Flap Classification and Design
Terminology
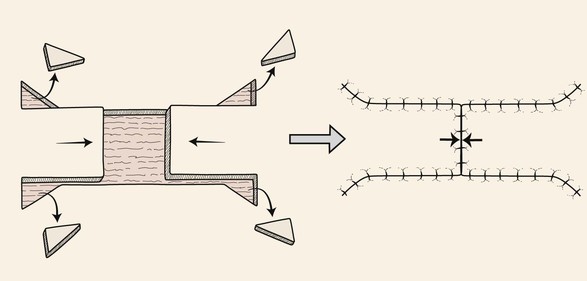
The primary defect is the wound to be closed by a local cutaneous flap. In this book, the majority of wounds shown have resulted from employing the micrographic (Mohs) surgical techniques to remove skin cancer. A secondary defect is the wound created when a skin flap is transferred to repair the primary defect (Fig. 6-1). The transfer of every cutaneous flap from its in situ position results in a secondary defect. The challenge of reconstructive surgery is to design a flap that places the secondary defect in the most advantageous location. This usually translates into harvesting of the flap from areas of the face and neck that have greater skin laxity.
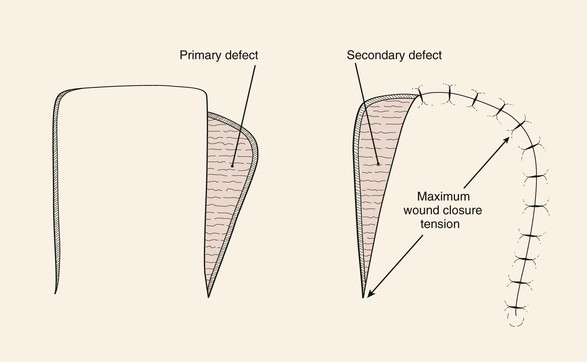
FIGURE 6-1 Movement of cutaneous flap used to repair primary defect creates secondary defect. (From Swanson NA: Classification, definitions, and concepts in flap surgery. In Baker SR, Swanson NA, editors: Local flaps in facial reconstruction, St. Louis, Mosby, 1995.)
When a skin flap is transferred to a defect, the motion of the flap is considered the primary tissue movement of the repair. This usually occurs by sliding or pivoting of tissue. Secondary tissue movement is the displacement of skin surrounding the defect toward the center of the primary defect. The vector of movement is typically in the opposite direction of the vector of movement of the flap. By necessity, there is also skin movement toward the donor site of the flap to close the secondary defect. Therefore, a combination of primary and secondary tissue movement occurs when a wound is repaired with a skin flap (Fig. 6-2). In a region where a primary defect is adjacent to a mobile facial structure, secondary tissue movement may result in distortion of these structures. Facial structures that have visible margins, such as the eyelids, lips, and nostrils, are particularly susceptible to distortion by secondary tissue movement. The stronger the attachments of facial structures to the underlying bone, the less propensity for distortion. For example, the earlobe is more likely to be deformed by secondary tissue movement than the tragus is.
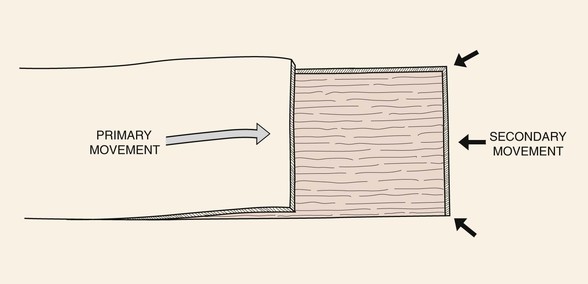
FIGURE 6-2 Combination of primary and secondary tissue movement occurs when a wound is repaired with a skin flap.
In part, the degree of wound closure tension is related to skin extensibility. Skin extensibility is the lengthening of skin under tension due to stretching of elastic fibers. There are directional variations in skin extensibility.1 That is, skin is more extensible when the vector of strain is in a certain direction. For this reason, it is advantageous to recruit skin for repair of a wound in areas of maximum skin extensibility. These areas are identified by the lines of maximum extensibility (LME).
Relaxed skin tension lines (RSTLs) are intrinsic to facial skin. RSTLs result from orientation of collagen fibers of the skin and are manifested in the aging face as skin creases and wrinkles (Fig. 6-3). RSTLs are perpendicular to LME. The orientation of skin excisions and repair of wounds are usually made parallel to RSTLs when possible (Fig. 6-4). Orienting them this way places the maximum wound closure tension parallel to LME and perpendicular to RSTLs. This orientation results in wound repair that is performed with the least amount of wound closure tension. Minimal wound closure tension is extremely beneficial in minimizing the appearance of facial scars. A converse of this is that incisions made at right angles to RSTLs usually heal with wider and more visible scars.
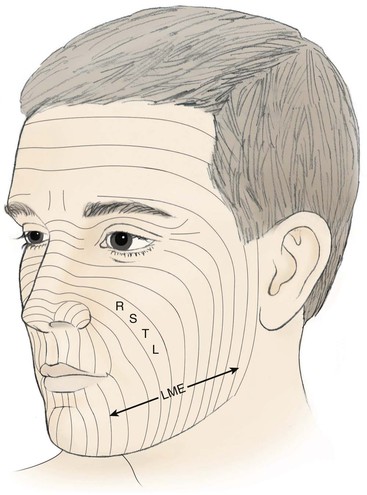
FIGURE 6-3 Relaxed skin tension lines (RSTLs) of face. Lines of maximal extensibility (LME) are perpendicular to RSTLs.
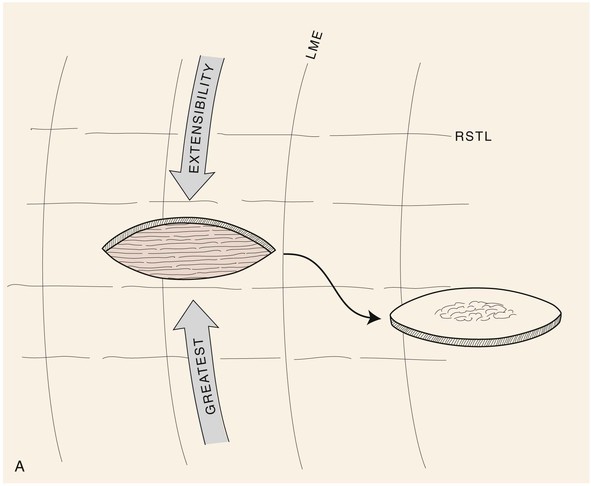
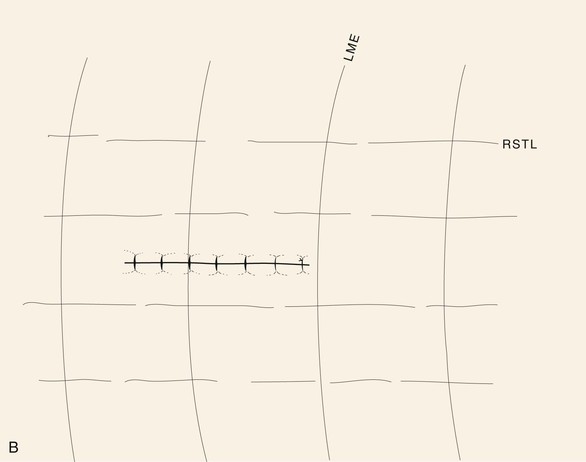
FIGURE 6-4 A, B, Orientation of skin excisions and repair of wounds are made parallel to RSTLs when possible.
An important factor that may limit skin expansion is the attachments of the skin to underlying structures, such as fascial or aponeurotic connections to the skin. Skin expansion is resisted by structures that anchor the skin by aponeurotic or tendinous insertions in bone. Examples of these include medial and lateral canthus, bony orbital rim, zygomatic arch, and malar eminence. Undermining of the skin reduces wound closure tension and more widely distributes skin deformation. Undermining releases the attachments of the skin to the underlying fascia, allowing the skin to become more expansible. Moderate skin undermining is beneficial in reducing wound closure tension. However, extensive skin undermining is not usually helpful in further reducing the wound tension, although it may assist with tissue draping and reduction in secondary tissue movement.
Flap delay is a means of increasing the blood flow to a flap. Delay is accomplished by incising all or a portion of the flap and elevating all or a portion before returning the flap to its in situ position. The incisions are sutured, and the flap is left in place usually for 10 to 14 days before the flap is transferred to a recipient site. Delay results in an enhanced circulation to the flap, probably by the closing of arteriovenous shunts and the realignment of the vasculature in the subdermal plexus. Delay is rarely used with local flaps of the face because of the overall rich blood supply to facial skin. Delay is reserved for particularly large flaps used to repair major facial defects in situations in which skin vascularity has been compromised by irradiation or previous surgery and, on occasion, in patients using tobacco.
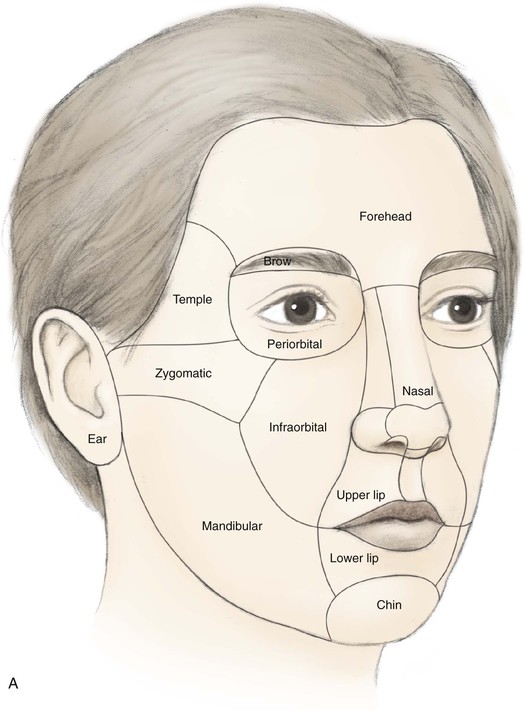
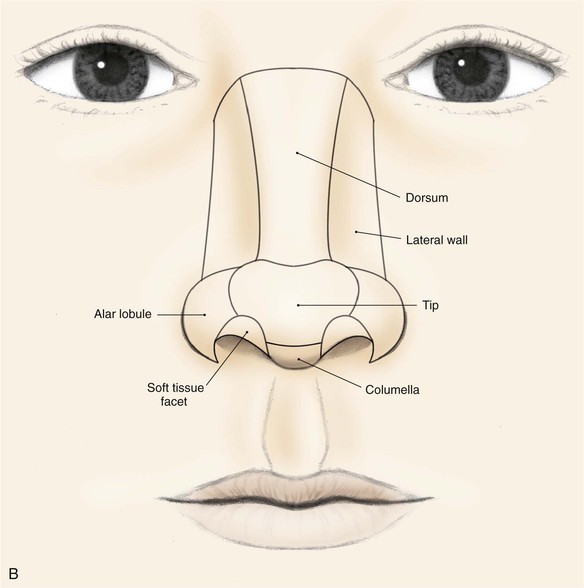
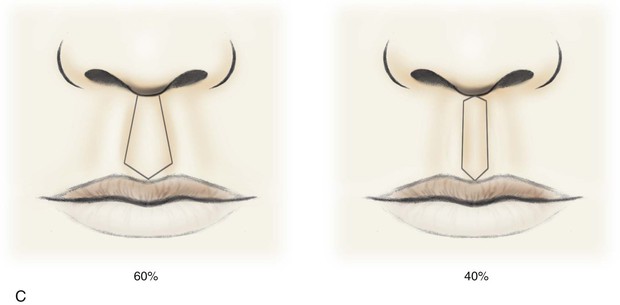
The face can be divided into specific areas or aesthetic regions, which are covered by skin that has common characteristics. These skin characteristics include thickness, quantity of subcutaneous fat, degree of adherence to underlying fascia, color, texture, and hair growth. Coincidentally, these facial areas are separated from each other by ridges or valleys in the skin created by the facial skeleton or musculature. These ridges and valleys are known as aesthetic borders and are identified by facial landmarks including eyebrows, melolabial creases, mental crease, philtral crests, vermilion borders, and anterior hairline. Aesthetic regions and their accompanying borders provide form, character, and individual uniqueness to the face. The principal aesthetic regions of the face are forehead, eyelids, cheeks, nose, lips, mentum, and auricles (Fig. 6-5). Some aesthetic regions may be divided into a number of components known as aesthetic units, which are separated by borders somewhat less discrete than those that delineate aesthetic regions. The forehead may be divided into central and temporal units. The cheek is divided into infraorbital, zygomatic, buccal, and parotid masseteric units. The upper lip is divided into philtrum and paired lateral units. The lower third of the face is divided into labial and mental units. The nose is particularly suited for division into aesthetic units because of its complex topography. It may be divided into nine aesthetic units that include dorsum, paired sidewalls, tip lobule, paired nasal facets, paired alae, and columella. These units are highlighted when incident light is cast on the nasal surface, creating shadows along the borders of each unit and topographic landmarks.2 As with facial aesthetic units, the framework of the nose supporting the overlying skin is primarily responsible for variations in light reflections and gives rise to the aesthetic border between the nasal units.
Local Flap Classification
Cutaneous flaps may be classified by the nature of their blood supply (random vs. arterial), by configuration (rhomboid, bilobe), by location (forehead, cheek, lip), and by the method of transferring the flap. Flaps classified by location are identified by the region of the body from which they are harvested. This location may be near or considerably removed from the primary defect. When they are removed from the defect, such flaps are transferred either by microvascular surgery or by staged movement of the flap toward the recipient site. On the basis of location, flaps are classified as local, regional, or distant. A local flap is one in which tissue immediately adjacent to or near the primary defect is used to cover the defect. The majority of skin flaps discussed in this textbook are local flaps. In regard to facial reconstruction, a regional flap is one in which tissue is harvested from a site not located on the face, scalp, or neck. However, the pedicle is sufficiently long to enable the flap to reach the primary defect. An example of a regional flap for facial repair is a deltopectoral flap transferred from the anterior chest wall to repair a defect of the lip or cheek. A distant flap is one that is harvested from sites so removed from the face that the pedicle is not sufficiently long to enable the flap to reach the face. Distant flaps are usually transferred to the face as free flaps, sometime referred to as microsurgical flaps. The blood vessels of their pedicle are connected to vessels in the head or neck by microvascular surgical techniques. Another way of transferring distant flaps to the face is by staging tubed flaps, in which the pedicle is “walked” toward the recipient site. This method has been abandoned since the development of microsurgical techniques.
The most common way to classify flaps on the basis of blood supply is to categorize them as random or axial pattern flaps. This is discussed in detail in Chapter 2. Random pattern flaps are based on the rich perforating vascular plexus of the skin (Fig. 6-6). They do not have a named blood vessel providing vascularity to the flap. In contrast, axial pattern flaps depend on a named artery for the majority of their blood supply (Fig. 6-7). These vessels parallel the linear axis of the flap and are usually located in the subcutaneous fat directly beneath the skin of the flap. Most axial pattern flaps have a degree of random pattern vascularity to their distal portion. The majority of cutaneous flaps of the face are random pattern. The most common axial pattern flap harvested from the face is the paramedian forehead flap based on the supratrochlear artery and vein.
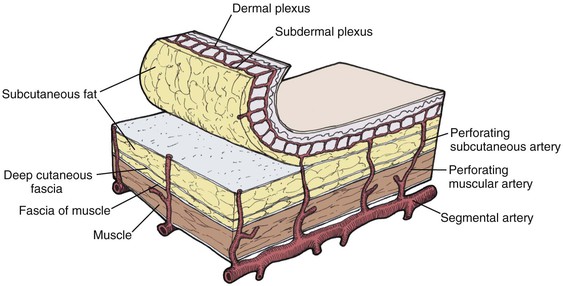
FIGURE 6-6 Random pattern flaps based on subcutaneous and intradermal vascular plexuses that supply blood to skin. (From Swanson NA: Classification, definitions, and concepts in flap surgery. In Baker SR, Swanson NA, editors: Local flaps in facial reconstruction, St. Louis, Mosby, 1995.)
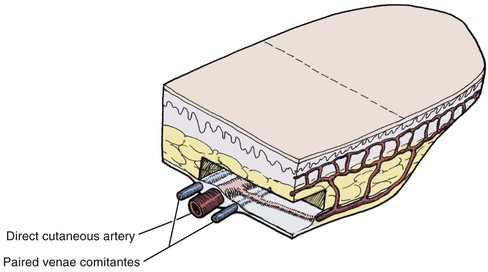
FIGURE 6-7 Axial pattern flaps based on named artery for blood supply. Most axial pattern flaps have a degree of random pattern to the distal portion. (From Swanson NA: Classification, definitions, and concepts in flap surgery. In Baker SR, Swanson NA, editors: Local flaps in facial reconstruction, St. Louis, Mosby, 1995.)
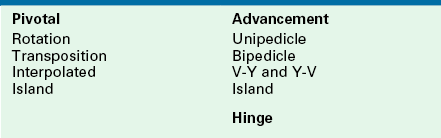
Classifying flaps by method of transfer, which is to say method of tissue movement, is usually the most convenient way of discussing flaps relative to their use in repair of facial cutaneous defects (Table 6-1).3–5 This classification divides local flaps into pivotal, advancement, and hinge. Advancement in the majority of situations depends on stretching the flap skin in the direction of flap movement. Such flaps are subjected to an increase in wound closure tension. In contrast, pivotal flaps rotate about a point at their base and in their purest form are not stretched. Thus they are not subjected to wound closure tension greater than the natural tension of the remaining facial skin, although the repair of the donor site of the flap is subjected to increased skin tension. However, in most circumstances in which pivotal flaps are used, tissue movement is achieved through a combination of pivoting and advancement. That is, movement of most pivotal flaps is aided by stretching (advancement) of the flap skin. Surgeons often speak of combined mechanisms of tissue movement, such as “advancement rotation flap.” For clarity, the major mechanism of tissue movement should dictate the term given to describe a particular flap, unless both mechanisms are of approximately equal importance.
Pivotal Flaps
There are four types of pivotal flaps: rotation, transposition, interpolated, and island. All pivotal flaps are moved toward the defect by pivoting the flap around a fixed point at the base of the pedicle. Except for island flaps skeletonized to the level of their nutrient vessels, the greater the pivot, the shorter is the effective length of the flap (Fig. 6-8). Pivoting a flap with a cutaneous pedicle 45° from its in situ position reduces the effective length 5%. A 90° and 180° pivot reduces effective length by 15% and 40%, respectively.6 The reduction in effective length must be accounted for when pivotal flaps are designed so that greater pivoting requires a longer design of the flap. As the flap turns in an arc around its relatively fixed pivotal point, redundant tissue, known as a standing cutaneous deformity (dog ear), develops at the base. Similar to effective length, there is a positive correlation between the degree of pivoting and the size of the standing cutaneous deformity. The greater the pivot of the flap, the larger the deformity that occurs. Thus, increasing the flap’s pivot will change the flap’s shape, shorten the effective length, increase wound closure tension, and deform the flap’s base by development of a standing cutaneous deformity. To limit these restricting factors, a flap’s arc of pivot should not exceed 90° whenever possible.
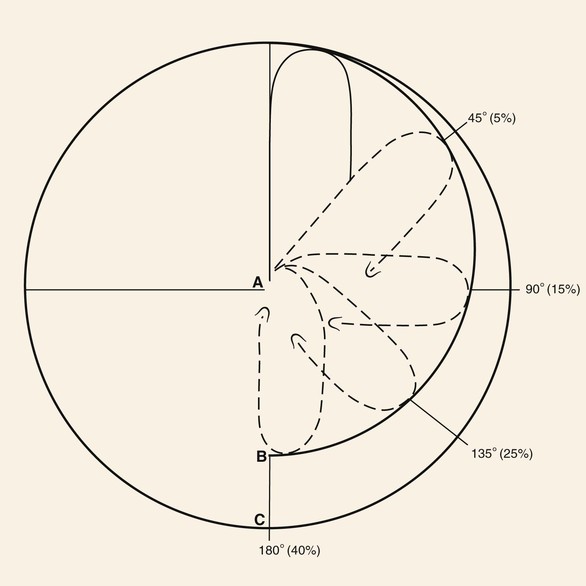
FIGURE 6-8 As transposition flap pivots, flap changes shape and shortens as standing cutaneous deformity increases. As flap pivots about point A, effective length of flap decreases along circumference B rather than C. Approximate percentage of shortening as related to degree of pivotal movement is in parentheses. (From Panje WR, Minor LB: Reconstruction of the scalp. In Baker SR, Swanson NA, editors: Local flaps in facial reconstruction, St. Louis, Mosby, 1995.)
Rotation Flaps
Rotation flaps are pivotal flaps with a curvilinear configuration. They are designed immediately adjacent to the defect and are best used to close triangular defects. In such instances, the triangle-shaped defect is covered by a portion of the standing cutaneous deformity, thus facilitating the pivotal movement of the flap (Fig. 6-9). This flap usually makes use of some advancement, and when it does, the vector of greatest wound closure tension is along a line from the base of the flap to a distal point of the curvilinear border. When no advancement is used in movement of the flap, animal studies have shown the greatest wound closure tension to be at the closure site perpendicular to the periphery of the flap, not across the long length of the flap.1 These studies have also demonstrated minimal mechanical benefit at the defect site in extending the arc of rotation flaps beyond 90° from the axis of the primary defect. However, there may be benefit in extending the incision to accommodate redraping of skin. A back cut at the base of the flap shifts the position of the pivotal point and thus changes the wound closure tension vector as well as the location of the standing cutaneous deformity.
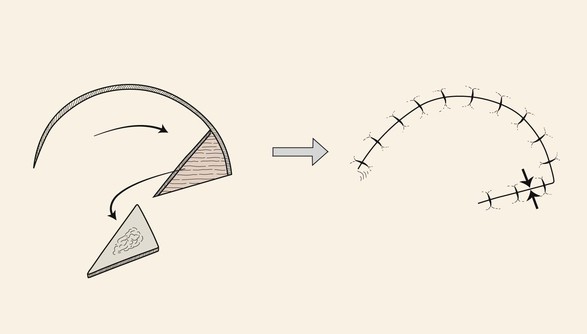
FIGURE 6-9 Rotation flaps are pivotal flaps with curvilinear configuration. They are designed immediately adjacent to defect and are best used to repair triangular defects. Opposing arrows indicate greatest wound closure tension.
Disadvantages of rotation flaps are relatively few. The defect itself must be somewhat triangular or must be modified by removal of normal tissue to create a triangular defect. The configuration of the flap includes a right angle at the distal tip, and the surgeon must take care in positioning the tip so that it is not subjected to excessive wound closure tension and vascular compromise. The curvilinear incision necessary to create the flap does not easily lie in RSTLs (see Fig. 6-3). As with all pivotal flaps, rotation flaps develop standing cutaneous deformities at their base that may not be removed without compromising vascularity. A second-stage revision in which the standing cutaneous deformity is removed may be necessary.
Transposition Flaps
In contrast to rotation flaps, which have a curvilinear configuration, transposition flaps have a linear configuration. Both are pivotal flaps moving about a pivotal point. Both flaps develop standing cutaneous deformities at their bases, and as a consequence, their effective length decreases as they pivot. This reduction in effective length must be considered in designing such flaps. Rotation flaps must be designed in such a way that one border of the flap is also a border of the defect for which it is intended for repair. Like rotation flaps, transposition flaps may be designed so that one border of the flap is also a border of the defect (see Fig. 6-1); however, it may also be designed with borders that are removed from the defect (Fig. 6-10). In this circumstance, only the base of the flap is contiguous with the defect. The area of greatest wound closure tension is at the closure site of the secondary defect adjacent to the base of the flap. Depending on whether the flap is stretched and the degree of stretching, the greatest wound closure tension may be along a vector from the pivotal point to the most peripheral border of the flap. The ability to construct a flap some distance from the defect with its axis independent from the linear axis of the defect is one of the greatest advantages of transposition flaps. This fact enables the surgeon to recruit skin at variable distances from the defect, selecting donor sites with the greatest skin elasticity or redundancy. In addition, the ability to select a variable site for harvest of a flap may allow the selection of a donor site that will provide the best possible scar camouflage or even the ability to hide the scar in aesthetic boundaries.
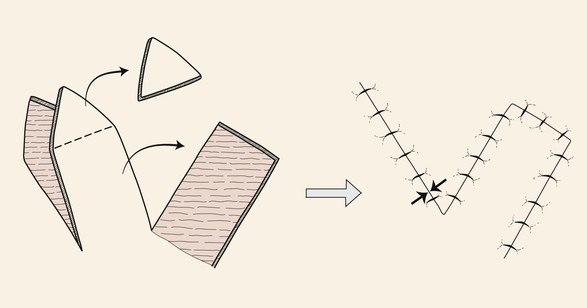
FIGURE 6-10 Transposition flaps are pivotal flaps with linear axes. The base of the flap is contiguous with the defect. Greatest wound closure tension is at closure site of donor defect (opposing arrows).
Transposition is the most common method of transferring local flaps to skin defects of the head and neck. A transposition flap is a reconstructive option for small to medium-sized defects of almost any conceivable configuration or location, thus making it the most useful of local flaps in facial reconstruction (Fig. 6-11).





