Fibroids
Synonyms/Description
Leiomyoma, myoma, fibromyoma, and uterine fibroma
Etiology
Fibroids are the most common benign pelvic tumor in women. The prevalence in women age 50 and older is estimated at 80% in African Americans and up to 70% in Caucasians. Others have estimated a lower incidence (up to 50% of perimenopausal women).
Myomas are thought to be monoclonal and originate from a single myocyte that undergoes somatic mutation as it grows. Cytogenetic anomalies are found in 40% of fibroids. Estrogen and progesterone are known to stimulate the growth of fibroids. Although many fibroids are asymptomatic, others may cause bleeding, pain, mass effect, urinary frequency, constipation, pregnancy loss, and infertility. The presence of symptomatic fibroids is the most common indication for hysterectomy.
Ultrasound Findings
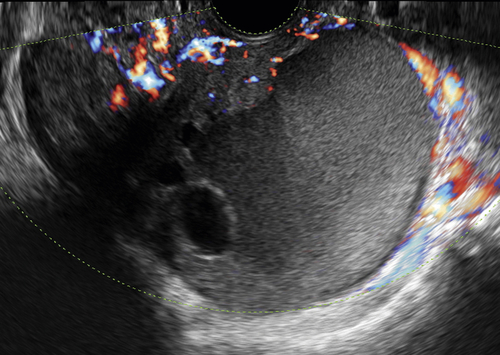
Fibroids are typically solid masses, which are sonographically hypoechoic or isoechoic with the surrounding myometrium. They are well circumscribed, with acoustic shadowing, often with a pattern of stripes or swirls caused by these shadows. They can be calcified, often with a circumferential pattern of calcification. If they degenerate, they can have central cystic portions. Color Doppler findings of fibroids are variable. Some fibroids have abundant flow and others scant; therefore there is no Doppler flow pattern specific to fibroids. Doppler is helpful to map the blood flow to the fibroid. If it is pedunculated, it may be confused with an ovarian mass.
Fibroids are further described by their location in the uterus.
Intramural
Fibroids are most commonly intramural and occur within the confines of myometrium.
Submucosal
A fibroid that protrudes into the endometrial cavity is submucosal. These can occasionally be pedunculated into the cavity and slide down into the cervix as the uterus tries to expel it. Three-dimensional ultrasound and sonohysterography can be very helpful in outlining the extent of the submucosal component of the fibroid within the cavity.
Subserosal
A fibroid that indents the serosal surface and gives a bumpy appearance of the outside of the uterus is subserosal.
Pedunculated
A fibroid that has grown from a subserosal fibroid outward and remains tethered to the uterus by a pedicle is considered pedunculated. Occasionally these can pick up vascularity from outside organs and become parasitic, no longer connected to the uterus, making the sonographic diagnosis more difficult.
Degenerating
Discrepancy between the rate of growth of the myoma and its blood supply can lead to an infarction of part (most often the center) of the myoma. The degenerating fibroid has a variable manifestation, the most common being a donut-appearing mass with a cystic center and a thick wall, located within the confines of the uterus. The acute infarction leads to severe pain and is more common during pregnancy. Some degenerating fibroids can mimic ovarian cystic masses, especially if they are pedunculated and multiseptate in appearance.
Differential Diagnosis
The differential diagnosis of fibroids depends on the location and appearance of the uterine mass. A fibroid that contains cystic areas and abundant blood flow may be indistinguishable sonographically from a uterine sarcoma (see Sarcoma). Follow-up scans showing aggressive growth, particularly in a postmenopausal patient, would suggest a malignancy. If the mass is ill-defined, it may represent an adenomyoma, which is similar in appearance to a fibroid, but has blurry or indistinct borders and is often seen in a setting of adenomyosis (see Endometriosis). If the fibroid is submucosal and more echogenic than usual, it could be confused with an endometrial polyp. A central blood supply with a feeding vessel and cystic spaces would favor a polyp. A bumpy and asymmetric uterus may be confused with a Müllerian duct anomaly such as a unicornuate uterus with a rudimentary horn forming a mass. Three-dimensional ultrasound is essential for diagnosing Müllerian duct abnormalities and the position of fibroids within the uterus.
