CHAPTER 74 Fixed Sagittal Imbalance
Fixed sagittal imbalance is a condition that occurs as a result of the loss of the normal lumbar lordosis or an increase in thoracic kyphosis, or both, resulting in the forward displacement of the head relative to the sacrum and pelvis. This “pitched forward” posture can lead to a number of debilitating consequences including difficulties with forward gaze, compensatory hip and knee flexion contractures, and loss of physiologic endurance as a result of increased energy expenditure.1 A number of etiologies of fixed sagittal imbalance are discussed in this chapter. The treatment of symptomatic sagittal imbalance is potentially complex, requiring correction, often with one or more osteotomies, and spinal instrumentation and arthrodesis.
Sagittal Alignment
An understanding of normal sagittal parameters is helpful in assessing patients with sagittal imbalance. Numerous authors have reported on ranges of sagittal alignment in asymptomatic volunteers. Bernhart and Bridwell2 studied 102 asymptomatic adolescent volunteers and described wide ranges of thoracic kyphosis (9 to 53 degrees, SD ± 10 degrees) and lumbar lordosis (−14 to −69 degrees, SD ± 12 degrees). The average age of patients in this study was 12.8 years. Stagnara and colleagues3 reported similar measurements in a group of 100 French volunteers aged 20 to 29 years. One hundred asymptomatic subjects and 100 patients with mechanical low back pain of slightly older age (mean age 39 years) were compared by Jackson and McManus.4 The differences were statistically significant as a result of the large study size; the absolute numbers were similar. The total lordosis averaged 60.9 degrees in the asymptomatic group versus 56.3 degrees in the symptomatic group. The authors reported that patients who were symptomatic were able to compensate for distal lumbar hypolordosis with exaggerated lordosis in the proximal lumbar spine. In general, all studies noted that approximately two thirds of the total lumbar lordosis is attained distally between L4 and the sacrum.
Standing sagittal alignment is typically measured from the middle of the C7 vertebral body on a 36-inch-long cassette radiograph. The spine is considered to be in neutral sagittal alignment when a gravity plumb line extending from the center of the C7 vertebral body bisects the S1 endplate. When the C7 plumb line passes anteriorly to the sacrum, the sagittal balance is considered positive; sagittal balance is negative when the C7 plumb line falls posteriorly to the sacrum.5 Recent studies have demonstrated that the C7 plumb line migrates more anteriorly with advancing age.6 This is due in large part to the loss of lumbar lordosis that occurs with disc degeneration.7 Pelvic parameters such as pelvic tilt and pelvic incidence and the relationship between the gravity line and heel position are additional methods to further the understanding of sagittal alignment and relationships with age.8,9
Etiology
Sagittal imbalance can have a variety of causes. One of the most common causes is the prior placement of Harrington distraction instrumentation for the treatment of scoliosis.10–12 A typical example would be a patient with a double major curve type pattern treated in the 1970s or 1980s with Harrington instrumentation extending from T4 to L3 or L4. If the spine was fused in proximal lumbar hypolordosis, maintenance of normal overall lumbar lordosis was often achieved with increased lordosis of the remaining normal discs—L3-4, L4-5, and L5-S1. If, over time, these discs degenerate, the patient will develop the progressive inability to compensate for the prior hypolordotic fusion and will develop sagittal imbalance. Moe and Denis13 have demonstrated the loss of lumbar lordosis after these procedures that results in the forward tilting of the spine. Patients who underwent these procedures 20 to 40 years ago are now becoming symptomatic.14
A second common scenario is termed degenerative sagittal imbalance.15 In this case, an adult patient has had numerous lumbar spinal fusion procedures, each with subsequent loss of lower lumbar lordosis. The incremental segmental changes gradually result in the patient’s inability to stand erect.
Another scenario involves the post-traumatic patient. An injury, typically a fracture at or around the thoracolumbar junction that heals in kyphosis, may present with a sharp, angular deformity.16 These deformities may be the sequelae of either operatively or nonoperatively treated unstable injuries. The patient typically complains of pain around the kyphos, as well as cephalad or caudad to the apex of the deformity. Compensation for the angular kyphotic deformity occurs at the suprajacent and subjacent disc spaces. With time, the discs can degenerate and lead to worsening of the deformity and increasing pain.
