Fingertip eczema

Excessive scaling (hyperkeratosis), erythema, and painful fissures all characterize recurrent eczema of the fingertips. If vesicles are present, consider contact allergy.

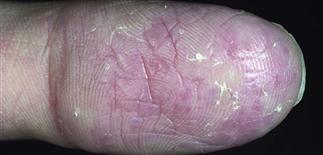
Marked hyperkeratosis and painful fissuring of the palmar and lateral aspects of the fingers. Consider chronic friction, chronic irritant exposures, or psoriasis.

A hyperkeratotic finger with tender areas where plate-like scale has peeled away. It is typically painful, not pruritic. Irritants should be avoided. Systemic retinoids may help if emollients fail.
Mild fingertip eczema with increased linear markings and xerosis. This often responds to bland emollient or topical lactic acid lotion used twice a day. Aggravated by paper handling and low humidity.
DESCRIPTION
Common form of eczema limited to the fingertips. One finger or several fingers can be affected. Itch is limited or is absent often. Tenderness and burning are common presenting complaints.
HISTORY
• Fingertip eczema is usually a recurring winter problem but may occur all year round. • Uncommon in children, it occurs most frequently in adults. • Atopy may be a predisposing factor. • Irritant chemicals or frictional contact may play a role. Repeated frictional contact with paper handling has been implicated as an aggravating factor. • A less frequent etiology is allergic contact dermatitis to plants, resins, glues. • Consider occupational and hobby-related allergens, heat, repeated water exposure, repeated wet–dry cycles, friction. • Cyanoacrylate glue (Crazy Glue) is often used to seal the fissured painful fingertip cracks; contact allergy to this chemical is uncommon but possible. • May last months or years, and can be very resistant to treatment. • Precipitating factors often not easily or consistently avoided. • Inflammation may start on the fingertips but slowly spread to involve fingers and palms.
PHYSICAL FINDINGS
• Dry, scaling, pink, fissured fingertips characterize fingertip eczema. • Peeling reveals red, tender skin. • Fingertips very dry, smooth, red, fragile. Inflammation tends to be chronic. • Vesiculation not typically seen. • Process stops before the distal interphalangeal joint is reached.
TREATMENT
• Avoid repeated wet–dry cycles, irritating detergents or solvents, heat, friction. • Manage as a subacute or chronic eczema; irritants should be avoided and affected areas must be lubricated frequently. • Apply frequently a bland emollient such as Vaseline. • A lactic acid cream (Lac-Hydrin or Amlactin 12% cream) may be helpful. • Medium-potency topical steroids, with or without occlusion, give temporary relief. • Cotton gloves and heavy moisturizers at night can help. • Tar-based creams applied twice each day may be tried if other measures fail. • Protection of hands and affected skin by repeated application of petrolatum and use of cotton gloves can be very helpful. • Decreasing irritation from repeated hand washing and decreasing exposure to other irritants is a cornerstone of treatment. Use household gloves for wet work and cleaning duties. • Patch test patient where occupational exposures to glues, adhesives, resins, or plants (e.g. for florists, dental hygienists, dentists) may be relevant, despite a lack of history of contact with ‘new’ exposures.







