CHAPTER 12 Fertility Challenges
Infertility is defined as the inability to conceive after 12 months of unprotected intercourse in a couple of reproductive age attempting to conceive. Approximately 90% of couples achieve conception within this time, and a further 15% of normally fertile couples take longer than 12 months to become pregnant. Research has shown that even couples in their late thirties have a 91% chance of conceiving naturally within 2 years, and recent studies estimate that an average of 25% to 40% of women have a live birth without treatment during the 3 years after the first infertility consultation, even without treatment. 1 2 3 Nevertheless, of the approximately 60 million women of reproductive age in the United States in 1995, about 1.2 million, or 2%, had had an infertility-related medical appointment within the previous year and an additional 13% had received infertility services at some time in their lives.4 This number has increased in recent decades because of societal demographic changes, particularly the aging of the baby boom generation, leading to an increased size of the reproductive age population, and more couples delaying fertility for the sake of careers.1
Infertility is not synonymous with sterility and it is important to differentiate these terms. Sterility is defined the inability to achieve pregnancy and affects only 1% to 2% of couples.2 Primary infertility refers to those who have never before conceived and secondary infertility to those who have achieved conception some time in the past (regardless of pregnancy outcome) and thereafter became infertile.5
FEMALE FACTORS AFFECTING FERTILITY
The main types of female infertility include ovulatory disorders (25%) and tubal disease (20% to 25%), including endometriosis (10%). Ovulatory factors are suspected when menstrual abnormalities are reported. Male infertility is the primary cause in approximately 25% of cases and contributes to an additional 15% to 25% of cases. Infertility results from unexplained causes in up to 20% of cases.1 Thorough evaluation of the couple will point to a probable cause in 85% to 90% of cases.2 Ovarian factors are primarily associated with follicular phase disruptions. An inadequate luteal phase is said to account for only 3% to 4% of fertility failure. Examples of all of the factors that account for fertility challenges are listed in Table 12-1.
| FACTOR | EXAMPLES |
|---|---|
| Ovulatory |
Data from Kaider A, Kaider B, Janowicz P, et al.: Immunodiagnostic evaluation in women with reproductive failure, Am J Reprod Immunol 42(6):335-346, 1999.
MALE FACTORS AFFECTING FERTILITY
Male factors affecting fertility include:
DIAGNOSIS
Evaluation of Male Factors
A secondary evaluation is recommended and usually includes more holistic measures:
Evaluation of Female Factors
Primary evaluation should include:
A secondary evaluation is recommended, especially for unidentified infertility:
In a tertiary evaluation for pelvic factors, minor surgery is often required. These tests require referral to a reproductive medical specialist. These tests and procedures, although sometimes necessary, are invasive, painful, and expensive:
Noninvasive Home Evaluation and Patient Participation: Thermo-Symptal Monitoring and Mucus and Cervical Evaluation for Detection of Ovulation
Basal Body Temperature Monitoring
Monitoring Cervical Mucus Changes
Daily monitoring of the texture, quality, and quantity of cervical mucus secretions can be useful to predict ovulation. Cervical mucus secretions change throughout the cycle under the influence of estrogen and progesterone. Approximately 2 or 3 days before ovulation occurs, the estrogen levels peak and the nature of the mucus changes from a pasty thick or milky consistency to a distinctive “spinnbarkeit”: stretchy mucus (usually 6 to 10 cm) of wet consistency and opaque color. It resembles a similar texture and nature to raw egg white. At this stage of the cycle, the mucus is an optimal reservoir to nourish sperm and encourage their survival for conception. When seen under a microscope, fertile spinnbarkeit mucus dries into a distinctive crystalline fernlike pattern. Small, inexpensive ovulation predictor microscopes for home use are available to assist couples in predicting ovulation. Saliva is usually used on the microscope as an alternative to cervical mucus, because saliva mimics the ferning pattern of the spinnbarkeit at the ovulation time. When estrogen levels are lower in the early follicular phase and midluteal phase of the cycle, the mucus secretions are thin, milky, and sparse in nature. When a woman is monitoring cervical mucus, it is recommended she feel the texture of the mucus (at the vaginal opening) between the forefinger and thumb and not use toilet tissue to collect the sample. It absorbs moisture and may lead to misinterpretation of the mucus viscosity. Home test kits that measure urinary LH levels are available for ovulation prediction. These are single use tests and their disadvantage is the expense when used regularly.
