4 Fever and Hypothermia
Fever is defined as an increase in body temperature. Normal body temperature is 36.8°C ± 0.4°C. Normally body temperature varies in a circadian fashion by about 0.6°C, being lowest in the morning and highest in the late afternoon or early evening. In 1998, the Society of Critical Care Medicine and Infectious Disease Society of America suggested that is “reasonable in many ICUs to consider all patients with temperatures ≥ 38.3°C to be febrile, warranting special attention to determine if infection is present.”1
Fever is triggered by the release of various cytokines—notably, interleukin 1-beta (IL-1β), tumor necrosis factor (TNF), and interleukin 6 (IL-6)—that are capable of up-regulating expression of the enzyme cyclooxygenase (COX)-2 and thereby causing secretion of prostaglandin E2 (PGE2) in the hypothalamus.2 PGE2 binds to prostaglandin receptors located on a cluster of neurons in the preoptic region of the hypothalamus. Although there are four subtypes of PGE2 receptors, only one, PGE2 receptor 3 (EPR3), is required for the development of fever in response to IL-1β, lipopolysaccharide (LPS), or PGE2.2 Activation of EPR3 triggers a number of neurohumoral and physiologic changes that lead to increased body temperature. The antipyretic effects of various nonsteroidal antiinflammatory drugs (NSAIDs) such as aspirin and ibuprofen is due to inhibition of COX-2-dependent PGE2 biosynthesis in the central nervous system (CNS). The mechanism whereby acetaminophen reduces fever is probably independent of COX-2 inhibition and remains controversial and poorly understood.3,4
Body temperature can be measured using an oral, axillary, or rectal mercury-filled glass thermometer. These traditional approaches, however, have been largely replaced by a variety of safer and more environmentally friendly methods that use thermistors located on catheters or probes situated in the pulmonary artery, distal esophagus, urinary bladder, or external ear canal.3 Infrared detectors can also be used to measure tympanic membrane temperature. Forehead skin temperature can be measured using a temperature-sensitive patch.
Fever is a cardinal sign of infection. Accordingly, the new onset of fever should trigger a careful diagnostic evaluation, looking for a source of infection. The diagnostic evaluation should be thorough and tailored to the recent history of the patient. For example, the possibility of a CNS infection should receive greater attention in a patient with recent or ongoing CNS instrumentation. By the same token, if a patient recently underwent a gastrointestinal surgical procedure, the clinician should have a high index of suspicion for an intraabdominal source of infection. Key elements in the assessment of new-onset fever in the intensive care unit (ICU) are listed in Box 4-1. Common sources of infection in ICU patients are listed in Box 4-2.
Box 4-1
Key Elements in the Evaluation of New-Onset Fever in ICU Patients
Box 4-2
Common Infectious Causes of Fever
Although fever in the ICU is most commonly due to infection, myriad noninfectious causes of systemic inflammation (Box 4-3) can also result in hyperthermia. Some authors claim that noninfectious causes of fever rarely result in a core temperature above 38.9°C,5,6 but rigorous data in support of this view are lacking. Still, infections are rarely if ever associated with core temperatures over 41.1°C. When the core temperature is this high, the clinician should suspect malignant hyperthermia, neuroleptic malignant syndrome, or heat stroke.
Box 4-3
Noninfectious Causes of Fever
In general, fever should not be treated with antipyretics. This view is founded on data that suggest that hyperthermia is an adaptive response that enhances the host’s ability to fight infection.7,8 In addition, body temperature is an unreliable clinical parameter when patients are receiving antipyretic therapy. These considerations notwithstanding, antipyretic therapy should be administered to selected patients with fever, among them patients with acute coronary syndromes (i.e., myocardial infarction or unstable angina), because the tachycardia that usually accompanies the febrile response can exacerbate imbalances between myocardial oxygen delivery and demand. Febrile patients with head trauma, subarachnoid hemorrhage, or stroke should receive antipyretics to prevent temperature-related increases in cerebral oxygen utilization. Children with temperatures higher than 40°C or with a history of seizures should also be treated.
