has orders to receive nothing by mouth? How is this maintenance rate adjusted for the dehydrated child?
1 The first objective in treating a child with severe dehydration is to restore intravascular volume and treat shock, regardless of etiology.
2 In all children receiving IV fluids, the serial electrolytes and urine output should be monitored and fluid rates adjusted on the basis of the child’s hydration status, urine output, and presence or absence of increased ADH.
3 Compared with IV therapy, oral rehydration therapy is effective in treating dehydration in most children, has fewer complications, and may be faster.
9 Will use of hypotonic maintenance solutions cause dangerous hyponatremia?
Hatherill M: Rubbing salt in the wound. Arch Dis Child 89:414–418, 2004.
15 When should oral rehydration not be used?
 Inability to tolerate oral fluids because of vomiting
Inability to tolerate oral fluids because of vomiting
 Altered mental status with risk of aspiration
Altered mental status with risk of aspiration
 Short gut or carbohydrate malabsorption, which limit absorption
Short gut or carbohydrate malabsorption, which limit absorption
Batra B, Stanton B: Oral rehydration therapy, 2006. Available at www.uptodate.com.
21 How do I treat hyperkalcemia?
The type and speed of treatment depend on the potassium levels and electrocardiogram changes. Potassium may be forced out of the cell by acidosis. Treatment of the acidosis causes potassium to return to the cell and out of the serum (Table 34-2).
| Potassium Level (mEq/dL) | ECG Finding | Treatment |
|---|---|---|
| <7.0 | Peaked t waves only, or normal | Remove K source, treat acidosis, Kayexalate (1g/kg orally or rectally) every 4–6 hr |
| 7.0 | Widespread ECG changes without arrhythmia | Glucose (0.5 g/kg or 5 mL/kg of D10 over 30–60 minutes) and insulin (0.1 U/kg over 30–60 minutes) plus bicarbonate (2 mEq/kg over 30–60 minutes) |
| 8.0 | Arrhythmia | 10% calcium gluconate (0.5 mL/kg over 2–5 minutes with ECG monitoring, discontinue if heart rate <100 beats per minute) plus glucose and insulin, bicarbonate as above |
ECG = electrocardiogram.