A fourth condition is the patient with ankylosing spondylitis. These patients will present with a lumbar hypolordosis and thoracolumbar kyphosis or cervicothoracic kyphosis.17 Patients with ankylosing spondylitis often have a stiff deformity and, as a result, are unable to compensate for it, leading to difficulties with forward gaze and mobility. Osteotomies in the lumbar spine or at the cervicothoracic junction are often necessary to correct the deformity.18,19
Patient Evaluation
History
Another essential aspect of the patient evaluation includes medical comorbidities, specifically diabetes, cardiac disease, and osteoporosis. Dual-energy x-ray absorptiometry (DEXA) is helpful in identifying patients with osteopenia and osteoporosis. These patients may benefit from preoperative pharmacologic treatment to improve bone mineral density. Patients who smoke are at significant risk of developing pseudarthrosis if spinal fusion is considered and may reasonably be required to cease smoking before surgery.20 All of these elements contribute to a thorough evaluation of the history of a patient with sagittal imbalance.
Physical Examination
The second aspect of the patient evaluation is the physical examination. Particular attention is paid to standing balance and gait. The overall postural balance in the coronal and sagittal planes and the pattern of gait should be examined. A patient with sagittal imbalance may often appear to have normal balance, only for the examiner to find that he or she is compensating with knee flexion. The apparent hip flexion is also often seen—in fact, femoral angulation relative to the vertical axis due to continued pelvic retroversion despite maximal hip extension. Lagrone and colleagues21 reported that almost 95% of patients with sagittal imbalance are unable to stand erect; nearly 90% had back pain with prolonged activity, and 27% had to flex their knees to stand erect. It is important to examine patients standing normally and with legs as straight as possible at the knee. The abdomen and back should be examined specifically for prior surgical incisions and postural creases and for a rotational deformity indicating a coronal spinal deformity. Examination of the patient in the supine and prone positions also helps to determine the flexibility of any spinal deformity, as evidenced by whether or not the kyphosis corrects with recumbent positioning. The supine position also eliminates the contributions of hip and knee flexion contractures to sagittal imbalance. Finally, a thorough neurologic examination is critical in all patients, but especially those who report deficits after prior surgery or whom upon history have suggestion of possible spinal cord level stenosis.
Radiographic Evaluation
Once the history and physical are complete, an assessment of the radiographic imaging is the next step in evaluation. Standing long cassette radiographs (14″ × 36″) are taken to include the entire spine from the base of the occiput to the distal sacrum and the femoral heads. The global spinal sagittal balance is determined using the C7 plumb line dropped vertically from the center of the body of C7. This may also be referred to as the sagittal vertical axis (SVA). The Scoliosis Research Society defines positive sagittal balance as the SVA passing anterior to the L5-S1 disc on the standing long cassette film. In general, any deviation of the SVA greater than 5 cm anterior to the normal position of the C7 plumb line is considered positive sagittal imbalance.14 Significant positive sagittal imbalance is defined as the C7 sagittal plumb line falling anterior to the femoral heads.
