Chapter 8 Fixation of Osteochondral Fragments
Introduction
Osteochondral fragments can also be created by the surgeon in the course of performing osteochondral autografts such as mosaicplasty and mega OATS (Chapters 5 and 6) or osteochondral allografting (Chapter 7).
This chapter reviews the most common methods of fragment fixation.
Indications for Internal Fixation
Few studies provide clear indications for surgical fixation of osteochondral fragments (Table 8-1). The underlying diagnosis has implications in the decision-making process, such as in the treatment of osteochondritis dissecans (OCD).
TABLE 8-1 Indications for Internal Fixation with Regard to Type of Osteochondral Fragment
| Type of Osteochondral Fragment | Indication for Fixation |
|---|---|
| Osteochondral fracture Chondral fracture Osteochondritis Dissecans (OCD) |
Fragment is nondeformed, reducible, viable Lesions that are unstable, partially detached lesions, completely detached lesions that are nondisplaced and viable displaced lesions |
To our knowledge, no quantitative measures of graft stability are available to assist the surgeon in deciding when to perform adjunctive fixation.
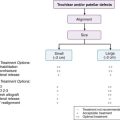
Juvenile Osteochondritis Dissecans
Surgical indication for juvenile osteochondritis dissecans (jOCD) includes failure of 6 to 9 months of nonoperative treatment of a stable lesion, an unstable or detached lesion, or a symptomatic patient with imminent physeal closure within 6 months to a year.1
Adult Osteochondritis Dissecans
Unlike jOCD, symptomatic adult OCD necessitates surgical intervention in most cases because of the progressive course, the inability of the fragment to heal on its own, and the fact that most adult lesions are unstable in nature.2
Massive lesions, multiple fragmented lesions, and substantial craters often require procedures utilizing open bone grafting of the bed or osteochondral autografts and allografts when fixation is not possible or the fragment is not adequate for fixation.3
Traumatic Osteochondral Fragments
In adults there is little evidence that purely chondral fragments have the ability to heal to bone. Nonetheless, surgeons may choose to attempt to repair very thin or small osteochondral fragments with the understanding that there is a significant risk of failure.4,5
One caveat of this approach (and, in fact, in treating any osteochondral fragment with internal fixation) is the avoidance iatrogenic injury to the joint by the fixation device should the fragment collapse or detach, leaving the fixation device proud or loose within the joint. Numerous case reports have documented articular cartilage injury and joint destruction by exposed or loose fixation devices.3–7
Overview of Internal Fixation Devices
The goal of any chosen device should be rigid fixation and compression while establishing a position that is seated low enough as to not interfere with the surrounding articular cartilage (Table 8-2). The device should allow for early range of motion and should retain the ability to be removed, if necessary.8
| Metal Pins and Wires |
| Smooth and threaded metal pins K-wires |
| Cannulated and AO Metal Screws |
| Constant pitch Variable pitch, headless (e.g., Herbert screw) |
| Bioabsorbable Implants |
| Biocompression screws Chondral pins and darts (smooth and barbed) |
| Osteochondral Plugs |
| Autograft bone plug/Osteochondral core |
Pins and Wires
The use of smooth metal pins for fixation was originally described by Smillie in 19579 but has since become more of a historical reference. Good results have been published using K-wires in combination with drilling and bone grafting,8,10 especially when splitting of a smaller fragment is a concern. Other advantages of K-wires include availability, low cost, and ease of use. Disadvantages include lack of compression achieved and possibility of breakage, along with the need for removal.
Cannulated and Variable Pitch Screws
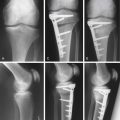
Several options exist with metal screws including cannulated screws and variable-pitch, headless screws. The most commonly referenced variable-pitch screw is the Herbert screw.11–14 This type of screw allows for rigid fixation, as well as having an auto-compression effect. Another advantage to this screw is that the headless design allows it to be countersunk beneath the surface of the articular cartilage.