If the fibroid is pedunculated laterally, in the broad ligament, it may be difficult to distinguish it from a solid adnexal mass such as a fibroma or Brenner tumor. Finding the ipsilateral ovary separate from the mass is important to rule out such entities.
Clinical Aspects and Recommendations
Fibroids are so common and variable in size and location that clinical management and recommendations depend on many variables, such as age, parity, desire for future fertility, bleeding pattern, and hormonal status (e.g., premenopausal vs. postmenopausal). In general, therapies for fibroids include gonadotropin-releasing hormone agonists, hysterectomy or myomectomy (abdominal or transcervical), MRI-guided focused ultrasound surgery, and uterine artery embolization. Symptom severity and a desire to maintain uterine preservation are factors in determining treatment choice.
In patients desiring future fertility, uterine preservation is crucial, and either expectant management or conservative surgery (myomectomy) is employed. Increasingly, minimally invasive techniques (transcervical resection, morcellation for selected submucous myomas, or laparoscopic surgery) would be preferred over traditional open abdominal myomectomy. Conservative management of bleeding can often be accomplished hormonally with combination contraceptives (pills, patch, or vaginal ring), the levonorgestrel-releasing IUD, progestin-only pills, tranexamic acid, and even nonsteroidal anti-inflammatory drugs (NSAIDs) in some patients. Preoperatively, GnRH agonists such as leuprolide or danazol have been employed to reduce uterine size. Some women close to menopause may use such agents to eliminate bleeding and reduce uterine size, thus allowing them to drift into natural menopause, when symptoms and bleeding will cease. In patients with severe symptoms of pelvic pressure, pain, bowel/bladder complaints, or abnormal uterine bleeding, hysterectomy will be definitive therapy. Other less invasive approaches such as high-frequency focused ultrasound (HiFUS) and uterine artery embolization are also used.
Perimenopausal patient’s estradiol levels initially rise as women become anovulatory and produce multiple follicles, without any becoming dominant. This can result in temporary enlargement of fibroids before actual menopause and may concern clinicians. Although uterine sarcomas may be difficult to distinguishsonographically from very vascular fibroids, true leiomyomas are benign and do not undergo malignant degeneration.
Figures
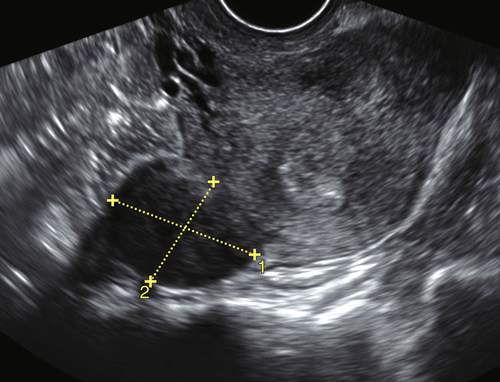
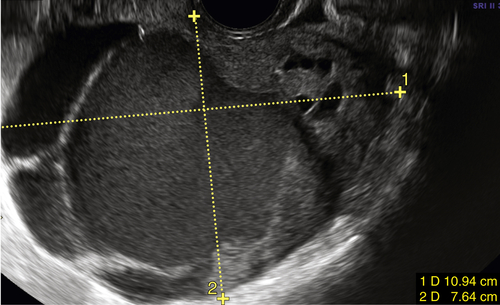
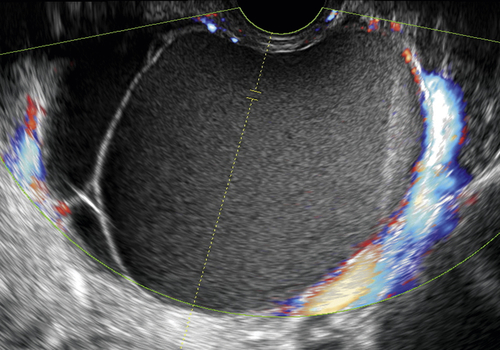
Figure F1-2 Pedunculated fibroid shown by the calipers.