FIGURE 6-11 A-E, Transposition flaps are common reconstructive options for small to medium-sized cutaneous cheek defects. A, Lentigo maligna outlined by sutures. Transposition flap designed. B, Skin lesion excised, standing cutaneous deformity (SCD) marked for excision at base of flap. C, Flap in place. D, E, At 1 year after surgery. No revision surgery performed.
Two types of transposition flaps frequently used are rhombic flaps and bilobe flaps. Rhombic flaps depend on advancement for part of their tissue movement, but the majority of movement is pivotal. A rhombus is an equilateral parallelogram. A rhombus defect may be thought of as two equilateral triangles placed base to base to form a rhombus with adjacent angles of 60° and 120°. All sides and the short diagonal of the defect must be equal in length in a 60°–120° rhombus defect and flap (Fig. 6-12). Once the 60°–120° rhombus defect has been created with all sides equal in length, the flap is designed by directly extending the short diagonal a distance equal to all other sides. This creates the first side of the flap. The second side of the flap, again equal in length to all other sides, is drawn parallel to one of the adjacent borders of the defect.7
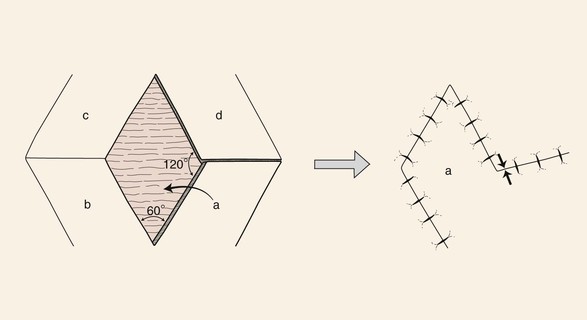
FIGURE 6-12 For every rhombus defect, four potential flaps may be designed. Greatest wound closure tension is at donor site (opposing arrows).
The greatest wound closure tension with a rhombus flap is at the donor site and has been calculated to be 20° from the short diagonal line across the base of the flap.7 Wide undermining of the surrounding tissue has minimal effect on the wound closure tension. Thus, in designing the flap, skin mobility and extensibility are important. Understanding the vector of the resultant wound closure tension is critical to avoid distortion of surrounding structures. For every rhombus defect, four potential flaps may be designed (Fig. 6-12). The surgeon can quickly visualize the resulting scar configuration and approximate vector of maximum wound closure tension by drawing the flap and then covering the two parallel sides of the flap with his or her fingers.
The design of the rhombus flap is more complex than that of most other facial skin flaps because of the geometry and option of placing the flap in four separate locations about a rhombus defect. The author does not use the rhombus flap or its variations frequently, primarily because approximately half of the entire length of the scar that results from use of the flap is not parallel or does not lie within RSTLs. This disadvantage is most important in the area of the forehead, where skin creases are more prominent. RSTLs are less important in the cheek, where creases are not as prominent, the skin is thinner, and the resulting scar from the use of a rhombus flap tends to blend better with adjacent skin.
The bilobe flap is a double transposition flap that shares a single base. Each lobe of the flap has a separate pivotal point, and thus each has a standing cutaneous deformity.8 It was originally designed for repair of nasal defects but has frequently been used to reconstruct cheek defects as well. In the classic design of the bilobe flap, the axes of the first and second lobes as well as the defect were all separated by an angle of 90° (180° total) (Fig. 6-13). This design transferred the tension of the wound closure through a 90° arc, which is more than the usual 45° to 60° arc of a single transposition flap. This greater movement about a pivotal point, together with the use of two tissue flaps, assists in minimizing wound closure tension of the primary and secondary defects.
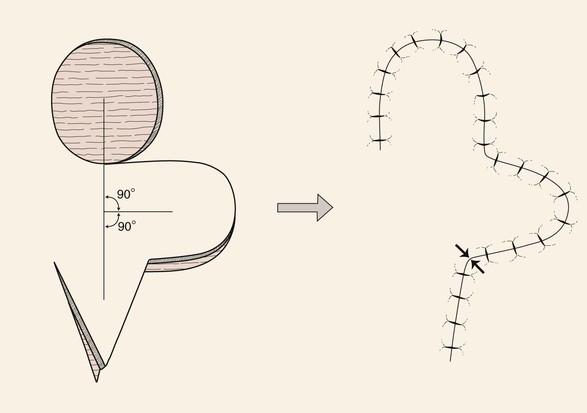
FIGURE 6-13 Classic design of bilobe flap. Axes of first and second lobes and defect, separated by 90° angles. Design transferred wound closure tension through 90° arc, compared with 45° to 60° arc of single transposition flap. Opposing arrows indicate greatest wound closure tension.
The major disadvantage of the bilobe flap is that the majority of the incision necessary to create the two lobes of the flap produces scars that do not parallel RSTLs. However, the configuration of the lobes may often be designed to have an angular shape that may conform to RSTLs better than curvilinear designs. The resulting scar of bilobe flaps is also lengthy because of the requirement of elevating two lobes.
Interpolated Flap
The interpolated flap, like the transposition flap, is transferred by pivotal movement and has a linear configuration, but it differs from transposition flaps in that its base is not contiguous with the defect. Thus the pedicle must cross over or under intervening tissue (Fig. 6-14). If the pedicle passes over intervening tissue, the pedicle must subsequently be divided in a second surgical procedure. This is referred to as insetting the flap. Two surgical stages are thus required, and this is the greatest disadvantage of such flaps. On occasion, the pedicle can be de-epithelialized or reduced to subcutaneous tissue only (island flap) and brought under the intervening skin to allow a single-stage reconstruction. Passing flaps through a subcutaneous tunnel may compromise the vascularity of the pedicle or create a contour deformity along its path.
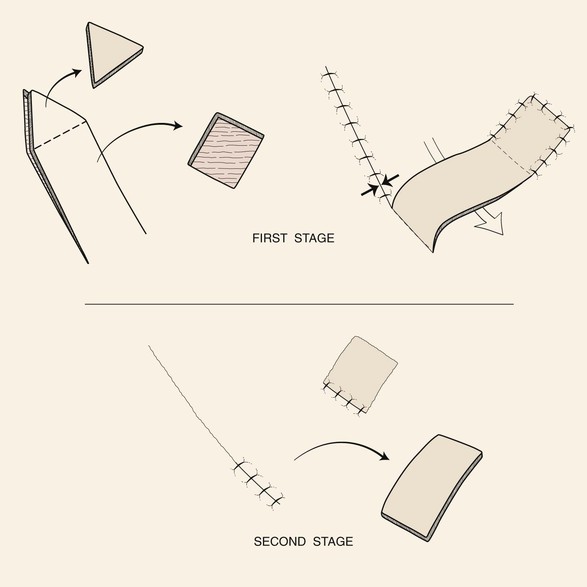
FIGURE 6-14 Base of interpolated flap is not contiguous with defect. Pedicle passes over or under intervening tissue. If it is over intervening tissue, the pedicle is divided in a second surgical stage. Opposing arrows indicate greatest wound closure tension.
The paramedian forehead flap used to repair large defects of the nose is the archetype of interpolated flaps (Fig. 6-15). This flap is exceedingly reliable because of its axial blood supply based on the supratrochlear artery and vein. The flap is designed so that the vessels located in the subcutaneous tissue plane extend along the axis of the flap, providing an ample blood supply to the skin.9 Because of this, the portion of the flap cephalic to the level of the eyebrow and extending up to the level of the anterior hairline can be trimmed of its frontalis muscle and most of the subcutaneous fat without harming the blood supply to the skin of the flap.10