CONVENTIONAL TREATMENT APPROACHES
Despite developments in fertility knowledge and technologies, the overall prognosis for achieving childbirth with reproductive technologies is approximately 50%, and declines as women age. Each treatment option has overt and hidden costs, including emotional, physical, and financial burdens, often without justification because of lack of success. Couples entering fertility treatment need to be fully cognizant of the potential price of treatment in all of these areas, and the benefit vs. costs must be evaluated. Patients must also consider the high frequency and implications of a multiple pregnancy, a common outcome with assisted reproductive technologies. Psychological support should be available to all couples considering reproductive technologies, with no blame laid upon either partner, and a realistic appraisal of the chances for success and failure of treatment honestly provided. Reproductive expert Marcelle Cedars advises, “The option of child-free living should also be included in any discussion. At times couples must be advised to stop treatment if the likelihood for success is quite low. Frequently this is a very difficult time for both the patient and the physician, but fruitless treatment should be avoided.”1
Ovarian Stimulation Therapy
When elevated prolactin levels are causing amenorrhea or luteal phase defects are confirmed (e.g., in PCOS), bromocriptine is used. In this circumstance, thyroid function is also evaluated, as primary hypothyroidism can cause elevated prolactin levels. Many pharmaceutical drugs can also cause hyperprolactinemia as a side effect. This needs to be considered and ruled out. Hyperprolactinemia is treated using bromocriptine, a dopamine agonist. Administration is either oral or vaginally at doses of 2.5 mg twice daily or 0.5 mg twice a week. Bromocriptine does not increase the risk of inducing multiple pregnancies. Side effects include weakness, nausea, and nasal congestion.
Pelvic Factors
Endometriosis and the effects of salpingitis are the most common problems causing infertility related to pelvic factors. These affect the structural health of the fallopian tubes, as well as uterine and endometrial tissue. Salpingitis is usually caused by infections with microorganisms such as Neisseria gonorrhea and Chlamydia trichomatosis; other infective organisms include Escherichia coli, Mycoplasma hominis, and Ureaplasma urealyticum.7 Bacterial vaginosis is common among these women. Antibiotic drugs are the usual treatment for these infections.8 The treatment option for moderate and advanced endometriosis is usually surgical; at the time of a laparoscopy, resection and ablation is performed. Fibroids are usually left untouched and are only addressed if multiple miscarriages have been a problem. ART is available for those who are unable to conceive after surgery for common pelvic factors.
Unexplained Infertility
When both partners’ evaluations yield negative results, this is defined as unexplained infertility. This is found in only 10% of cases.8 The main courses of treatment for couples with unexplained fertility include observation of the cycle and refining of timing techniques for intercourse, ovarian stimulation, IUI, GIFT, and IVF.
THE BOTANICAL PRACTITIONER’S PERSPECTIVE
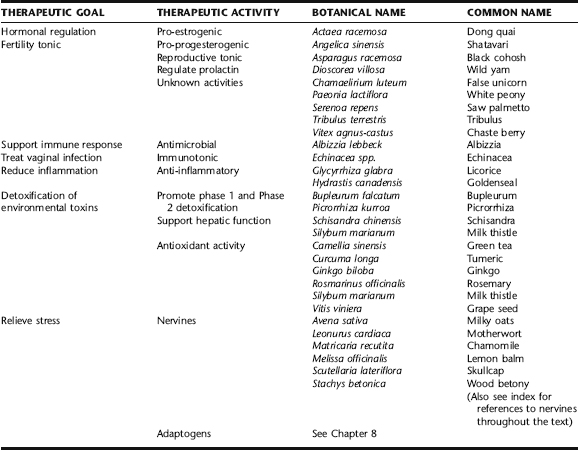
Botanical treatment of infertility cannot address overt physical impediments to fertility; however, it can provide treatment and support for numerous fertility-related problems, such as hormonal dysregulation, thyroid and adrenal disorders, genitourinary infections, immune dysregulation, and stress-related problems (Table 12-2). The herbal consultation also takes into account factors such as nutritional deficiency and occupational/environmental exposures. Most importantly, a holistic practitioner reviews the case as a totality of contributing factors, not simply a reproductive issue.
