Femur and Hip
Perspective
Ancient Egyptian and Greek drawings depict persons with hip deformities ambulating with assistive crutches. The first available written description of a hip fracture was by the 16th-century French surgeon Ambroise Paré.1 In 1850, von Langenbeck was the first to attempt repair of a hip fracture with a nail for internal fixation. Later, Davis used ordinary wood screws in an attempt to aid the healing of femoral neck fractures.2 With the advent of radiography in the 19th century, the types of fractures and dislocations became easily identifiable, thus allowing discussion and investigation of management strategies, classification systems, and prognosis.
Epidemiology
Approximately 10 million adults in the United States have osteoporosis, and an additional 33.6 million have low bone density of the hip, both of which predispose to hip fracture.3 The annual incidence of hip fracture continues to grow as our population ages. During the late 1990s, approximately 250,000 patients a year sought treatment in emergency departments (EDs) after sustaining hip fractures.4 In 2005 alone, this number exceeded 290,600 patients.5 It is estimated that this number will surpass half a million patients a year by 2025.5 Although hip fractures represent only 14% of all fractures in adults, they account for 72% of medical costs related to fractures.5 Femoral neck fractures have a female to male ratio of 4 : 1 and typically occur in elderly patients with osteoporosis.6 There is an increasing incidence of intertrochanteric fractures with advancing age, and women are affected six times more often than men.3,7 Overall, more than three quarters of all hip fractures occur in postmenopausal women older than 50 years.3
The elderly are not the only population affected by hip and femur pathology. Perthes’ disease—avascular necrosis (AVN) of the femoral head—occurs from 2 to 14 years of age, with a peak age of onset of 5 years, and it is five times more common in boys than in girls.8 Slipped capital femoral epiphysis (SCFE) peaks at 13.5 years of age among boys and 12 years among girls, in association with the onset of puberty, and is nearly twice as common in boys.9
Principles of Disease
Skeletal Anatomy
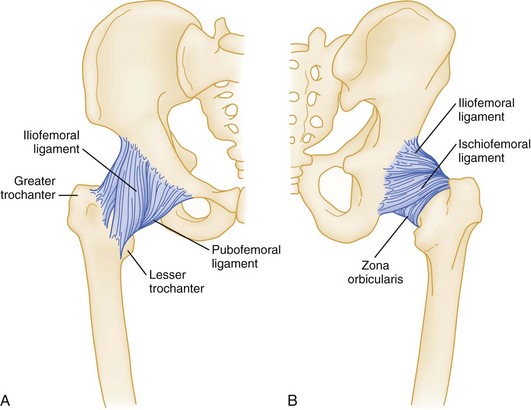
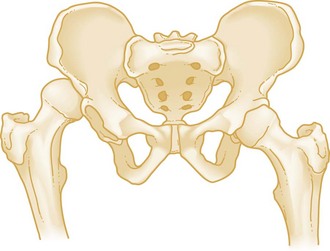
The femoral head is firmly seated in the acetabulum, which is reinforced by labral cartilage. The well-developed capsule, overlying ligaments, and proximal musculature of the lower extremity add strength to the joint (Fig. 56-1). The nearly spherical femoral head articulates with the acetabular cup in a variation of the ball-and-socket joint.
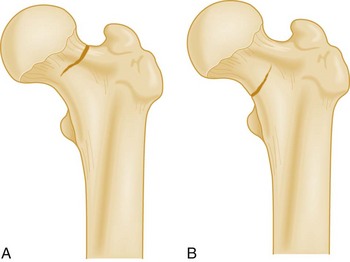
The femur is the longest and strongest bone in the human body and is routinely subjected to substantial forces produced during powerful muscle contraction and weight transmission. In an anatomic position, the two femurs extend obliquely from the pelvis medially to the knee and bring the legs closer to the midline, where they can best support the body. Structurally, the femoral neck serves as an oblique strut between the pelvis (the horizontal beam) and the shaft of the femur (the vertical beam) (Fig. 56-2). The length, angle, and narrow circumference of the femoral neck permit substantial range of motion at the hip, but these same characteristics subject the neck to incredible shearing forces. A fracture results when these forces exceed the strength of the bone. As drawn on an anteroposterior (AP) radiograph, the intertrochanteric line, an oblique line connecting the greater and lesser trochanters, marks the junction of the femoral neck and its shaft.
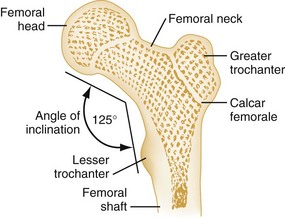
Figure 56-2 Bony architecture of proximal end of the femur.
Musculature
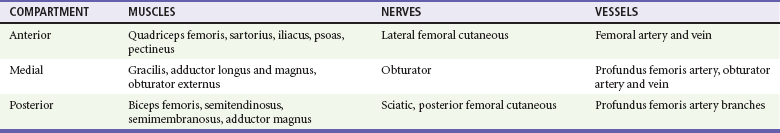
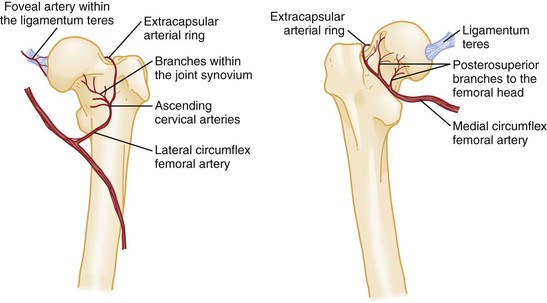
The musculature of the hip and thigh is the largest and most powerful in the human body. The muscles in this region of the body are located within three different compartments, each containing associated nerves and vessels (Table 56-1). The muscles also are grouped according to their primary action at the hip. Knowledge of the major muscle actions offers insight into the injury patterns and deformities commonly seen (Fig. 56-3).