FIGURE 6-15 A, Interpolated paramedian forehead flap. B, Pedicle divided and flap inset during second-stage procedure. C-F, Preoperative views of nasal tip defect and postoperative views after reconstruction with interpolated paramedian forehead flap shown in A. No revision surgery performed.
Similar to the interpolated paramedian forehead flap used for nasal reconstruction, the melolabial interpolated flap transferred from the cheek to the nose is a reliable flap for reconstruction of alar defects. The flap may be based on a cutaneous pedicle (Fig. 6-16) or subcutaneous tissue pedicle (Fig. 6-17). Regardless of the nature of the pedicle, it is divided and the flap is inset at the nose 3 weeks after the flap is transferred to its recipient site. Unlike the forehead flap, the cheek flap has a random blood supply and cannot safely be thinned of as much of its subcutaneous fat as the forehead flap. Interpolated flaps have the advantage of crossing over rather than through the intervening tissue between flap donor site and the defect, so they do not distort boundaries between aesthetic regions of the face. This ensures a completely natural-appearing border between the cheek or forehead and the nose. Another advantage of an interpolated flap is that it can be harvested in regions of redundant tissue, which may be at sites removed from the immediate area of the defect. That is, the base of the flap is not immediately juxtaposed to the defect as required by the use of transposition and rotation flaps.