DISCUSSION OF BOTANICAL PROTOCOL
Black Cohosh
Black cohosh was thought to have estrogen-modulating activity and is used for both ovarian insufficiency affecting fertility and estrogen dominance affecting infertility (e.g., one factor in PCOS) (See Plant Profiles: Black cohosh for a discussion on the research and possible mechanisms of action). It has been described as a selective estrogen receptor modulator (SERM). It was a favorite herb of the native North American Indians and Eclectic physicians for amenorrhea, as a uterine tonic and a number of other gynecologic applications. 9 10 11 Black cohosh has been subjected to extensive clinical trials, demonstrating some estrogen-modulating activity and ability to reduce elevated LH levels, while not affecting FSH and prolactin in any way. In modern herbal applications, black cohosh is indicated for infertility associated with anovulation, PCOS, ovulatory pain, and secondary amenorrhea. Some common side effects have been noted, including a frontal headache with a dull, full, or bursting feeling and a low frequency of stomach complaints, including nausea and vomiting. These side effects are most likely with the high end of a therapeutic daily dose. Recent concerns have arisen that black cohosh may be associated with liver disease, including liver failure; therefore, caution should be observed with its use. (See Plant Profiles: Black cohosh.) It is recommended that this herb be avoided in pregnancy.
Chaste Berry
Chaste berry has a long history of use for regulating menstrual cycles, which may result from its ability to regulate prolactin levels, enhance corpus luteum development, and correct relative progesterone deficiency. Vitex is beneficial for ovulatory factors associated with infertility, in particular, modulating the anterior pituitary’s production of luteinizing hormone (LH), while mildly inhibiting follicle stimulating hormone (FSH). Vitex has been shown to downregulate the production of excess prolactin in hyperprolactinemia via dopaminergic activity.9,12 In an uncontrolled study, chaste berry reduced elevated prolactin levels in 80% of 34 women with hyperprolactinemia at a dosage of 30 to 40 mg per day for 1 month and improved symptoms of a variety of menstrual disorders, including secondary amenorrhea, cystic hyperplasia of the endometrium, deficient corpus luteum function, metrorrhagia, polymenorrhea, and oligomenorrhea.9 Chaste berry reduces thyroxin-releasing hormone (TRH)–induced prolactin release (essentially a pituitary–thyroid axis problem), normalizes shortened luteal phases, corrects luteal phase progesterone deficiencies, and reduces PMS symptoms in women with luteal phase defects caused by latent hyperprolactinemia. In two uncontrolled studies involving 45 infertile women with normal prolactin and pathologically low progesterone, 39 of the women achieved pregnancy after 3 months on chaste berry. In a second study involving 31 women with infertility, after 3 months 15 of these women were pregnant. Of these, seven women who became pregnant using chaste berry, seven previously had amenorrhea, four had luteal insufficiency, and four had been diagnosed with unexplained infertility.
Shatavari
Shatavari is a traditional Ayurvedic herb. The root is used medicinally. In the Indian medicine system, shatavari is said to “give her capacity to have a hundred husbands.”13 In traditional Ayurvedic gynecologic prescribing, shatavari has been used as a nutritive tonic, general female reproductive tonic, fertility tonic, treatment for sexual debility, and as an aphrodisiac. It has also been used traditionally as a tonic for lactating women to improve the quality and quantity of breast milk. Pharmacologic research has found the key constituents of shatavari are steroidal saponins, including shatavarin-I, alkaloids, and mucilage. The presences of the steroidal saponins suggest shatavari’s activity as an estrogen modulator and a menstrual cycle regulator. Shatavari has adaptogenic and immunomodulating properties and can be used as a very useful tonic herb for women with stress-induced and immune-mediated infertility. It has antibacterial action; hence, it should be considered a general reproductive tonic for any woman who has a history of genitourinary infections. There are no known contraindications to the use of shatavari. The daily dose is 4.5 to 8.5 mL of a dried plant extract.
Saw Palmetto
The Eclectic physicians used saw palmetto as a urinary and reproductive tract remedy for inflammation. It was widely used for ovarian pain, pelvic congestion, and atrophy of the ovaries. It proves to be a useful herb to include for infertility in cases of pelvic factors associated with infertility and infertility caused by PCOS. It is known to inhibit the production of prolactin from the pituitary.20 If there is a history of genitourinary infection or pelvic inflammatory disease (PID), Saw palmetto is a valuable herb. The daily dose is 2 to 4 mL of a dried plant extract.