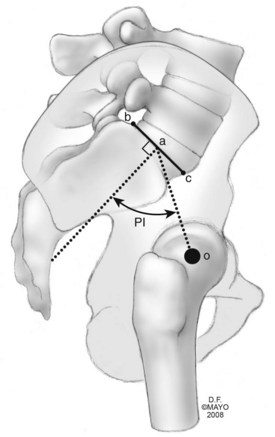
Other parameters that assist in the radiographic evaluation of these patients include measurements of the regional thoracic kyphosis (Cobb angle measured from T5-T12 on the lateral radiograph), lumbar lordosis (sagittal Cobb angle measured from the inferior endplate of T12 to the superior endplate of S1), thoracolumbar alignment (sagittal Cobb angle from T10-L2), and the pelvic incidence. The pelvic incidence assesses the relationship of the distal lumbar spine and sacrum to the pelvis and hip joints. The measurement is defined by the angle between the perpendicular to the sacral endplate and its midpoint and the line connecting this L point to the midpoint of a line connecting the femoral heads (Fig. 74–1).22,23
In addition to the long cassette standing radiographs, the authors routinely obtain focused studies of the lumbar and/or thoracic region. This helps in better defining local anatomy in a “coned-down” manner. Other useful studies include recumbent long cassette radiographs, either supine or prone. These radiographs help to elucidate the degree of flexibility within a deformity. The prone lateral view is similar to, but not exactly like, what the patient’s spine may look like on the operating table. Another useful radiograph is the supine hyperextension lateral, in which a bolster is placed under the apex of a kyphosis and, after some relaxation, a radiograph is taken to determine flexibility.24
Surgical Decision Making
For those patients with debilitating symptoms due to significant sagittal imbalance, surgical management generally involves spinal instrumentation and fusion in combination with an osteotomy or osteotomies to allow the surgeon to restore a more normal spinal alignment. The types of osteotomies include the Smith-Petersen osteotomy (SPO), the pedicle subtraction osteotomy (PSO), and the vertebral column resection (VCR).25,26 The key criterion for determining the necessity of an osteotomy is a partially or completely fixed deformity based on the physical examination and radiographic evaluation.27 Spinal malalignment that corrects entirely with prone positioning (seen on the recumbent lateral radiograph) is flexible; in this case, osteotomies for spinal realignment are unnecessary.
Sagittal imbalance may be divided into two types, I and II.25 Type I refers to a patient with a segmental problem, usually hyperkyphosis or limited lordosis. The segments above and below the problem can compensate for the local deformity, though, thus maintaining normal global sagittal spinal alignment. One example of a type I sagittal deformity is a patient with a post-traumatic kyphosis at the thoracolumbar junction with hyperlordosis of lumbar spine. Another example is a patient with Scheuermann kyphosis. Although the magnitude of the thoracic or thoracolumbar kyphosis can vary, and may be more than 100 degrees, the C7 plumb line remains normal.