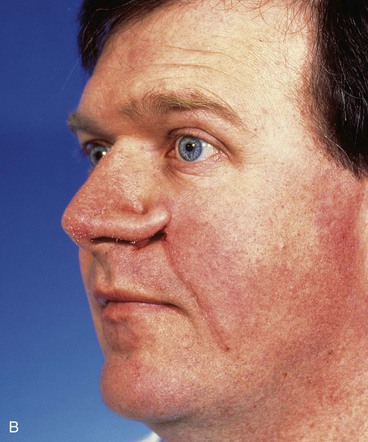


FIGURE 6-16 A, A 2 × 0.6-cm skin defect of alar rim after micrographic surgery for skin cancer. Internal lining provided by bipedicle vestibular skin advancement flap. Donor site of bipedicle flap closed with thin full-thickness skin graft. Structural support provided by auricular cartilage rim graft. B, Cutaneous pedicled interpolated cheek flap secured over auricular cartilage graft positioned along nostril margin. C, One week after second-stage division of pedicle and flap inset. D, Six months later. Critical alar facial sulcus preserved. No revision surgery performed. (From Fader DJ, Baker SR, Johnson TM: The staged cheek to nose interpolated flap for reconstruction of the nasal alar rim/lobule. J Am Acad Dermatol 37:614, 1997.)
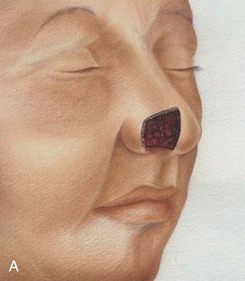
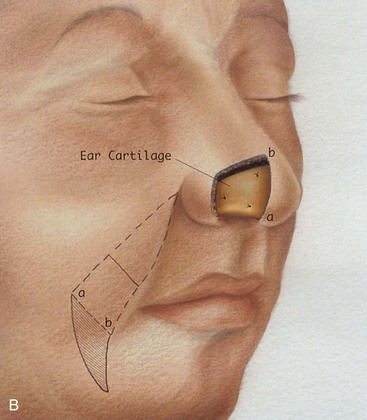
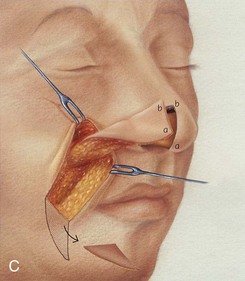
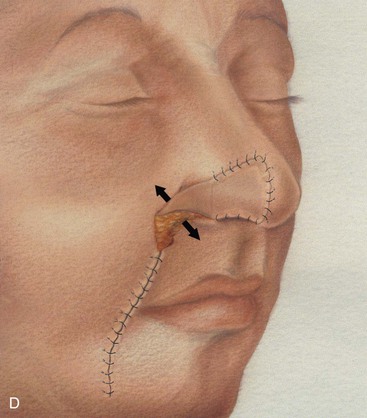
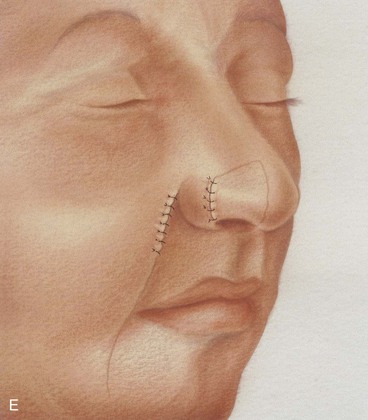
FIGURE 6-17 A, Cutaneous defect of anterior alar groove. B, Auricular cartilage graft in place for structural support. Subcutaneous tissue pedicle interpolated melolabial flap designed for repair of defect. C, Flap elevated on pedicle of fat. Standing cutaneous deformity forming at superior aspect of donor site transferred with flap to nose. Standing cutaneous deformity forming at inferior aspect of donor site excised and discarded. D, Flap transferred to recipient site. Pedicle crosses over alar facial sulcus. E, Three weeks later, pedicle divided and flap inset at nose.
Advancement Flaps
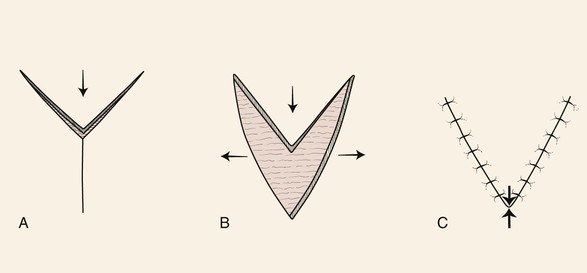
Advancement flaps have a linear configuration and are moved by sliding toward the defect. This involves stretching the skin of the flap (Fig. 6-18). Thus advancement flaps work best in areas of greater skin elasticity. The most basic advancement flap is the simple linear layered closure, which involves undermining and direct advancement of tissue side-to-side to close the defect primarily. This closure does not create a secondary defect, and additional incisions are made only for the removal of standing cutaneous deformities (Fig. 6-19). However, the term advancement flap usually refers to a flap created by incisions that allow a “sliding” movement of tissue. Tissue transfer is achieved by moving the flap and its pedicle in a single vector. The greatest wound closure tension is perpendicular to the distal border of the flap. Advancement flaps may be categorized as unipedicle, bipedicle, V-Y, Y-V, and island. Except for the V-Y and island flaps, all other advancement flaps form two standing cutaneous deformities, one on either side of the base of the flap. This is in sharp contrast to pivotal flaps, which form only one standing cutaneous deformity.
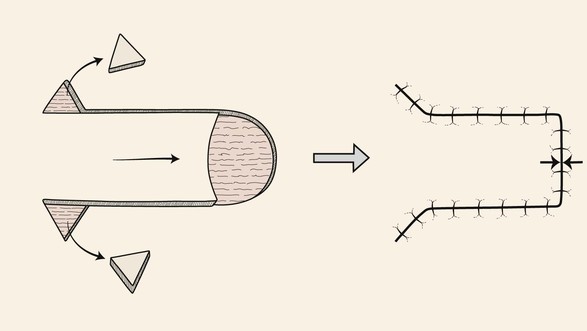
FIGURE 6-18 Advancement flaps have linear configuration and are moved by sliding toward defect. Greatest wound closure tension is perpendicular to distal border of flap (opposing arrows). Removal of the Burow triangles at base of flap equalizes wound border length and length of primary plus secondary defect.
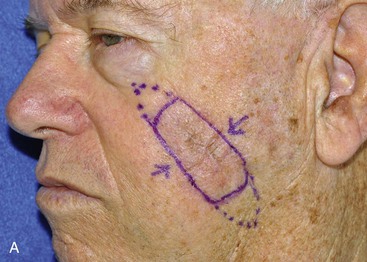