Tribulus
There is little information on the traditional use of tribulus leaf. In Ayurvedic medicine, the fruit has been used for improving male fertility and male erectile function, uterine disorders, urinary disorders, kidney stones, gout, and gonorrhea. As a result of Bulgarian research, tribulus has become a popular herb for the treatment of infertility, menopause, and low libido. It acts as a general tonic, aphrodisiac, and is used to restore vitality, reduce the physiologic effects of stress, and is a powerful fertility tonic for both men and women.9
Open-label clinical trials have demonstrated improvements in both male and female infertility.14 Bulgarian research has identified a unique steroidal saponin known as a furostanol saponin, calculated to no less than 45% protodioscin. The leaf is noted to be higher in the unique saponin than the fruit. Other active constituents include phytosterols and spirostanol glycosides. The results of studies and clinical trials with tribulus have been remarkable, both in animal and human models. When given at a dose of 750 mg per day for 5 days it increased serum FSH and estradiol when compared with baseline in females, and increased LH and testosterone in males, demonstrating an increase in sex hormone production for both men and women.9 The steroidal saponins are thought to bind and weakly stimulate the hypothalamic estrogen receptor sites. The tonic activities of tribulus have been shown to act by intensifying protein synthesis and enhancing the activity of enzymes associated with energy metabolism. It increases iron absorption from the small intestines and inhibits lipid peroxidation during stress. This leads to more muscle strength and improved endurance and stamina.9 Another stunning study showed that tribulus increased serum growth hormone, insulin, and aldosterone without exceeding normal values. Protodioscin, the steroidal saponin in tribulus, has been shown to improve sexual desire via the conversion of protodioscine to dehydroepiandrosterone (DHEA).15 It has been observed that tribulus grown in different soils does not consistently produce the important active furosterol, protodiocin. To ensure the desired clinical results, it is recommended to use only Bulgarian-grown tribulus standardized to 40% furosterol saponins by UV analysis. It is not interchangeable with Chinese or Indian tribulus. When samples of these were analyzed, they were shown to contain only 3% steroidal saponins by UV analysis, and none of these steroidal saponins are the unique and desirable furosterols. Specific female fertility studies have been conducted with tribulus. In an open study with 36 infertile women who were given tribulus on days 5 to 14 of the menstrual cycle for 2 to 3 months, 6% became pregnant as a result of normalized ovulation, 61% demonstrated normalized ovulation and no pregnancy, and 33% demonstrated no effect from tribulus within the 2- to 3-month time frame of the study.16 In this same study, another subgroup of women used tribulus concurrently with pharmaceutical ovarian stimulation with the drug epimestrol. Of the 62 women in this group, within 2 to 3 months, 39% had normalized ovulation and resultant pregnancy, 35% had normalized ovulation with no pregnancy, and the remaining 26% had no effect from the combined therapy. The results obtained from using tribulus concurrently with epimestrol were better than using the drug alone.
Although no increased frequency of fetal malformation or other harm has been observed in limited use by women during pregnancy, tribulus is considered contraindicated in pregnancy according to TCM, and in at least one animal study, decreased survival in the offspring of penned pregnant ewes fed the herb was observed.14 Animal studies of the minor alkaloid fraction of tribulus indicate that it inhibits acetylcholine, depressing activity of the frog heart in situ. The aqueous fraction produced mild hypotension. In dogs, an alcoholic extract of the whole plant produced a sharp vasodepression through a cholinergic mechanism.16 Ingestion of tribulus by sheep produced outbreaks of a locomotor disorder known as staggers, an asymmetric locomotor disorder in sheep produced by a central functional abnormality.17 Ingestion of tribulus caused photosensitivity in animals. No human or animal teratogenicity data are available, and scientific evidence for the safe use of tribulus during pregnancy is not available. The daily dose of tribulus is equivalent to 40 g per day of dried leaf or a concentrated extract standardized to contain a minimum of furostanon saponins as protodioscin at 300 to 400 mg per day. It is best used on days 5 to 14 of the menstrual cycle for enhanced fertility. It is essential to ensure phytoequivalence for optimal therapeutic outcomes. It is advisable to discontinue tribulus use during the luteal phase of the menstrual cycle, and to absolutely not resume use if pregnancy is suspected.