Smith-Petersen Osteotomy
The original description of the SPO was given by Smith-Petersen and colleagues28 in 1945. It was described as a posterior wedge resection of the spine through the region of the facet joints in patients with ankylosing spondylitis with a subsequent controlled fracture of the ossified anterior longitudinal ligament. The ideal candidate for an SPO has a long, rounded kyphosis over multiple segments (e.g., a patient with Scheuermann kyphosis). The resection typically achieves about 10 degrees of correction per level, roughly correlating to one degree of lordosis for each millimeter of bone resection.29 The osteotomy requires removal of the interspinous ligaments, the ligamentum flavum, and the superior and inferior articular processes bilaterally. One of the requirements for an SPO is a mobile disc anteriorly because this osteotomy involves resection of posterior elements only, followed by compression posteriorly (Fig. 74–2). Compression of the remaining posterior elements can be achieved through gravity from appropriate intraoperative positioning, hinging of the operating table, or gentle compression against pedicle screw fixation, although the latter is not advisable in osteoporotic patients.30
Pedicle Subtraction Osteotomy
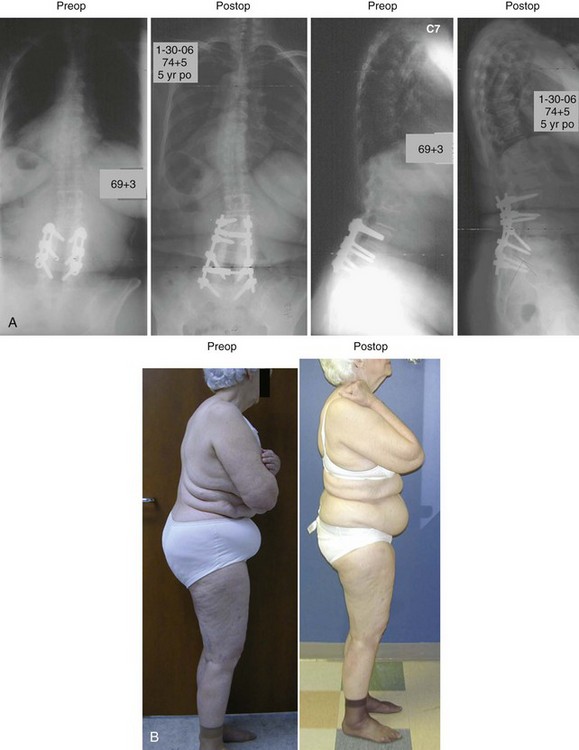
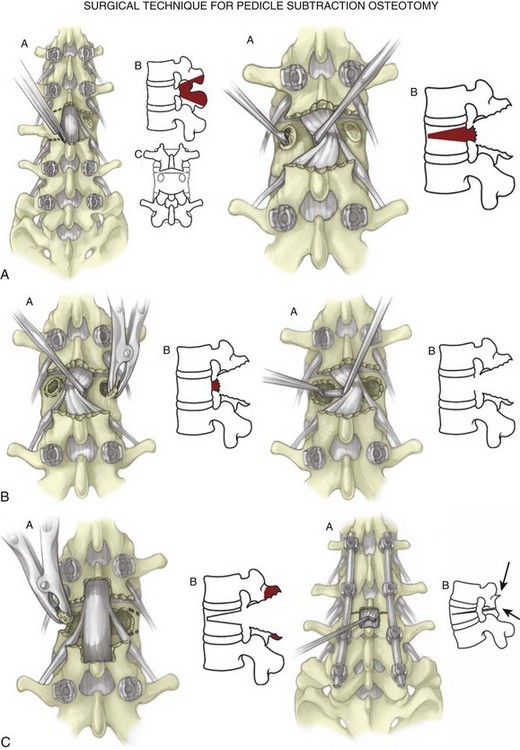
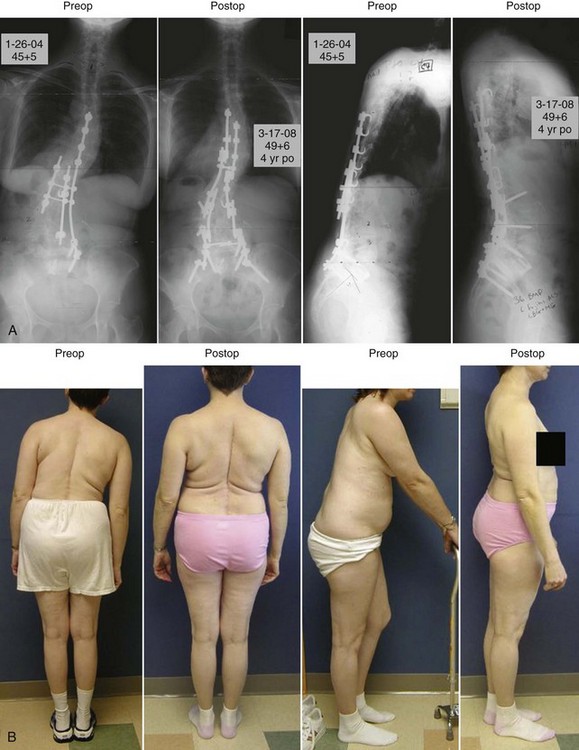
The pedicle subtraction osteotomy is the “workhorse” procedure for correcting fixed sagittal imbalance. It allows for a three-column correction of the spine through an entirely posterior approach. More importantly, it does so without lengthening the spinal column.15 It is completed entirely through one vertebral body, typically in the lumbar spine (Figs. 74-3 and 74-4).
The procedure proceeds in the following manner16:
The authors recommend widely opening the canal centrally at the osteotomy site to be able to inspect the dura for buckling and to probe the neural foramina with a Woodson elevator to ensure the absence of any neural compression. If a fusion construct is extended distally to the sacrum, as would be the case for a PSO at L3 or below, the authors recommend the addition of iliac screws to protect against S1 pedicle screw pullout or failure.31,32
A variation of the PSO that approaches the next osteotomy to be discussed is the asymmetric PSO. This can be performed to address sagittal imbalance with a coexistent coronal deformity. More bone along the lateral wall of the vertebral body is resected on the side of the convexity compared with the amount of bone resected along the concavity. This often involves removing the disc above and below the body along the convexity of the deformity. This allows not only for restoration of sagittal alignment but also for translation, which helps to restore coronal alignment (Fig. 74–6).