Hypothermia blankets are often used to lower the core temperature in febrile ICU patients, but these blankets are no more effective in cooling patients than antipyretic agents.9 Hypothermia blankets can cause large temperature fluctuations and are associated with rebound hyperthermia when removed.8 Additionally, external cooling can augment hypermetabolism and actually promote persistent fever. Lenhardt and colleagues demonstrated that active external cooling in volunteers with induced fever increased oxygen consumption by 35% to 40% and was associated with a significant increase in circulating epinephrine and norepinephrine concentrations.10
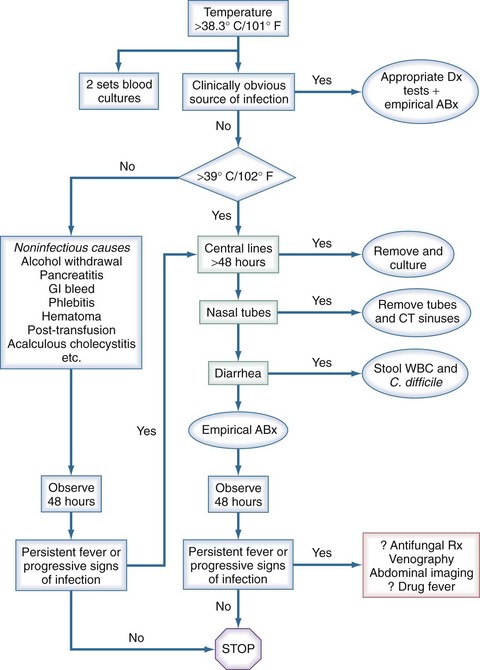
A reasonable approach for evaluating fever in ICU patients was described by Marik.4 As depicted in Figure 4-1, blood cultures should be obtained whenever an ICU patient develops a new fever. The sensitivity of blood cultures for detecting bacteremia depends to a large extent on the volume of blood inoculated into culture media. Whenever possible, at least 10 to 15 mL of blood should be withdrawn and inoculated into 2 or 3 bottles or tubes at a ratio of 1 mL of blood per 5 mL of medium.1
Intravascular catheters are commonly suspected as a source of infection and fever in ICU patients; they can cause fever due to localized or systemic (bloodstream) infection. In patients with new-onset fever without other ominous signs (e.g., hypotension, profound thrombocytopenia, acute respiratory distress syndrome), it is unnecessary to remove all intravascular catheters. In contrast, if one or more of these (or other ominous) signs is present, the most prudent course of action is to remove all vascular access catheters, including tunneled and/or cuffed devices, and culture the tips using semiquantitative methods on solid media.1
Fever is a common feature of the systemic inflammatory response syndrome (SIRS), irrespective of whether the underlying cause is infectious or noninfectious.11 Procalcitonin, a precursor of the polypeptide hormone, calcitonin, has been studied extensively as a circulating marker that can be used to differentiate infectious from noninfectious causes of SIRS in ICU or emergency department patients. Although enthusiasm for this approach for determining the presence of sepsis (i.e., SIRS plus infection) was initially high, one recent meta-analysis suggested that the performance of this test is low, and that measurements of procalcitonin are unreliable for distinguishing infectious from noninfectious causes of SIRS in critically ill adult patients.12 In contrast to these findings, another recent meta-analysis, which had looser criteria for the inclusion of studies, concluded that “procalcitonin represents a good biological diagnostic marker for sepsis, severe sepsis, or septic shock.”13 At present, therefore, it seems likely that measurements of procalcitonin might be a useful adjunct for the evaluation of fever in ICU patients, but this assay is not a replacement for other key diagnostic modalities: careful physical examination; chest x-ray; assessment of sputum Gram stain findings; and appropriate cultures of blood, urine, and sputum or bronchoalveolar lavage fluid.
1 O’Grady NP, Barie PS, Bartlett JG, et al. Practice guidelines for evaluating new fever in critically ill adult patients. Clin Infect Dis. 1998;26:1042-1059.
2 Dinarello CA. Review: infection, fever and exogenous and endogenous pyrogens: some concepts have changed. J Endotoxin Res. 2004;10:201-222.
3 Chandrasekharan NV, Dai H, Roos KLT, et al. COX-3, a cyclooxygenase variant inhibited by acetaminophen and other analgesic/antipyretic drugs: cloning, structure, and expression. Proc Natl Acad Sci USA. 2002;99:13926-13931.
4 Anderson BJ. Paracetamol (acetaminophen): mechanism of action. Ped Anesthesia. 2008;18:915-921.
5 Marik PE. Fever in the ICU. Chest. 2000;117:855-869.
6 Cunha BA. Fever in the intensive care unit. Intensive Care Med. 25, 1999. 658-651
7 Kluger MJ, Ringler DH, Anver MR. Fever and survival. Science. 1975;188:166-168.
8 Bernheim HA, Kluger MJ. Fever: effect of drug-induced antipyresis on survival. Science. 1976;193:237-239.
9 O’Donnell J, Axelrod P, Fischer C, Lorber B. Use and effectiveness of hypothermia blankets for febrile patients in the intensive care unit. Clin Infect Dis. 1997;24:1208-1213.
10 Lenhardt R, Negishi C, Sessler DI, et al. The effects of physical treatment on induced fever in humans. Am J Med. 1999;106:550-555.
11 Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31:1250-1256.
12 Tang BM, Eslick GD, Craig JC, McLean AS. Accuracy of procalcitonin for sepsis diagnosis in critically ill patients: systematic review and meta-analysis. Lancet Infect Dis. 2007;7:210-217.
13 Uzzan B, Cohen R, Nicolas P, Cucherat M, Perret G-Y. Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: a systematic review and meta-analysis. Crit Care Med. 2006;34:1996-2003.