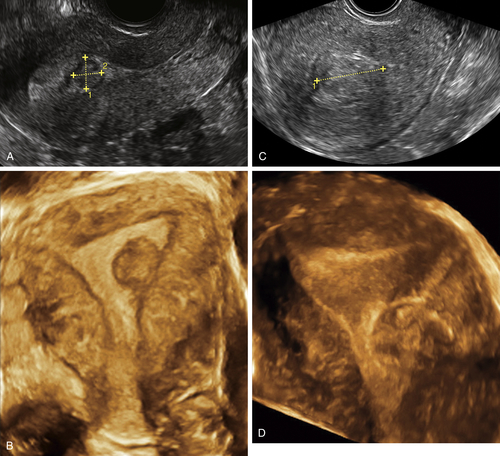
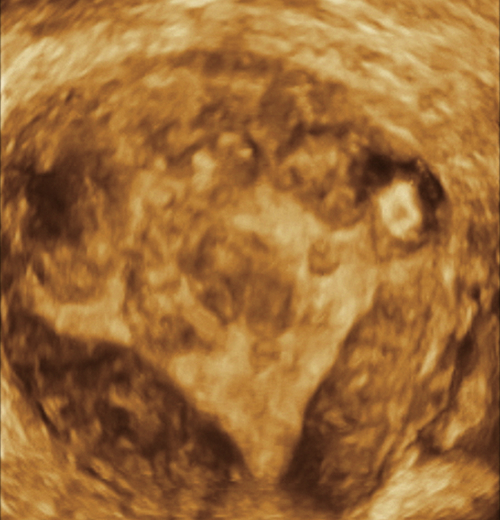
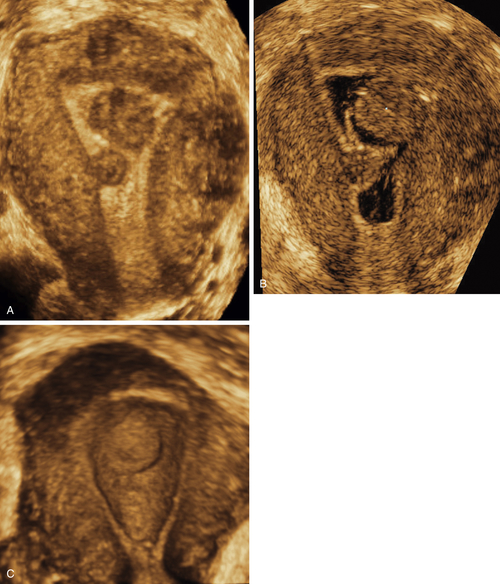
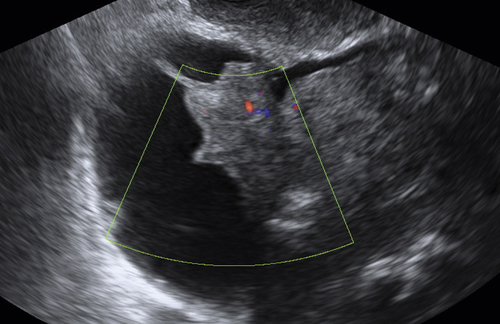
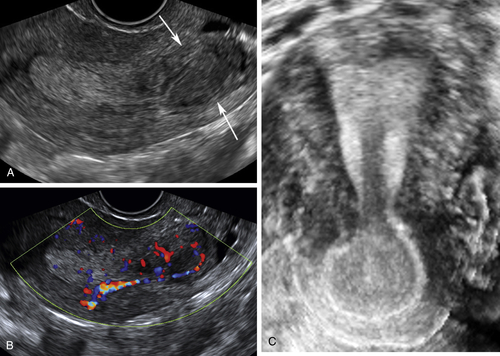
Figure F1-3 Two cases of submucosal fibroids (2-D and 3-D coronal views). A and B, Small, almost completely submucosal fibroid in the left side of the cavity best seen with 3-D. C and D, Larger fibroid, lower in the uterus and 50% submucoal. Three-dimensional imaging is necessary to map out the exact position of the fibroid within the uterine cavity.