The disadvantage of the Herbert screw along with the other metal screws is that they may require an additional surgery for removal, and, if the fragment settles or breaks, the screw may become proud, leading to injury of the opposing articular surface. When possible, the surgeon attempts to place these devices in a manner that avoids the articular surface (Fig. 8-1).
Bioabsorbable Implants
They are bioabsorbable, which obviates the need for surgical removal, they are usually low-profile and can be countersunk below the articular cartilage surface and, unlike metallic implants, bioabsorbable implants produce no artifact on imaging studies, facilitating postoperative assessment of fragment healing.15 Some of the complications that have been reported with bioabsorbable implants include the previously mentioned inflammatory reaction, screw loosening and back-out, synovitis, chronic effusions, and lack of adequate compression or fixation with some devices.3,6,7
Osteochondral Plugs
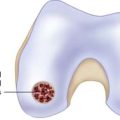
Another innovative method of fixation of osteochondral fragments is the use of bone plugs or osteochondral cores. Miniaci has described a method of using a small osteochondral autograft plug to fix osteochondritis dissecans.16 This technique has the obvious advantage of providing both fragment fixation and bone grafting with a single “device.”
Surgical Technique: Chondral Dart
Darts can be inserted either arthroscopically or with an open procedure after bone grafting or placement of an allograft. The author’s experience is primarily using chondral darts for adjunctive fixation of osteochondral allografts (Chapter 7).
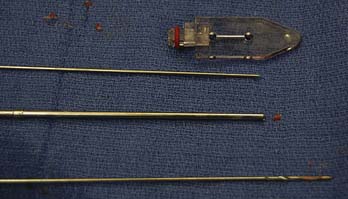
The instruments include a cannulated guide, drill, and insertion tamp, which are designed to allow for 2 mm of countersinking of the dart (Fig. 8-2).
In this case a partial talus shell allograft is to be placed.
After fashioning of the graft (Fig. 8-3) and the recipient site of the medial talus (Fig. 8-4), the graft fragment is seated (Fig. 8-5). Note the relative stability of this fragment because of the conformity of the tibiotalar joint and lateral support of the host talus.
With the fragment in place, the cannulated guide is placed on the articular surface, and the drill is used to prepare the osseous channel for the dart (Fig. 8-6).
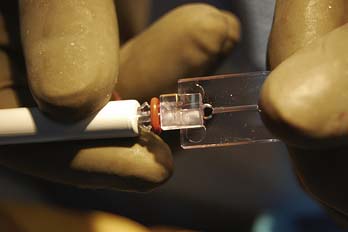
While keeping the guide in place on the fragment, the chondral dart is loaded into the cannulated guide (Fig. 8-7) followed by the insertion tamp, which is gently impacted to seat the dart (Fig. 8-8). Care must be taken to maintain the cannulated guide at the same position and angle during both drilling and dart insertion.
The stability of the fixation can be evaluated, and additional darts can be inserted as necessary. One advantage of darts and pins is the relatively small insertion defect footprint on the articular cartilage (Fig. 8-9).
Surgical Technique: Biocompression Screw
Instruments include a tapered drill and tap (Fig. 8-10) and screwdriver for the implant insertion (Fig. 8-11). In this case example, the patient has an osteochondral lesion of the talus amenable to open grafting and fixation (Fig. 8-12).

FIGURE 8-10 Cannulated drill and tap for insertion of biocompression screw (Arthrex, Naples, Florida).
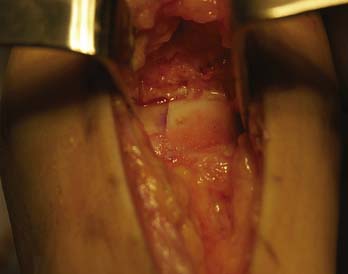
The lesion is elevated to ensure there is adequate bone on the fragment for fixation and healing (Fig. 8-13), and the host bed is prepared by curettage, drilling, and bone grafting to improve the biological milieu (Fig. 8-14). Confirmation of the need for fixation with compression is made by determining fragment stability. It is preferable that the fragment is slightly proud (by addition of bone graft) to accommodate the effect of compression and remodeling of the bone graft and fragment (Fig. 8-15).