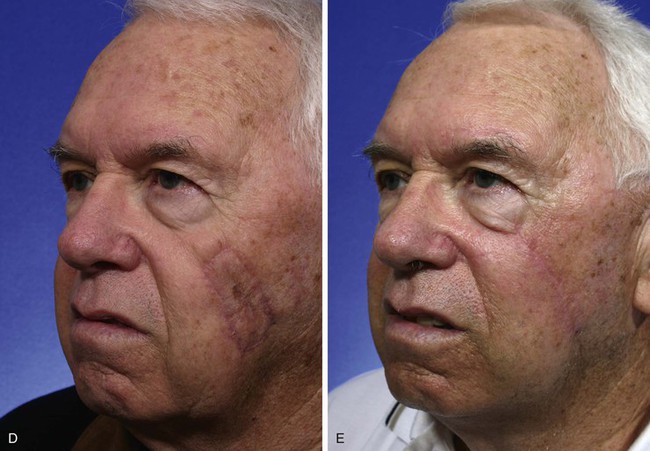

FIGURE 6-19 A-C, Cheek advancement flaps often take the form of primary wound closure with excision of standing cutaneous deformities (SCD). A, A 4 × 2-cm lentigo maligna of medial cheek marked for excision and repair by advancement of cheek skin. Anticipated standing cutaneous deformities marked for excision. B, Cutaneous lesion excised. C, Standing cutaneous deformities excised and wound closed. D-G, Preoperative and 2-month postoperative views. No revision surgery performed.
Unipedicle Advancement Flap
A unipedicle advancement flap is created by parallel incisions that allow a sliding movement of tissue in a single vector toward a defect. The movement is in one direction, and the flap advances directly over the defect. As a consequence, the flap must be developed adjacent to the defect, and one border of the defect becomes the leading border of the flap. Repair with an advancement flap involves both primary and secondary tissue movement (see Fig. 6-2). Complete undermining of the advancement flap as well as of the skin and soft tissue around the pedicle is important to enhance tissue movement. The two standing cutaneous deformities forming at the base of advancement flaps may require excision or may be eliminated by a halving suture technique. This involves dividing in half the length of the wound repair with each consecutive suture. This evenly distributes the redundant tissue of the standing cutaneous deformity as small puckers along the entire length of the wound. Thus the redundancy is “sewn out” without the need for excision of skin. Excision of standing cutaneous deformities (Burow triangles) may facilitate movement of the flap (Fig. 6-18). Unlike with the pivotal flap, in which the standing cutaneous deformity must be dealt with at the base of the flap, the deformities that develop from advancement can be excised anywhere along the length of the flap and not necessarily juxtaposed to the base. This is because of the mechanism of tissue movement. Excision of standing cutaneous deformities of advancement flaps is predicated on the most optimal site for excision. Typical excisions are placed in RSTLs or in borders between aesthetic regions of the face.
Unipedicle advancement flaps and rotation flaps have one characteristic that is inherent only in these two flap designs. Owing to their specific design and use, when either type of flap is transferred to its respective recipient site, it results in a situation in which there are unequal lengths to the borders of the wound. This is because the peripheral border of the wound (flap incision plus defect length) is longer than the length of the flap. Triangular skin excisions along the periphery of the wound (Burow triangle) in essence have the effect of reducing the length of the peripheral wound so that its length matches the length of the border of the flap. These excisions are referred to as equalizing triangles. In the case of rotation flaps, a single Burow triangle excision is required, whereas unipedicle advancement flaps require two excisions, one on either side of the flap. An alternative to the technique of Burow triangle excision is to invert the triangular excision and to close the skin defect by advancing the triangular flap created by the inverted excision (Fig. 6-20).11 This is referred to as an inverted Burow triangle excision. When it is used, the technique results in an irregular suture line. Although this technique results in a longer scar than in a standard Burow triangle excision, the irregular scar pattern may create a less conspicuous and less contracting scar.
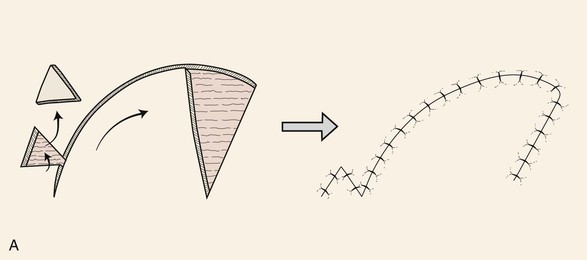
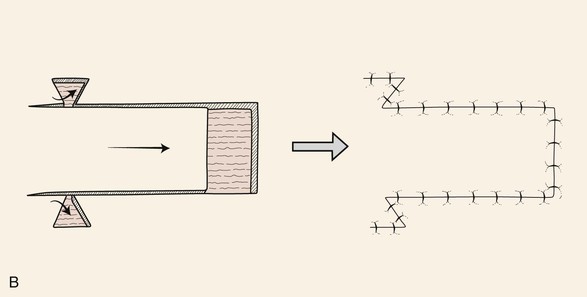
FIGURE 6-20 A, B, Alternative to technique of excising Burow triangles to adjust for unequal wound lengths is excision of inverted triangle of skin at peripheral margin of wound. An inverted Burow triangle excision can be used for unipedicle advancement and rotation flaps.
Bilateral unipedicle advancement flaps are commonly combined to close various defects, resulting in H- or T-shaped repairs, depending on the configuration of the defect. Repair in this manner is often referred to as an H-plasty or T-plasty (Fig. 6-21). In both cases, advancement flaps are designed on opposite sides of the defect and advance toward each other. Each flap is responsible for covering a portion of the defect. The resulting standing cutaneous deformities are often excised in the area of the defect or along the linear axes of the flaps. The two flaps do not necessarily have to be of the same length. Flap length is determined primarily by the elasticity and redundancy of tissue at the donor site.
V-Y and Y-V Advancement Flaps
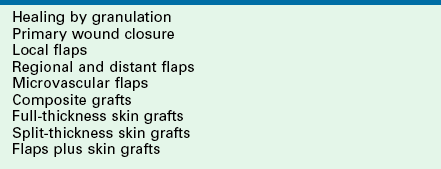
The V-Y advancement flap is unique in that the V-shaped flap is not stretched or pulled toward the recipient site but rather achieves its advancement by recoil or by being pushed forward. Thus the flap is allowed to move into the recipient site in a nearly tension-free fashion. The secondary triangular donor defect is then repaired with wound closure tension by advancing the two borders of the remaining wound toward each other. In so doing, the wound closure suture line assumes a Y configuration, with the common limb of the Y representing the suture line resulting from closure of the secondary defect (Fig. 6-22). The flap is optimally designed so that the common limb of the Y falls in the boundary of neighboring aesthetic regions or within a natural crease, fold, or wrinkle. V-Y advancement is particularly useful when a structure or region requires lengthening or release from a contracted state. For instance, V-Y advancement is helpful in releasing contracted scars that are distorting structures such as the vermilion or eyelids. The affected area of distorted vermilion or eyelid is incorporated into the V-shaped flap and advanced toward the lip or eye to restore natural topography. The skin borders adjacent to both sides of the secondary defect are then advanced toward each other and sutured. The suture line becomes the vertical or common limb of the Y configuration. The V-Y advancement flap may also be designed as an island flap based on a subcutaneous tissue pedicle. In this case, the flap is stretched toward the defect rather than allowed to recoil. This type of flap is discussed in detail in a later portion of this chapter.
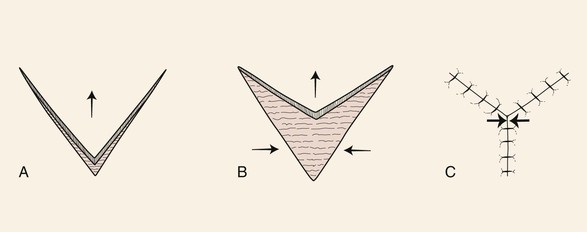
FIGURE 6-22 A, B, V-Y advancement flap: V-shaped flap not stretched or pulled toward defect. It achieves advancement by recoil or by being pushed forward. C, Wound closure suture line assumes Y configuration. Greatest wound closure tension is at closure site of donor defect (opposing arrows).
The Y-V advancement flap has a similar principle to the V-Y flap except that the V-shaped flap is stretched or pulled toward a linear incision made at the apex of the triangular flap (Fig. 6-23). The borders of this incision are allowed to spread apart, creating a tissue void. The flap is advanced into the void and sutured in place. The wound closure suture line assumes a V configuration. The maximum wound closure tension is at the apex of the flap. The Y-V advancement flap has fewer applications than the V-Y flap but may be used on some occasions to relocate, in a more natural position, a distorted facial structure. An example would be in correcting an oral commissure that has been displaced medially by scar. The commissure is incorporated into the triangular flap, and a horizontal incision is made lateral to the commissure. The flap consisting of the commissure is then advanced laterally into the tissue void created by the horizontal incision.
Bipedicle Advancement Flaps
Bipedicle advancement flaps are used primarily for repair of large defects of the scalp. The flap is designed adjacent to the defect and is advanced into the defect at a right angle to the linear axis of the flap. This leaves a secondary defect that usually must be repaired with a split-thickness skin graft. As a consequence, bipedicle flaps are rarely used for reconstruction of the face and neck. The exception to this is the use of bipedicle advancement flaps for relining limited full-thickness nasal defects of the hemi-tip or ala that have a vertical height of no more than 1.0 cm. The flap consists of vestibular skin and mucosa based medially on the septum and laterally on the floor of the nasal vestibule. An extended intercartilaginous incision is made, and the flap is elevated off the undersurface of the alar cartilage and mobilized inferiorly to reline the ala or hemi-tip. The donor site on the ventral aspect of the cartilage is covered with a thin full-thickness skin graft. The bipedicle flap is thin and provides natural physiologic material for the interior of the nasal passage with sufficient vascularity to support the concomitant use of free cartilage grafts placed over the lining flap for structural support of the construction.12
Hinge Flap
Hinge flaps are commonly used for repair of full-thickness nasal defects in which the remaining nasal skin adjacent to the defect is sufficient to develop a flap for internal nasal lining. Hinge flaps may also be used to close mature sinofacial and salivary fistulas anywhere in the aerodigestive tract. Hinge flaps consisting of subcutaneous tissue and sometimes muscle without overlying skin can be used to fill in contour deficits.13
Burget and Menick14 have studied the vascularity of septal mucosa and have shown that the entire ipsilateral mucoperichondrium can be transferred on a narrow pedicle containing the septal branch of the superior labial artery and hinged on the caudal aspect of the nasal septum. Such hinge flaps are designed to extend from the floor of the nose to within 1 cm of the junction of the upper lateral cartilage and cartilaginous septum. The flap may extend posteriorly well beyond the bony cartilaginous septum, producing a hinge mucosal flap measuring as much as 3 cm wide and 5 cm long. The flap is reflected laterally across the nasal passage to reline full-thickness alar defects with a vertical height of 1.5 cm or greater. Because the flap spans the nasal passage, it must be detached from the septum 3 weeks after initial transfer. In this respect, the caudal septal hinge flap assumes some of the properties of an interpolated flap, requiring subsequent inset. For full-thickness defects of the ala extending cephalically into the nasal sidewall, a single ipsilateral mucoperichondrium hinge flap is insufficient to reline the entire interior of the lateral nose. In such instances, a second hinge septal mucosal flap is harvested from the contralateral side based on the nasal dorsum. This flap is reflected laterally through a fenestrum in the septum to line the more cephalic portion of the nasal sidewall; the ipsilateral hinge mucosal flap is used to line the more caudal aspect of the defect.
Defect Analysis
In assessing a facial defect, the surgeon must determine the most appropriate method of reconstruction.3 Several issues enter the decision-making process. First, the closure must not conceal residual tumor, so the reconstructive surgeon must be comfortable with the fidelity of the extirpative method. Second, the risk of tumor recurrence must be assessed; the reconstructive method of choice may be altered by this consideration. Finally, given these factors, the surgeon should select the technique that will render the best possible aesthetic and functional result.
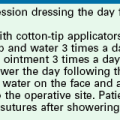
In assessing a given defect, the surgeon should evaluate its complexity in terms of missing tissue layers, topography, and aesthetic region/unit involvement. Surgical judgment is critical in the decision-making process. On initial consideration, the surgeon should evaluate the applicability of immediate versus delayed reconstruction.15 Options for cutaneous repair include healing by second intention (granulation); primary wound closure with or without M-plasty; skin graft; and local, regional, or distant flap repair (Table 6-2). Optimally, each layer of absent tissue should be replaced with like tissue. When possible, the cutaneous defect should be closed with skin of similar thickness, color, and texture as that of the missing skin. Missing cartilage should be replaced by appropriately positioned, contoured, and sculptured cartilage. Mucosa should generally be repaired with neighboring mucosal tissue.
Preferred Flaps
Scalp
Whenever possible, multiple rotation flaps are preferred to the use of a single flap for scalp reconstruction. Each flap is designed to pivot on an independent pivotal point. When two rotation flaps are used, the flaps may be designed to pivot in opposite directions, creating an O-T configuration of the wound repair, or in the same direction, as an O-Z repair16 (Fig. 6-24). Use of more than one rotation flap is advantageous because it recruits tissue for reconstruction from different locations on the scalp. Within limits, the greater the number of flaps used, the more diffuse is the tissue recruitment. Likewise, the burden of the repair of the secondary defect is shared by the number of donor sites of the flaps used. Two or three rotation flaps work best for reconstruction of most scalp defects. When three flaps are used, each flap is responsible for repairing one-third of the surface area of the defect. Wound closure is accomplished by pivoting all three flaps in the same direction. Repair of the defect has an appearance of a pinwheel, and wound closure configuration resembles the closing of a camera lens.16 When a single rotation flap is used, the parameter of the arc of the flap should be at least four times the diameter of the scalp defect. Sometimes one or two back cuts at the base of the flap are necessary to reduce wound closure tension. On rare occasions, the secondary defect must be skin grafted or left to heal by secondary intention. Standing cutaneous deformities at the base of scalp flaps are not resected at the time of flap transfer because resection has the effect of reducing the width of the base of the flap and may impair vascularity. In addition, deformities tend to flatten during a 4- to 6-week interval. Usually after 6 weeks, any remaining deformity may be removed safely because recipient site vascularity is sufficient to maintain flap viability.