White Peony
White peony is commonly used in traditional Chinese and Japanese medicine for gynecologic conditions. It is generally used for infertility associated with PCOS, hyperprolactinemia, endometriosis, ovarian failure, and androgen excess. Paeonia has been shown to positively influence low progesterone, reduce elevated androgens (testosterone), and modulate estrogen and prolactin. In vitro, the active constituent paeoniflorin has been shown to affect the ovarian follicle by its action on the aromatase enzyme. Aromatase is important for follicular maturation, ovulation and corpus luteum function, steroid hormone synthesis, and the regulation of conversion of androgens to estrogens. The biofeedback in the pituitary and hypothalamus rely on aromatase to regulate prolactin and gonadotrophin-releasing hormone (GnRH). Excess levels of prolactin and GnRH inhibit the activity of aromatase. In TCM, Paeonia is always used in combination with other herbs. A TCM formula that contains Paeonia lactiflora and used in application for infertility is Keishi-bukuryo-gan (TJ-25) or Cinnamon and Hoelen Formula. One study with TJ-25 demonstrated, when used for 14 consecutive days in rats, increased plasma levels of LH by 94%, FSH by 67%, and estradiol by 50%. This formula is thought to be a GnRH antagonist and mildly antiestrogenic. When combined with Glycyrrhiza glabra, Paeonia lactiflora is effective at promoting fertility and improving pregnancy rates in cases of androgen excess, as learned from the TCM Licorice and Peony Formula.18 This combination regulated LH to FSH ratios.
Immune Support
Immunologic factors affecting fertility are prevalent. Most cases result in recurrent spontaneous miscarriage; however, in some cases immunologic concerns prevent conception. The development of antisperm antibodies is one such circumstance. In study of 1020 female patients with primary or secondary infertility, serum antisperm antibody, antiovarian antibody, antiendometrial antibody, and anti-hCG antibody levels were tested. Patients were treated with dexamethasone, vitamin E, and vitamin C for three cycles consecutively as one course. After one course of treatment with corticosteroids, the disappearance rates of the antibodies mentioned were over 90%, and the average pregnancy rate was up to 30%. Corticosteroid use is associated with significant side effects.8 Herbs can be used either as an alternative first-line therapy or concurrently. An example of herb–drug synergy was seen when Glycyrrhiza glabra and cortisone ere successfully used together to minimize the dose dependence of the corticosteroid drug.9 Glycyrrhiza glabra has a cortisol-sparing action, as well as anti-inflammatory and adrenal restorative actions. It is contraindicated in hypertension, and steroid doses need to be modulated.
Echinacea is a well-known traditional immune-enhancing herb. It was widely used by Native Americans and then adopted by the Eclectic physicians for general immune support and infections. It is beneficial in the preconception stage of an infertility protocol to help immune surveillance. Echinacea can be aptly described as an immune modulator, assisting in enhanced phagocytosis and immune recognition. This may just be the key factor needed to regulate or prevent the onset of an autoimmune issue preventing conception or continued pregnancy. This action of echinacea is thought to be as a result of the presence of alkyl amides within the Echinacea root.19
Albizzia is a traditional Ayurvedic herb with antiallergenic properties. It has been shown to stabilize mast cells, reducing levels of allergy-inducing antibodies.20 Although not phytochemically well defined, albizzia is a useful herb to support women who are producing antisperm antibodies.