FIGURE 8-13 The lesion is elevated to inspect the osseous portion of the fragment and prepare the bone bed.

FIGURE 8-14 Cancellous bone grafting is performed to fill the lesion defect and improve potential for healing.
The amount of countersinking can be adjusted by the depth of drilling and tapping. The biocompression screw is inserted carefully until the fragment is compressed and the screw is adequately countersunk (Figs. 8-16 and 8-17).
Headed screws require an additional step of removing cartilage and bone to allow countersinking of the screw head.
1. Kramer D.E., Kocher M.S. Juvenile osteochondritis dissecans of the knee. Op Tech Sports Med. 2008;16(2):70-76.
2. Kocher M.S., Tucker R., Ganley T.J., et al. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med. 2006;34(7):1181-1191.
3. Scioscia T.N., Giffin J.R., Allen C.R., et al. Potential complication of bioabsorbable screw fixation for osteochondritis dissecans of the knee. Arthroscopy. 2001;17(2):E7.
4. Alford J.W., Cole B.J. Cartilage restoration, part 2: techniques, outcomes and future directions. Am J Sports Med. 2005;33(3):443-460.
5. Sgaglione N.A., Miniaci A., Gillogly S.D., et al. Update on advanced surgical techniques in the treatment of traumatic focal articular cartilage lesions in the knee. Arthroscopy. 2002;18(2 Suppl 1):9-32.
6. Friederichs M.G., Greis P.E., Burks R.T. Pitfalls associated with fixation of osteochondritis dissecans fragments using bioabsorbable screws. Arthroscopy. 2001;17(5):542-545.
7. Weckström M., Parviainen M., Kiuru M.J., et al. Comparison of bioabsorbable pins and nails in the fixation of adult osteochondritis dissecans fragments of the knee. Am J Sports Med. 2007;35(9):1467-1476.
8. Penton J.L., Cascio B.M. Internal fixation of osteochondritis dissecans in the knee. Op Tech Sports Med. 2008;16(2):97-101.
9. Smillie I.S. Treatment of osteochondritis dissecans. J Bone Joint Surg Br. 1957;39:248-260.
10. Anderson A.F., Lipscomb A.B., Coulam C. Antegrade curettement, bone grafting and pinning of osteochondritis dissecans in the skeletally mature knee. Am J Sports Med. 1990;18:254-261.
11. Makino A., Muscolo D.L., Puigdevall M., et al. Arthroscopic fixation of osteochondritis dissecans of the knee: clinical, magnetic resonance imaging, and arthroscopic follow-up. Am J Sports Med. 2005;33(10):1499-1504.
12. Rey Zuniga J.J., Sagastibelza J., Lopez Blasco J.J., et al. Arthroscopic use of herbert screw in osteochondritis dissecans of the knee. Arthroscopy. 1993;9(6):668-670.
13. Cugat R., Garcia M., Cusco X., et al. Osteochondritis dissecans: a historical review and its treatment with cannulated screws. Arthroscopy. 1993;9(6):675-684.
14. Johnson L.L., Uitvlugt G., Austin M.D., et al. Osteochondritis dissecans of the knee: arthroscopic compression screw fixation. Arthroscopy. 1990;6:179-189.
15. Larsen M.W., Pietrzak W.S., DeLee J.C. Fixation of osteochondritis dissecans lesions using poly(l-lactic Acid)/Poly(glycolic Acid) copolymer bioabsorbable screws. Am J Sports Med. 2005;33(1):68-76.
16. Miniaci A., Tytherleigh-Strong G. Fixation of unstable osteochondritis dissecans lesions of the knee using arthroscopic autogenous osteochondral grafting (mosaicplasty). Arthroscopy. 2007;23(8):845-851.