FIGURE 6-24 O-Z plasty useful for repair of scalp defects. A, A 4 × 4-cm full-thickness vertex scalp defect. Rotation flaps designed to pivot in same (clockwise) direction. B, Wound repair assumes Z-shaped closure. (From Baker SR: Reconstructive surgery for skin cancer. In Friedman RJ, Dzubow LM, Rigel D, et al, editors: Cancer of the skin, Philadelphia, Elsevier-Saunders, 2005.)
Forehead
The most effective technique for reconstruction of the forehead usually involves one or more advancement flaps. In spite of the relative inelasticity of forehead skin, the use of advancement flaps versus pivotal flaps is preferred because they typically produce the best cosmetic results. This is because incisions necessary for advancement flaps may be placed in the horizontal creases of the forehead or along the border of the eyebrow, depending on the location of the defect. Transposition flaps do work well in the region of the temple, but more medially on the forehead. It becomes difficult to close the donor site when such flaps are used. Dividing the forehead into three zones (median, paramedian, lateral) assists in planning reconstruction. In spite of a wound closure scar that is perpendicular to the horizontal creases of the forehead, defects of the central third of the forehead may be repaired with a vertical orientation with a predictably good aesthetic result (Fig. 6-25). This is probably due to the natural dehiscence or attenuation of the frontalis muscle in this portion of the forehead. In contrast, defects located solely within the paramedian and lateral zones of the forehead are best repaired with wound closure oriented in a horizontal axis when possible. Advancement flaps should be designed with horizontal orientations because this design facilitates scar camouflage and minimizes the vertical component to the repair. Vertical scars in the paramedian and lateral zones of the forehead are perpendicular to forehead creases and their appearances are accentuated by contraction of the frontalis muscle.
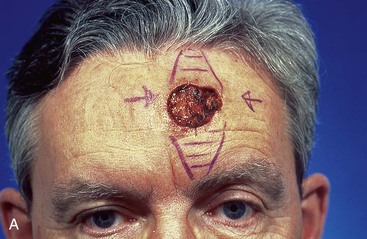

FIGURE 6-25 Skin defects of central forehead repaired with vertical orientation provide acceptable aesthetic results. A, A 3.5 × 3.0-cm skin defect of central forehead repaired by primary closure. Areas marked for excision (horizontal lines) represent anticipated standing cutaneous deformities. B, Postoperative view at 10 months. No revision surgery performed. (From Baker SR: Reconstructive surgery for skin cancer. In Friedman RJ, Dzubow LM, Rigel D, et al, editors: Cancer of the skin, Philadelphia, Elsevier-Saunders, 2005.)
Because of the inelasticity of forehead skin, bilateral advancement flaps are typically designed on opposite sides of the defect. This arrangement reduces the degree of tissue movement required compared with use of a single flap. Two opposing advancement flaps recruit tissue from two separate areas of the forehead, and this has the effect of reducing wound closure tension compared with the use of a single flap (Fig. 6-26). Except in the midline of the forehead, advancement flaps should be elevated in the subcutaneous plane to preserve the supraorbital and supratrochlear nerves. Defects in the midline are best closed without making horizontal incisions. Rather, they are treated like a primary wound closure, using advancement by dissecting in the subgaleal plane, because all sensory nerves are superficial to this plane of dissection. If the defect cannot be completely closed by primary apposition of wound margins, the remaining portion of the wound is left open to heal by second intention.