NUTRITIONAL CONSIDERATIONS
Between 1990 and 1993, Foresight, a British medical association for the promotion of preconception, conducted a study using a nutritional and lifestyle modification preconception care program. The results were nothing less than remarkable. There was a tenfold reduction in the expected incidence of miscarriage and birth defects and over 80% success rate with unexplained infertility. It was evaluated that before the study was started, 60% of the women drank alcohol regularly and 57% of the women involved were previously smokers. Out of the 367 couples in the study, 327 (89%) of them successfully became pregnant and 327 children were born. All of these babies were born healthy. Among the 204 couples with infertility problems, 175 (86%) were able to achieve a healthy pregnancy.21 One of the most significant aspects of these results was the involvement of both partners in the program—both female and male factors were concurrently addressed. In addition to nutritional supplementation, the study included lifestyle and social modifications, including the cessation of smoking, and coffee and alcohol consumption. Smoking cigarettes and coffee consumption have been linked to subfertility and delayed conception. 22 23 24 Based on the Foresight study, the suggested preconception care nutritional program is outlined in Table 12-3.21
| NUTRIENT | DAILY DOSE |
|---|---|
| Beta carotene | 6 mg |
| Vitamin E | 500 IU |
| Vitamin D | 200 IU |
| B1, B2, B3, B5 | 50 mg each |
| B12 | 400 μg |
| B6 | Up to 250 mg |
| Biotin | 200 μg |
| Choline | 25 mg |
| Inositol | 25 mg |
| PABA | 25 mg |
| Folic acid | 500 mg |
| Vitamin C | 2000–3000 mg |
| Bioflavonoid | 300 mg |
| Calcium | 800 mg |
| Magnesium | 400 mg |
| Potassium | 15 mg |
| Iron | 15 mg |
| Iodine | 75 μg |
| Selenium | 100–200 μg |
| Zinc | 20–60 mg |
| Chromium | 100–200 μg |
| Omega-3 essential fatty acids (as Evening primrose oil) | 500–1000 mg |
| Omega-6 essential fatty acids (as fish oil or flaxseed oil) | 500–1000 mg |
ADDITIONAL THERAPIES
Stress Management and the Mind–Body Approach
There is a direct relationship between fertility and stress is as much an endocrine experience as an emotional reality. The human body has extensive hormonal responses to the environment, especially stress, which occur at the hypothalamic and pituitary levels. The anterior pituitary is responsible for regulation of the female menstrual cycle. In response to stress, the adrenals release the hormone cortisol, known to adversely affect the menstrual cycle. The effects of stress are mostly associated with long menstrual cycles and delayed ovulation. Stress and elevated cortisol have also been linked to elevated prolactin levels. Stress management strategies should include lifestyle modifications, including exercise, yoga, and emotional release techniques. Physiologically, the hypothalamic pituitary adrenal (HPA) axis can be supported with adrenal tonic herbs such as licorice and rehmannia, in combination with adaptogenic herbs such as eleuthero (Eleutherococcus senticosus) and ashwagandha. These herbs act to regulate the HPA axis and assist in general adaptation syndrome. There is also increasing evidence that a behavioral approach might be effective in infertility treatment. A study of 54 women who completed a behavioral treatment program based on ability to elicit a relaxation response demonstrated decreased anxiety, depression, and fatigue. Additionally, 34% of the women became pregnant within months of completing the program. Behavioral therapy should be considered as therapy itself, or in conjunction with other treatments, including ART.25
Addressing Environmental and Occupational Toxicity Associated with Infertility
Formulas for Infertility: Various Associated Contributing Factors
Estrogen Balancing and Ovarian Tonic Formula (for follicular phase problems)
| Chaste berry | (Vitex agnus-castus) | 30 mL |
| Shatavari | (Asparagus racemosa) | 30 mL |
| Schisandra | (Schisandra chinensis) | 20 mL |
| Black cohosh | (Actaea racemosa) | 10 mL |
| Wild yam | (Dioscorea villosa) | 10 mL |
| Total: 100 mL | ||
Luteal Insufficiency Formula
| White peony | (Paeonia lactiflora) | 50 mL |
| Chaste berry | (Vitex agnus-castus) | 15 mL |
| Licorice | (Glycyrrhiza glabra) | 25 mL |
| Blue cohosh | (Caulophyllum thalictroides) | 10 mL |
| Total: 100 mL | ||
Formula for Hyperprolactinemia
| White peony | (Paeonia lactiflora) | 25 mL |
| Ashwagandha | (Withania somnifera) | 25 mL |
| Gymnema | (Gymnema sylvestris) | 15 mL |
| Chaste berry | (Vitex agnus-castus) | 12.5 mL |
| Licorice | (Glycyrrhiza glabra) | 12.5 mL |
| Total: 100 mL | ||
Formula for Elevated LH
| White peony | (Paeonia lactiflora) | 65 mL |