Outcomes following this procedure have not been reported extensively. A recent study is one of the first to report 5- to 8-year outcomes in patients undergoing PSO. Kim and colleagues33 reported on 35 consecutive patients undergoing PSO for sagittal imbalance, a follow-up from the initial 2-year study. Scoliosis Research Society outcomes remained similar in all domains at 5 years including very good patient satisfaction (87%), good self-image (76%), good function (69%), and fair pain subscales (66%) at latest follow-up.
Vertebral Column Resection
A vertebral column resection (VCR) is reserved for patients with fixed coronal and sagittal imbalance or complex severe deformities in the thoracolumbar spine.34 It is a complex osteotomy that includes resection of the entire vertebral body and the intervertebral discs above and below. Deformities that may be appropriate for VCR include a sharp, angular kyphosis in the thoracic spine or a severe thoracic or thoracolumbar kyphoscoliosis. A hemivertebrectomy is a form of vertebral column resection, as the hemivertebra is resected with the discs above and below.35 It is a powerful technique in deformity correction. Once completed, the spinal column can be shortened and the combined sagittal and coronal deformity corrected via a combination of translation and compression. An anterior structural cage is often necessary to bridge the defect left by resection of the vertebral body. Because this procedure circumferentially disconnects the spinal column, obtaining a fusion at this level is paramount.
The procedure involves resection of the posterior elements of the spine at the apex of the deformity. The laminae and facets proximal and distal to the level of the VCR are resected. In the thoracic spine, a costotransversectomy is necessary.25 Disarticulation of the rib head affords access to the lateral vertebral body. Once the rib is removed, a temporary rod is placed opposite the working side to stabilize the spine and protect the neural elements. Sacrifice of exiting nerve roots in the thoracic spine is tolerated and makes exposure much easier for working entirely via the posterior approach. In the lumbar region, the nerve roots cannot be sacrificed and thus VCR may require separate anterior and posterior approaches. If possible, a malleable retractor is placed lateral to the vertebral body in the subperiosteal plane. The pedicle, vertebral body, and discs are then removed in piecemeal fashion. Osteotomy closure is accomplished slowly and steadily using two temporary rods.36 It is usually necessary to place an anterior structural cage within the defect before complete closure in order to avoid shortening the spine excessively.
Complications
The surgical treatment of sagittal imbalance can result in significant complications. Osteotomies to restore sagittal alignment may be associated with significant intraoperative blood loss, lengthy operative times, and neurologic deficits. A decision is often made to stage such lengthy procedures. Suk and colleagues36 reviewed 70 patients undergoing VCR for severe spinal deformities. The average intraoperative blood loss was 2333 mL. In this same series, two patients had complete spinal cord injuries, although neither patient was neurologically intact before surgery. Neither patient had evidence of compressive lesion on re-exploration. Buchowski and colleagues37 reported on a consecutive series of 102 patients undergoing 108 PSOs. Twelve patients (11.1%) were found to have a neurologic deficit of two or more motor grades immediately following the procedure. For three patients (2.8%), the deficits were permanent. All three of these patients were able to ambulate. Neurophysiological monitoring did not detect any of the deficits intraoperatively. In all cases, the deficit occurred distal to or at the osteotomy site and was always unilateral. Factors involved include residual dorsal impingement, dural buckling, and osteotomy subluxation. The authors recommended careful closure of the osteotomy site, frequent attention to the neural elements via the central decompression, and an intraoperative wake-up test as neurophysiological monitoring did not detect any deficits.
At five years, Kim and colleagues38 reported on 10 pseudarthroses in 8 patients undergoing PSO. None of the pseudarthroses were at the osteotomy site. Five of the pseudarthroses were discovered after 2 years. The patients tended to be older (>55 years) and have fusions that extended to the sacrum (6 of 8). Nine of the 10 pseudarthroses were at the thoracolumbar junction. The tenth was at L5-S1.