FIGURE 6-26 Bilateral advancement flaps preferred for repair of small (2 cm or less) skin defects of paramedian and lateral forehead. Except in midline, advancement flaps are elevated in subcutaneous tissue plane to preserve supraorbital and supratrochlear nerves. A, Margins of lentigo maligna outlined by sutures. B, Bilateral advancement flaps (H-plasty) designed. Shaded triangles represent Burow triangles, which were excised. C, Postoperative view at 5 months. No revision surgery performed. (From Baker SR: Reconstructive surgery for skin cancer. In Friedman RJ, Dzubow LM, Rigel D, et al, editors: Cancer of the skin, Philadelphia, Elsevier-Saunders, 2005.)
Medial Cheek
The surgeon has a number of options when repairing skin defects of the medial cheek. This is because of the elasticity of skin in this area and the relative abundance of redundant facial skin. The preferred method of flap repair is usually by a transposition or advancement flap. Advancement flaps may be designed with a cutaneous or subcutaneous tissue pedicle. When it is designed solely on a subcutaneous tissue pedicle, it is known as an island pedicle flap. Transposition flaps used for repair of medial cheek defects are best designed so that the donor site is in the vicinity of the jowl (Fig. 6-27). The jowl is the area of greatest facial skin redundancy. In older patients, this redundancy can provide a source for a large flap and still enable primary closure of the donor site. Flaps are usually superiorly based, and whenever possible, the closure of the donor site should be designed to lie in the melolabial and labial mandibular creases. The standing cutaneous deformity is removed just lateral to the superior border of the defect.






FIGURE 6-27 Transposition flaps used to repair medial cheek defects are best designed so donor site is in vicinity of jowl. A, B, Preoperative views of melanoma in situ. Margins were cleared by assessing histology of strips of skin surrounding melanoma. C, Incised transposition flap designed to recruit skin from region of jowl. D, Wound closure. Standing cutaneous deformity removed from superolateral aspect of defect. E, F, Postoperative views at 6 months. No revision surgery performed. (From Baker SR: Reconstructive surgery for skin cancer. In Friedman RJ, Dzubow LM, Rigel D, et al, editors: Cancer of the skin, Philadelphia, Elsevier-Saunders, 2005.)
The V-Y subcutaneous tissue pedicle island advancement flap is an option for repair of medial cheek skin defects at or below the level of the nasal alae.17 The flap is particularly well suited for skin defects located immediately adjacent to the alae (Fig. 6-28). A triangle-shaped skin island is designed with the base of the triangle formed by the inferior margin of the defect. Optimally, the vector of flap advancement is designed to parallel the melolabial crease. The width of the skin island should equal the width of the defect at its widest point. The length of the skin island should generally be twice the length of the defect. The trailing half of the skin island tapers to a point to facilitate donor site closure in a V-Y fashion after flap advancement. The skin island may extend as far as the inferior border of the mandible if necessary (Fig. 6-29). Positioning the inferior tip of the skin island directly in the melolabial crease optimally conceals the donor site scar. Insofar as possible, incisions should be designed so their scars are parallel to or in borders of aesthetic regions.


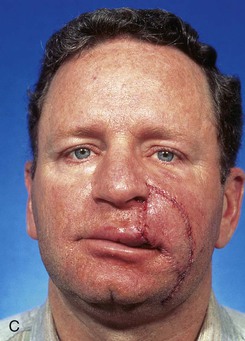



FIGURE 6-28 V-Y subcutaneous tissue pedicle island advancement flap useful for repair of cheek defects adjacent to ala. A, B, A 4 × 3.5-cm skin defect of lip and cheek. V-Y subcutaneous tissue pedicle island advancement flap designed for repair. Remaining skin of lateral upper lip marked for excision. C, D, Flap in place. E, F, Postoperative views at 2 years, 8 months. Contouring of flap performed 9 months after surgery. (From Baker SR: Reconstructive surgery for skin cancer. In Friedman RJ, Dzubow LM, Rigel D, et al, editors: Cancer of the skin, Philadelphia, Elsevier-Saunders, 2005.)

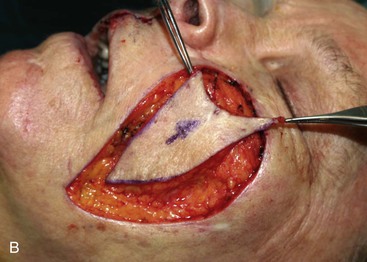
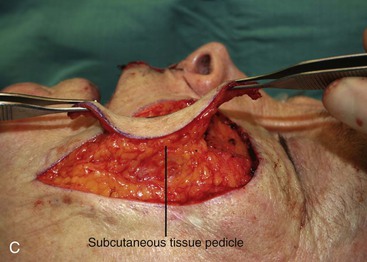




FIGURE 6-29 Multiple flap designs may be used for concurrent facial cutaneous defects. A, A 3 × 3-cm cutaneous defect of medial cheek. V-Y subcutaneous tissue pedicle island advancement flap designed for repair. B, C, Flap elevated on fat pedicle attached to central portion of flap. D, Flap in place. E-H, Preoperative and 5-month postoperative views. No revision surgery performed. I, Postoperative view at 5 months. Cutaneous lip defect converted to full-thickness lip wedge excision closed primarily. No revision surgery performed.
Cutaneous pedicled advancement flaps are less useful compared with island advancement flaps and transposition flaps in repair of medial cheek defects. When tissue advancement is used for repair of the medial cheek, it often takes the form of primary wound closure. Standing cutaneous deformities are removed in aesthetic borders when possible (see Fig. 6-19). If incisions are necessary to create a flap, they are designed so that they are placed in the natural lines of the face. Two parallel or slightly divergent incisions are made adjacent to the defect, and the flap is elevated in the subcutaneous plane and advanced over the defect. If the flap does not stretch sufficiently, it may be necessary to excise the Burow triangles on either side of the flap’s base. These triangular excisions help equalize the distance between the sides of the flap and the margins of the primary and secondary defect.
Lateral Cheek
Lateral cheek skin has less subcutaneous fat and is more adherent to the underlying fascia than is medial cheek skin. For this reason, subcutaneous tissue pedicle island advancement flaps work less well here because such flaps depend on ample subcutaneous tissue for movement. The preferred flap for smaller defects of the lateral cheek is the transposition flap. Larger defects are best repaired with rotation advancement flaps designed to recruit upper cervical skin into the flap (Fig. 6-30). Transposition flaps are usually superiorly based, and the skin immediately above the angle of the mandible serves as the donor tissue for the flap. This is because skin of the lateral inferior cheek is more redundant and mobile compared with skin in the lateral superior cheek near the temple. The increased mobility is attributed to the presence of the platysmal muscle covering the mandible.
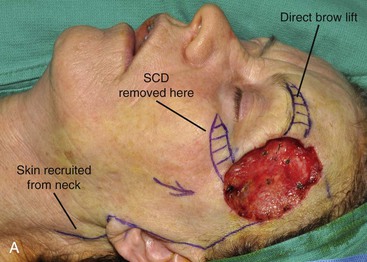


FIGURE 6-30 A, A 5 × 7-cm skin and soft tissue defect of temple. Temporal branch of facial nerve resected. Cervical-facial rotation advancement flap designed to recruit upper cervical skin for purpose of repair. Direct brow lift marked to treat brow ptosis resulting from paralysis. SCD, standing cutaneous deformity. B, Wound closed. C, Postoperative view at 6 months. No revision surgery performed.
Central Lip
Depending on the laxity of the lips, cutaneous defects approaching half the width of the lip may be converted to full-thickness excisions of the lip followed by primary wound closure (see Fig. 6-29). The majority of skin defects of the central upper and lower lips that cannot be closed primarily can be repaired most favorably with bilateral advancement flaps. For the upper lip, incisions for opposing advancement flaps are made along the vermilion-cutaneous border and immediately below the nasal sill (Fig. 6-31). For the lower lip, incisions are placed in the vermilion-cutaneous border and the mental crease. Although the skin of the lips is elastic, it is tightly adherent to the underlying muscle and must be dissected sharply from the orbicularis oris as there is little subcutaneous fat present. It is usually necessary to remove a Burow triangle from the vermilion to prevent excessive bunching when the opposing borders of the two advancement flaps are approximated.




FIGURE 6-31 Cutaneous defects of central upper and lower lips that cannot be closed primarily may be repaired most favorably with bilateral advancement flaps. A, A 3 × 2.5-cm skin defect. B, Bilateral advancement flaps designed with incisions in vermilion-cutaneous border and adjacent to nasal sill. Bilateral Burow triangles marked in alar facial sulcus. C, Wound closed. Single standing cutaneous deformity removed from vermilion inferiorly and bilateral deformities removed from alar facial sulcus superiorly. D, Postoperative view at 8 months. No revision surgery performed. (From Baker SR: Reconstructive surgery for skin cancer. In Friedman RJ, Dzubow LM, Rigel D, et al, editors: Cancer of the skin, Philadelphia, Elsevier-Saunders, 2005.)
Lateral Lip
Cutaneous defects of the lateral aspect of the upper and lower lips that cannot be repaired primarily are best repaired with rotation flaps or subcutaneous tissue pedicle island advancement flaps (Fig. 6-32). Skin is recruited from the adjacent perioral area. In general, flaps from the medial cheek should not be used because by necessity they traverse the melolabial crease and obliterate this important aesthetic boundary. Rotation flaps should be designed so that the incision for the flap lies in or parallel to the melolabial crease. The skin flap is elevated from the orbicularis oris and is based on the ample subcutaneous fat located immediately lateral to the commissure. In the case of upper lip defects, a back cut below the level of the commissure may be necessary to facilitate sufficient tissue movement. A standing cutaneous deformity develops as the flap pivots and should be excised along the vermilion border to prevent the flap from distorting the vermilion.
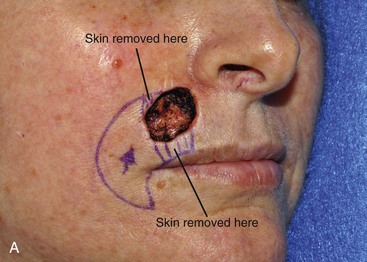