| Black cohosh | (Actaea racemosa) | 35 mL |
| Total: 100 mL | ||
Formula for Low LH
| Tribulus* | (Tribulus terrestris) | 60 mL |
| Chaste berry | (Vitex agnus-castus) | 40 mL |
| Total: 100 mL | ||
Formula for Elevated FSH
| Tribulus | (Tribulus terrestris) | 80 mL |
| Shatavari | (Asparagus racemosus) | 10 mL |
| Chaste berry | (Vitex agnus-castus) | 5 mL |
| Wild yam | (Dioscorea villosa) | 5 mL |
| Total: 100 mL | ||
Formula for Elevated Testosterone/Androgens
| Tribulus* | (Tribulus terrestris) | 75 mL |
| Schisandra | (Schisandra chinensis) | 10 mL |
| White peony | (Paeonia lactiflora) | 10 mL |
| Licorice | (Glycyrrhiza glabra) | 5 mL |
| Total: 100 mL | ||
Formula for Pelvic Factors/Uterine Tonic
| White peony | (Paeonia lactiflora) | 25 mL |
| Shatavari | (Asparagus racemosus) | 25 mL |
| Saw palmetto | (Serenoa repens) | 20 mL |
| False unicorn | (Chamaelirium luteum) | 15 mL |
| Goldenseal | (Hydrastis canadensis) | 15 mL |
| Total: 100 mL | ||
Formula for Cervical Factors (sperm antibodies, mucous membrane integrity)
| Rehmannia | (Rehmannia glutinosa) | 25 mL |
| Echinacea | (Echinacea spp.) | 25 mL |
| Wild yam | (Dioscorea villosa) | 20 mL |
| Saw palmetto | (Serenoa repens) | |
| Total: 100 mL | ||
toxins linked to infertility include heavy metals, pesticides, environmental estrogens, volatile organic solvents, and radiation.26,27 Heavy metals most often linked to subfertility are lead, mercury, and cadmium.26,28
One study examined the association between occupational chemicals and radiation exposure in 281 infertile women compared with 216 fertile women. The study concluded there was an increased risk of infertility among women exposed to volatile organic solvents, chemical dust, pesticides, and video display terminals (radiation). The women exposed to volatile organic solvent and chemical dust had an increased incidence of ovulatory problems. Tubal factors and endometriosis were associated with solvents and chemical dusts. Endometriosis and cervical factor infertility were associated with exposure to video display terminals (radiation).29
Environmental contamination is widespread; therefore, exposure to toxins is virtually ubiquitous. Research suggests the involvement of oxidative stress and electron transfer as the underlying causes of drastic health concerns such as infertility. The treatment framework should include multifaceted preventative measures, such as botanical and nutritional antioxidant therapy and liver support.30 Herbal therapy with a focus on liver support and improvement of phase 1 and 2 liver detoxification are helpful in the preconception period and during the infertility treatment to aid effective conjugation of sex hormones and toxins. Herbs such as Silybum marianum, Schisandra chinensis, Picrorrhiza kurroa, and Burpleurum falcatum have demonstrated hepatoprotective and hepatorestorative activity and assist with improvement of liver function and the detoxification processes in the body.31 To protect against the damaging effects of radiation exposure, foods and herbs rich in antioxidants have been shown to protect and regulate gene activity. Herbs that exhibit antioxidant activity include Ginkgo biloba, Vitis vinifera, Silybum marianum, Rosmarinus officinalis, Camellia sinensis, and Curcuma longa.
Acupuncture and TCM
Acupuncture can be considered for women suffering from infertility and has been shown to be of benefit in those with luteal phase defects. In TCM, the diagnosis of kidney insufficiency is said to relate to luteal phase defects. Using acupuncture to regulate the kidney may help regulate the hypothalamus pituitary ovarian axis.32,33
A young couple had been trying to conceive for 28 months before seeking holistic therapy. They had been through one failed IVF attempt 6 months earlier, which motivated them to explore other options. The female was 30 years old, and from medical evaluation, the fertility complications resulted from female factors. The menstrual history has been normal with menarche at age 14 and a regular 34-day cycle. She was aware of texture changes to her cervical mucus and noted that she experienced fertile mucus on days 16 or 17 of the cycle each month and experienced cramps on the first day of her menses. Her general medical history included anxiety, depression, insomnia, and hypoglycemia.
Treatment Protocol
| Black cohosh | (Actaea racemosa) | 15 mL |
| Ginger | (Zingiber officinale) | 15 mL |
| White peony | (Paeonia lactiflora) | 15 mL |
| Chaste berry | (Vitex agnus-castus) | 15 mL |
| Goldenseal | (Hydrastis canadensis) | 15 mL |
| Rehmannia | (Rehmannia glutinosa) | 10 mL |
| Albizzia | (Albizzia lubbock) | 15 mL |
| Total: 100 mL |