Another complication seen in patients undergoing surgery for sagittal realignment is an acute Fracture at or just above the Proximal aspect of the pedicle Screw Construct (termed FPSC). This appears to be a phenomenon associated more commonly with pedicle screw fixation. O’Leary and colleagues39 reviewed a consecutive series of 13 patients at one institution who sustained acute fracture above the proximal aspect of long pedicle screw constructs (FPSCs). Ten out of 13 patients had significant preoperative positive sagittal imbalance, averaging 13 cm. On average, the SVA of these patients was 3 cm anterior to the posterior superior corner of the sacrum after surgery. When a matched cohort analysis was performed comparing patients with significant sagittal imbalance with and without FPSC, patients sustaining acute proximal junctional fractures tended to be older (average age 66) females, obese (BMI 32), and more osteopenic. A thorough radiographic analysis was completed for the cohort and the FPSC patients. After analyzing sagittal parameters including lumbar lordosis, thoracic kyphosis (T3-T12), sagittal balance (C7 plumb line), pelvic incidence, and a sagittal plumb line from the upper instrumented vertebrae (UIVpl), no differences could be determined between the FPSC group and the cohort group.
Conclusion
Pearls and Pitfalls
Key Points
1 Booth KC, Bridwell KH, Lenke LG, et al. Complications and predictive factors for successful treatment of flatback deformity (fixed sagittal imbalance). Spine. 1999;24(16):1712-1720.
2 Lagrone MO, Bradford DS, Moe JH, et al. Treatment of symptomatic flatback after spinal fusion. J Bone Joint Surg Am. 1988;70(4):569-580.
3 Bridwell KH, Lewis SH, Rinella A, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. Surgical Technique. J Bone Joint Surg Am. 2004;86A(Suppl 1):44-50.
4 Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy versus vertebral column resection for spinal deformity. Spine. 2006;31(19):S171-S178.
5 Buchowski JM, Bridwell KH, Lenke LG, et al. Neurologic complications of pedicle subtraction osteotomy: a 10-year assessment. Spine. 2007;32(20):2245-2252.
1 Rajnics P, Templier A, Skalli W, et al. The association of sagittal spinal and pelvic parameters in asymptomatic persons and patients with isthmic spondylolisthesis. J Spinal Disord Tech. 2002;15:24-30.
2 Bernhardt M, Bridwell KH. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989;14(7):717-721.
3 Stagnara P, DeMauroy JC, Dran G, et al. Reciprocal angulation of vertebral bodies in a sagittal plane: Approach to references for the evaluation of kyphosis and lordosis. Spine. 1982;7(4):335-342.
4 Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. Spine. 1994;19:1611-1618.
5 O’Brien MF, Kuklo TR, Blanke KM, Lenke LG. Spinal deformity study group radiographic measurement manual. 2004 Medtronic Sofamor Danek USA, Inc.
6 Schwab F, Lafage V, Boyce R, et al. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine. 2006;31:E959-E967.
7 Gelb DE, Lenke LG, Bridwell KH, et al. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20:1351-1358.
8 El Fagoun AB, Schwab F, Gamez L, et al. Center of gravity and radiographic posture analysis: a preliminary review of adult volunteers and adult patients affected by scoliosis. Spine. 2005;30:1535-1540.
9 Lafage V, Schwab F, Skalli W, et al. Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine. 2008;33:1572-1578.
10 Doherty JH. Complications of fusion in lumbar scoliosis: proceedings of the Scoliosis Research Society. J Bone Joint Surg Am. 1973;55:438.
11 Bradford DS, Tribus CB. Current concepts and management of patients with mixed decompensated spinal deformity. Clin Orthop. 1994;306:64-72.
12 Denis F. The iatrogrenic loss of lumbar lordosis. The flat back and flat buttock syndromes. In: Farcy J-P, editor. Complex Spinal Deformities. Spine: State of the Art Reviews, Vol. 8. Philadelphia: Hanley & Belkfus, Inc.; 1994:659-680. No. 3
13 Moe JH, Denis F. The iatrogenic loss of lumbar lordosis. Orthop Trans. 1977;1:131.
14 Booth KC, Bridwell KH, LG Lenke, et al. Complications and predictive factors for successful treatment of flatback deformity (fixed sagittal imbalance). Spine. 1999;24:1721-1727.
