Fetal monitoring and prenatal diagnosis
HCG
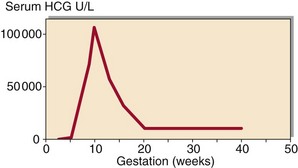
Human chorionic gonadotrophin (HCG) is a glycoprotein produced by the chorionic cells of the developing embryo that is detectable by sensitive assays within days of conception. Measurement of HCG is used to confirm pregnancy, and forms the basis of pregnancy tests (p. 9). The protein’s rapid rate of synthesis in early pregnancy provides systemic evidence of the blastocyst 24 hours after implantation. HCG continues to be secreted by the developing placenta, and serum and urine concentrations increase during the first 9 weeks of pregnancy, then decline gradually until the third trimester (Fig 75.1). The function of HCG is to maintain the activity of the corpus luteum sustaining progesterone synthesis. Measurement of HCG is also of value in:
 Assessing fetal viability in threatened abortion.
Assessing fetal viability in threatened abortion.
 Detecting ectopic pregnancy. HCG fails to rise at the expected rate. In the first trimester of a normal pregnancy it approximately doubles every 48 hours.
Detecting ectopic pregnancy. HCG fails to rise at the expected rate. In the first trimester of a normal pregnancy it approximately doubles every 48 hours.
 Detecting and monitoring hydatidiform mole and choriocarcinoma. HCG may be used as a tumour marker for diagnosis and monitoring of these trophoblastic malignancies (pp. 140–141).
Detecting and monitoring hydatidiform mole and choriocarcinoma. HCG may be used as a tumour marker for diagnosis and monitoring of these trophoblastic malignancies (pp. 140–141).
Prenatal diagnosis
Prenatal diagnostic techniques fall into two groups: invasive and non-invasive (Table 75.1). Prenatal diagnosis may be required because of increased risk of inherited disease. Neural tube defects cannot usually be predicted by family history, and pregnant women may be offered a screening test to detect these disorders. For further details on antenatal screening see pp. 154–155.
Table 75.1
Techniques for prenatal diagnosis
| Invasive | Amniocentesis |
| Chorionic villus sampling | |
| Cordocentesis | |
| Fetoscopy | |
| Fetal skin biopsy | |
| Fetal liver biopsy | |
| Non-invasive | Ultrasound |
| Radiography |
Alpha-fetoprotein
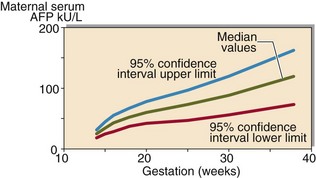
Alpha-fetoprotein (AFP) is a small glycoprotein synthesized by the yolk sac and fetal liver and is a major fetal plasma protein. Because of its size it appears in fetal urine, and hence it is present in amniotic fluid and maternal blood. AFP concentrations increase in maternal blood until 32 weeks of gestation in a normal pregnancy (Fig 75.2).
Bilirubin
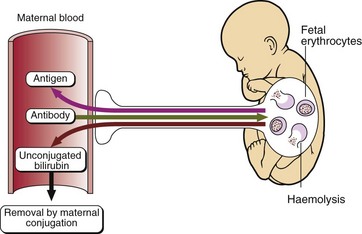
Bilirubin is measured in amniotic fluid to aid in the assessment of fetal risk in rhesus incompatibility. Incompatible red cell antigens can enter the maternal circulation either from the fetus at the time of delivery or, rarely, because of incompatible blood transfusion; specific red cell antibodies are stimulated in the mother. If a Rh –ve mother has a Rh +ve child these antibodies may cross the placenta and react with specific antigens to the fetal red cell membrane causing haemolysis (Fig 75.3). This is unusual in a first pregnancy but may be a feature of subsequent pregnancies. Excess breakdown of red cells leads to anaemia, overproduction of bilirubin and, eventually, oedema.
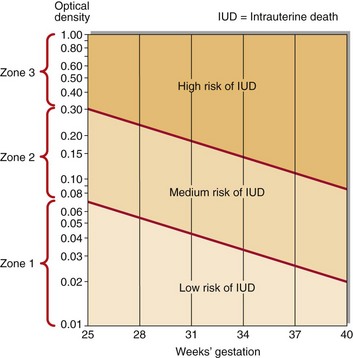
During fetal life, unconjugated bilirubin crosses the placenta and is removed by the mother, so the baby may not be born with obvious jaundice. However, the baby will rapidly become jaundiced in the days immediately after birth. In utero, the level of bilirubin in the amniotic fluid can be used to predict the severity of the fetal condition. Amniocentesis is performed on women who have previously had an affected fetus and on women who show a high and rising Rh titre. The severity of the problem can be assessed by reference to a nomogram that relates bilirubin levels to gestational age, such as that in Figure 75.4. Fetal exchange blood transfusion or early delivery may be considered.