FIGURE 6-32 Cutaneous defects of lateral upper lip may be repaired with V-Y subcutaneous tissue pedicle island advancement flaps. A, A 3 × 2.5-cm skin defect of lateral upper lip. V-Y subcutaneous tissue pedicle island advancement flap designed for repair. Skin of lip marked for removal to place scar at vermilion-cutaneous border. B, Incised flap recruits skin from perioral area. Flap advanced and wound closed. C, D, Postoperative views at 5 months. No revision surgery performed.
Subcutaneous tissue pedicle island advancement flaps are ideally suited for repair of lateral skin defects of the upper lip. They do not work as well for defects of the lower lip. As discussed earlier, this flap design is also ideal for medial cheek defects adjacent to the nasal alae. The flap is dissected in a fashion similar to the method discussed for its use in repair of medial cheek defects, except that the flap is freed from its orbicularis muscle attachments near the commissure and is based solely on the abundant subcutaneous fat located just lateral to the commissure.
Nose
The two most commonly used local flaps for repair of cutaneous defects of the nose and in which the donor site of the flaps is confined to the nose are the subcutaneous tissue pedicle island advancement flap and the bilobe flap.18 The island flap is used for repair of defects located at the anterior aspect of the alar groove. The bilobe flap is used to repair small cutaneous defects of the nasal tip, caudal dorsum, or caudal sidewall.
Small defects (1.5 cm or less in size) in the region of the anterior alar groove between the ala and tip can be effectively repaired with a subcutaneous tissue pedicle island advancement flap (Fig. 6-33). It is based on subcutaneous tissue and portions of the transverse nasalis muscle. A triangle-shaped flap with its base making up the cephalic border of the defect is designed with the apex of the flap positioned laterally. The posterior border of the flap rests in the alar groove. The anterior border extends cephalically and slightly medially from the defect and is designed to recruit skin of the nasal sidewall. The anterior border then arcs laterally to meet the posterior border in the alar facial sulcus. The flap is incised to the level of the perichondrium of the nasal cartilages. The adjacent nasal skin is undermined widely, and the proximal and distal thirds of the flap are undermined in the subcutaneous plane. The central third of the flap remains pedicled on the subcutaneous tissue. The flap is undermined only to the degree that there is sufficient mobility to allow the flap to be advanced into the recipient site. The flap is advanced and secured at the recipient site first, and then the donor site is closed, creating a V-Y configuration to the repair.


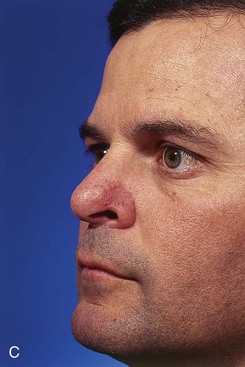
FIGURE 6-33 Skin defects smaller than 1 cm and located at anterior alar groove between ala and tip may be repaired with subcutaneous tissue pedicle island advancement flap. A, Flap designed adjacent to skin defect. B, Flap advanced. C, Postoperative view at 2 months. No revision surgery performed.
Bilobe nasal flaps are the preferred flap to repair 1- to 1.5-cm cutaneous defects of the central tip or caudal dorsum (Fig. 6-34).18 They may also be used to repair skin defects of the lateral nasal tip. However, when the defect encroaches on the nostril margin, there is a greater likelihood of elevation of the nostril as the wound heals. A distance equal to the radius of the defect is measured from the lateral border of the defect to the pivotal point of the two lobes of the bilobe flap. Two arcs are drawn with their centers at the pivotal point. One arc passes through the center of and the other tangential to the distal border of the defect. The base of both lobes of the flap arises from the first arc. The height of the first lobe extends to the second arc. The height of the second lobe is twice the height of the first lobe and tapers to a point. The width of the first lobe equals the width of the defect. The width of the second lobe may be 25% less than the first lobe. The axis of the defect and the two lobes of the flap are approximately 45° apart for a total of 90° to 110°. The donor site of the second lobe is closed first. The first lobe is transposed and the standing cutaneous deformity removed. The second lobe is then transposed and trimmed to fit precisely without wound closure tension.
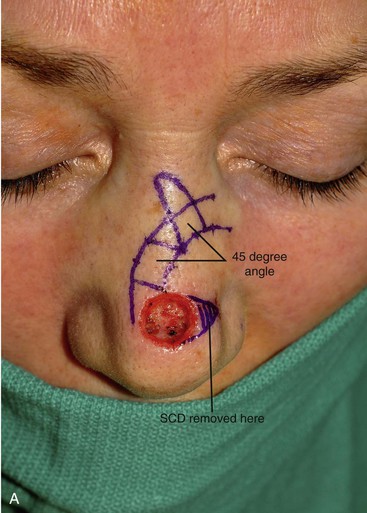




FIGURE 6-34 Bilobe nasal flaps work best for repair of skin defects of central nasal tip. A, A 1 × 1-cm skin defect of nasal tip. Bilobe nasal flap designed for repair. Axes of lobes oriented 45° from each other. SCD, standing cutaneous deformity. B, Wide undermining in subfascial tissue plane required. C, Flap in place. D-G, Preoperative and 4-month postoperative views. Flap dermabraded 2 months after surgery.
Eyelid
Requirements for eyelid repair are dependent on whether the defect is partial or full thickness. Full-thickness defects ideally require a mucous membrane for internal lining and for lubrication of the ocular surface. Skeletal support that provides adequate lid rigidity and contour yet is sufficiently malleable to conform to the surface of the globe is also required. A rigid eyelid margin is necessary to keep eyelashes and skin away from the cornea. Adequate muscle is necessary to provide for closure of the eyelids. The external surface of the eyelids should be surfaced with thin skin sufficiently supple to allow eyelid excursion. Many small superficial eyelid defects can be repaired by primary wound closure or by thin full-thickness skin grafts. Larger cutaneous defects of the eyelid are usually repaired with rotation advancement flaps recruiting skin from the adjacent upper cheek. It is generally preferred to advance skin toward the eyelid from the lateral cheek rather than from the medial cheek because scar contracture from the use of medial cheek flaps tends to pull downward on the eyelid, causing ectropion. Another common flap design used for lower eyelid defects is a transposition flap in which skin from the opposing upper eyelid is transferred to the lower eyelid defect. These transposition flaps are usually based near the lateral canthus, and the upper eyelid donor site for the flap is closed primarily.
References
1. Larrabee, WF, Jr. Design of local skin flaps. Otolaryngol Clin North Am. 1990; 23:899.
2. Burget, GC, Menick, FJ. Subunit principle in nasal reconstruction. Plast Reconstr Surg. 1985; 76:239.
3. Clevens, RA, Baker, SR. Defect analysis and options for reconstruction. Otolaryngol Clin North Am. 1997; 30:495.
4. Baker, SR. Reconstruction of facial defects. In: Cummings CW, Fredrickson JM, Harker LA, et al, eds. Otolaryngology—head and neck surgery. 3rd ed. Philadelphia: Mosby; 1998:527–559.
5. Baker, SR. Local cutaneous flaps in soft tissue augmentation and reconstruction in the head and neck. Otolaryngol Clin North Am. 1994; 27:139.
6. Gorney, M. Tissue dynamics and surgical geometry. In: Kernakan DA, Vistnes LM, eds. Biological aspects of reconstructive surgery. Boston: Little, Brown, 1977.
7. Bray, DA. Rhombic flaps. In: Baker SR, Swanson NA, eds. Local flaps in facial reconstruction. St. Louis: Mosby; 1995:151–163.
8. Zitelli, JA. Bilobe flaps. In: Baker SR, Swanson NA, eds. Local flaps in facial reconstruction. St. Louis: Mosby; 1995:165–180.
9. Baker, SR, Alford, EL. Mid-forehead flaps. Oper Tech Otolaryngol Head Neck Surg. 1993; 4:24.
10. Menick, FJ. Aesthetic refinements in use of the forehead flap for nasal reconstruction: the paramedian forehead flap. Clin Plast Surg. 1990; 17:607.
11. Suzuki, S, Matsuda, K, Nishimura, Y. Proposal for a new comprehensive classification of V-Y plasty and its analogues: the pros and cons of inverted versus ordinary Burow’s triangle excision. Plast Reconstr Surg. 1996; 98:1016.
12. Baker, SR. Internal lining flaps. In: Baker SR, ed. Principles of nasal reconstruction. 2nd ed. New York: Springer; 2011:29–46.
13. Johnson, TM, Baker, SR, Brown, MD, et al. Utility of the subcutaneous hinge flap in nasal reconstruction. J Am Acad Dermatol. 1994; 30:459.
14. Burget, GC, Menick, FJ. Nasal support and lining: the marriage of beauty and blood supply. Plast Reconstr Surg. 1989; 84:189.
15. Thomas, JR, Frost, TW. Immediate versus delayed repair of skin defects following resection of carcinoma. Otolaryngol Clin North Am. 1993; 26:203.
16. Baker, SR. Options for reconstruction in head and neck surgery. In: Cummings CW, Fredrickson JM, eds. Otolaryngology—head and neck surgery, Update 1. St. Louis: Mosby; 1989:192–248.
17. Rustad, TJ, Hartshorn, DO, Cleven, RA, et al. The subcutaneous pedicle flap in melolabial reconstruction. Arch Otolaryngol Head Neck Surg. 1998; 124:1163.
18. Baker, SR. Nasal cutaneous flaps. In: Baker SR, ed. Principles of nasal reconstruction. 2nd ed. New York: Springer; 2011:163–209.