15 Bridwell KH, Lewis SH, Lenke LG, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal balance. J Bone Joint Surg Am. 2003;85A(3):454-463.
16 Bridwell KH, Lewis SH, Rinella A, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. Surgical Technique. J Bone and Joint Surg Am. 2004;86A(Suppl 1):44-50.
17 Bradford DS, Schumacher WL, Lonstein JE, et al. Ankylosing spondylitis: Experience and surgical management of 21 patients. Spine. 1987;12:238-243.
18 Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop. 1985;194:142-152.
19 Simmons EH. Kyphotic deformity of the spine in ankylosing spondylitis. Clin Orthop. 1977;128:65-77.
20 Brown CJ, Orme TJ, Richardson HD. The rate of pseudarthrosis (surgical nonunion) in patients who are smokers and patients who are nonsmokers: a comparison study. Spine. 1986;11(9):942-943.
21 Lagrone MO, Bradford DS, Moe JH, et al. Treatment of symptomatic flatback after spinal fusion. J Bone Joint Surg Am. 1988;70:569-580.
22 Legaye J, Duval-Beaupere G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99-103.
23 Hanson DS, Bridwell KH, Lenke LG, Rhee JM. Correlation of pelvic incidence with low and high-grade isthmic spondylolisthesis. Spine. 2002;27:2026-2029.
24 Angevine PD, Bridwell KH. Sagittal imbalance. Neurosurg Clin N Am. 2006;17(3):353-363.
25 Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy versus vertebral column resection for spinal deformity. Spine. 2006;31:S171-S178.
26 Gill JB, Levin A, Burd T, Longley M. Corrective osteotomies in spine surgery. J Bone and Joint Surg Am. 2008;90:2509-2520.
27 Bridwell KH. Causes of sagittal spinal imbalance the assessment of the extent of needed correction. Instr Course Lect. 2006;55:567-575.
28 Smith-Petersen MH, Larson CB, Aufranc OE. Osteotomy of the spine for the correction of flexion deformity in rheumatoid arthritis. J Bone Joint Surg Am. 1945;27:1-11.
29 La Marca F, Brumblay H. Smith-Peterson osteotomy in thoracolumbar deformity surgery. Neurosurgery. 2008;63(3 Suppl):163-170.
30 Bridwell KH. Osteotomies for fixed deformities in the thoracic and lumbar spine. In: Bridwell KH, DeWald RL, editors. The Textbook of Spinal Surgery. ed 2. Philadelphia: Lippencott-Raven; 1977:821-835. Philadelphia
31 Cunningham BW, Lewis SJ, Long J, et al. Biomechanical evaluation of lumbosacral reconstruction techniques for spondylolisthesis: an in vitro porcine model. Spine. 2002;27:2321-2327.
32 Tsuchiya K, Bridwell KH, Kuklo TR, et al. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine. 2006;31:303-308.
33 Kim YJ, Bridwell KH, Lenke LG, et al. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow up study. Spine. 2007;32:2189-2197.
34 Suk SI, Chung ER, Kim JH, et al. Posterior vertebral column resection for severe rigid scoliosis. Spine. 2005;30:1682-1687.
35 Bradford DS, Boachie-Adjei O. One-stage anterior and posterior hemivertebral resection and arthrodesis for congenital scoliosis. J Bone Joint Surg Am. 1990;72:536-540.
36 Suk SI, Kim JH, Kim WJ, Lee SM, Chung ER, Nah KH. Posterior vertebral column resection for severe spinal deformities. Spine. 2002;27:2374-2382.
37 Buchowski JM, Bridwell KH, Lenke LG, et al. Neurologic complications of pedicle subtraction osteotomy: a 10-year assessment. Spine. 2007;32:2245-2252.
38 Kim YJ, Bridwell KH, Lenke LG, et al. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow up study. Spine. 2007;32:2189-2197.
39 O’Leary PT, Bridwell KH, Good CR et al. Risk factors and outcomes for catastrophic failures at the top of long pedicle screw constructs (FPSC): a matched cohort analysis performed at a single center. Presentation at 43rd Annual Scoliosis Research Society Annual Meeting, Salt Lake City, UT, September 2008.

