W13 Fiberoptic Bronchoscopy
 Before Procedure
Before Procedure
Indications
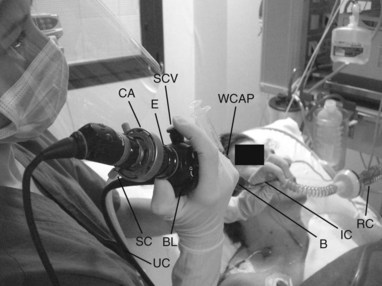
Equipment
 Anatomy
Anatomy
Nomenclature of Peripheral Bronchi
 Procedure
Procedure
 After Procedure
After Procedure
Complications
 Outcomes and Evidence
Outcomes and Evidence
Jackson C, Huber JF. Correlated applied anatomy of the bronchial tree and lungs with a system of nomenclature. Dis Chest. 1943;9:319-326.
Ikeda S. Atlas of flexible bronchofiberscopy. Tokyo: Igaku Shoin; 1974.
Baughman RP, Golden JA, Keith FM. Bronchoscopy, lung biopsy, and other diagnostic procedures. In: Murray JF, Nadel JA, Mason RJ, et al, editors. Textbook of respiratory medicine. 3rd ed. New York: Saunders; 2000:728-759.
British Thoracic Society Bronchoscopy Guidelines Committee, a Subcommittee of the Standards of Care Committee. British Thoracic Society guidelines on diagnostic flexible bronchoscopy. Thorax. 2001;56:11-21.
Bolliger CT, Mathur PN, Beamis JF, et al. ERS/ATS statement on interventional pulmonology. European Respiratory Society/American Thoracic Society. Eur Respir J. 2002;19:356-373.
Ernst A, Silvestri GA, Johnstone D. Interventional pulmonary procedures: guidelines from the American College of Chest Physicians. Chest. 2003;123:1693-1717.
Prakash UBS, Offord KP, Stubbs SE. Bronchoscopy in North America: the ACCP survey. Chest. 1991;100:1668-1675.
Meduri GU, Chastre J. The standardization of bronchoscopic techniques for ventilator-associated pneumonia. Chest. 1992;102:557S-564S.
Murphy PA. Fibre-optic endoscope used for nasal intubation. Anaesthesia. 1967;22:489-491.
Ovassapian A. Fibreoptic endoscopy and the difficult airway, 2nd ed. Philadelphia: Lippincott-Raven; 1996.
Lindholm CE, Ollman B, Snyder JV, et al. Cardiorespiratory effects of flexible fiberoptic bronchoscopy in critically ill patients. Chest. 1978;74:362-368.
Matsushima Y, Jones RL, King EG, et al. Alteration in pulmonary mechanics gas exchange during routine fiberoptic bronchoscopy. Chest. 1984;86:184-188.
Trouillet J, Guiguet M, Gibert C, et al. Fiberoptic bronchoscopy in ventilated patients: evaluation of cardiopulmonary risk under midazolam sedation. Chest. 1990;97:927-933.
Antonelli M, Conti G, Riccioni L, et al. Noninvasive positive-pressure ventilation via face mask during bronchoscopy with BAL in high-risk hypoxemic patients. Chest. 1996;110:724-728.
Antonelli M, Conti G, Rocco M, et al. Noninvasive positive-pressure ventilation vs conventional oxygen supplementation in hypoxemic patients undergoing diagnostic bronchoscopy. Chest. 2002;121:1149-1154.
Antonelli M, Pennisi MA, Conti G, et al. Fiberoptic bronchoscopy during noninvasive positive pressure ventilation delivered by helmet. Intensive Care Med. 2003;29:126-129.