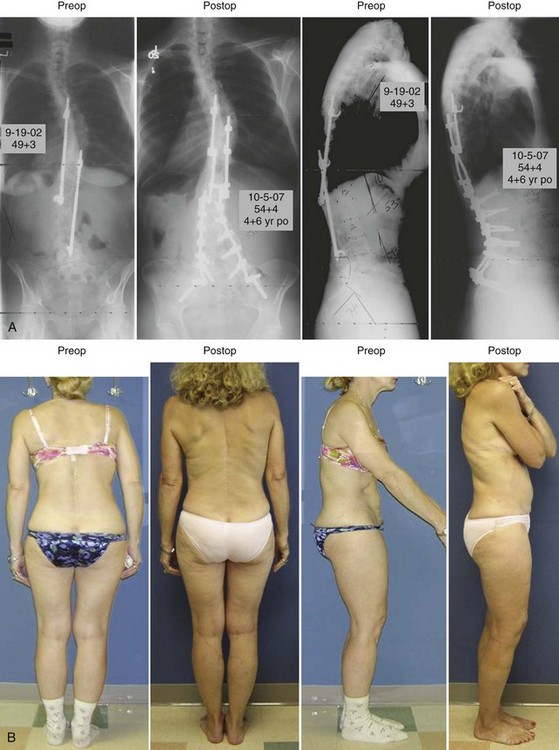
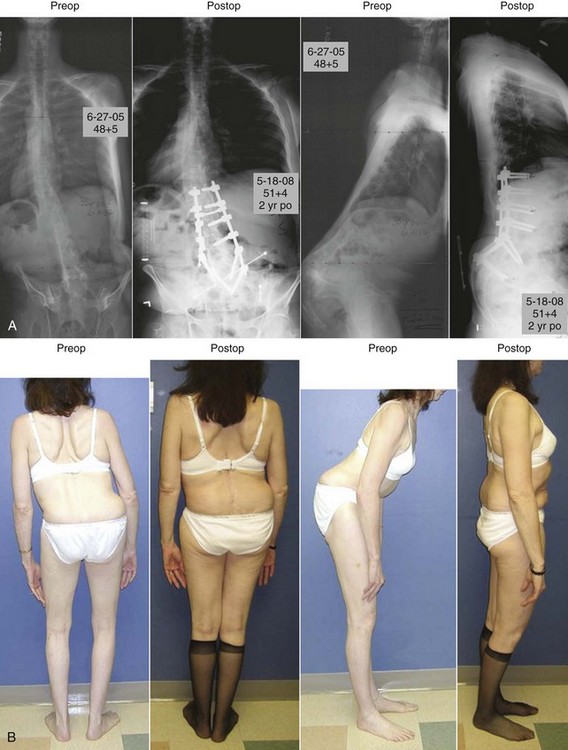
 -year postoperative coronal and sagittal radiographs of a 49-year-old female patient who presented having had Harrington fusion from T4 to L4 as an adolescent. She has now developed severe disc degeneration and spinal stenosis at L4-L5 and L5-S1. She has a mild to moderate sagittal imbalance. She was treated with decompression at L4-L5 and L5-S1 and extension of fusion to the sacrum. To restore sagittal balance, she also had two Smith-Petersen osteotomies (SPOs) performed through the prior fusion mass at L2-L3 and L3-L4 with local bone graft and biologics. B, Standing preoperative and
-year postoperative coronal and sagittal radiographs of a 49-year-old female patient who presented having had Harrington fusion from T4 to L4 as an adolescent. She has now developed severe disc degeneration and spinal stenosis at L4-L5 and L5-S1. She has a mild to moderate sagittal imbalance. She was treated with decompression at L4-L5 and L5-S1 and extension of fusion to the sacrum. To restore sagittal balance, she also had two Smith-Petersen osteotomies (SPOs) performed through the prior fusion mass at L2-L3 and L3-L4 with local bone graft and biologics. B, Standing preoperative and  -year postoperative coronal and sagittal clinical photos of the patient.
-year postoperative coronal and sagittal clinical photos of the patient.