Vascular Anatomy
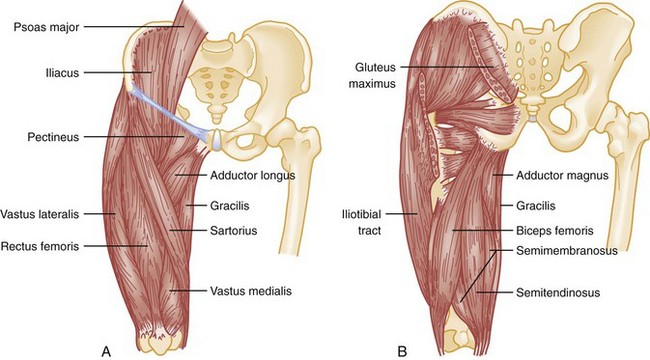
The arterial supply to the femoral head arises from two main sources (Fig. 56-4). The major source is the ascending cervical arteries as they branch off the extracapsular ring and run along the femoral neck beneath the synovium. Some blood is supplied to the femoral head from the second source, within the marrow spaces—the intraosseous cervical vessels. A third and minor source is the foveal artery, which lies within the ligamentum teres.
As the external iliac artery passes beneath the inguinal ligament, it becomes the common femoral artery.10 At this point the artery is located midway between the anterior superior iliac spine (ASIS) and the symphysis pubis. Approximately 3 to 4 cm distal to the inguinal ligament, the common femoral artery branches to form the superficial and deep femoral arteries. The larger superficial femoral artery passes along the anteromedial aspect of the thigh and terminates at the junction of the middle third and lower third of the thigh. Here, the superficial femoral artery passes through the adductor hiatus and becomes the popliteal artery. The deep femoral artery runs posterolaterally to the superficial femoral artery, supplies the hamstrings, and terminates in the distal third of the thigh as small branches piercing the belly of the adductor magnus. These perforating branches constitute an additional site of potential injury. The abundant muscle coverage and blood supply of the thigh aid in healing fractures of the femoral shaft.
Venous System
In the proximal two thirds of the thigh, the common and superficial femoral veins lie adjacent to the common and superficial femoral arteries. At the inguinal ligament, the common femoral vein is posterior and medial to the common femoral artery and moves to the lateral position as it passes distally. The deep femoral vein and the greater saphenous vein are the two main tributaries to the common and superficial femoral veins. The deep femoral vein and artery run in parallel as the vein joins the superficial femoral vein just distal to the inguinal ligament. The greater saphenous vein arises in the dorsum of the foot and ascends anterior to the medial malleolus. This vein is relatively superficial as it passes up the medial aspect of the leg to join the common femoral vein distal to the inguinal ligament.10
Nerves
The femoral and sciatic nerves are the major nerves within the thigh. The femoral nerve is the largest branch of the lumbar plexus; it passes under the inguinal ligament lateral to the femoral artery and divides into anterior and posterior branches soon after entering the thigh. The sensory divisions of the anterior branch, the intermediate and medial cutaneous nerves, supply sensation to the anteromedial aspect of the thigh. The motor division of the anterior branch innervates the pectineus and sartorius muscles. The posterior femoral branch gives off the saphenous nerve, which supplies sensation to the skin along the medial aspect of the lower part of the leg. The posterior branch also supplies motor function to the muscles of the quadriceps femoris group.10
The sciatic nerve is the largest peripheral nerve in the body. It arises from the sacral plexus. The sciatic nerve exits the pelvis through the greater sciatic foramen and travels through the posterior thigh; it extends from the inferior border of the piriformis to the distal third of the thigh. The sciatic nerve gives off articular branches that supply the hip joint. In the thigh, muscular branches innervate the adductor magnus and hamstring muscles. Just proximal to the popliteal fossa, the sciatic nerve divides to form the tibial and common peroneal nerves.10
Pathophysiology
Osteoporosis of the Femur
Osteoporosis is the leading cause of hip fracture. Osteoporosis currently affects more than 10 million people in the United States and is projected to affect approximately 14 million adults older than 50 years by the year 2020. The number of hip fractures attributable to osteoporosis is expected to be 6.3 million by the year 2050, although the incidence in women has been decreasing in recent years, probably because of an increased awareness and more aggressive treatment of osteoporosis.3,11 Hip fractures can have a devastating impact. One in five patients dies during the first year after a hip fracture, mostly from causes other than the fracture itself; one third require nursing home placement after hospital discharge; and less than one third regain their prefracture level of physical function.12 The economic impact of these fractures is enormous.
The pathophysiology of osteoporosis is not completely understood, but strong associations with hormonal changes related to aging, genetic predisposition, vitamin D deficiency, lack of physical activity, and smoking have been recognized.13 Severe osteoporosis and hip fractures are most common in elderly white women; however, a decrease in bone density after age 30 is seen across all demographic groups. Radiography of the head of the femur can quantify the degree of osteoporosis, even in the nonfractured hip. The trabeculae of the femoral head and neck strengthen the bone and support the large mechanical forces produced across the hip joint. As osteoporosis begins and then progresses, these trabeculae disappear. This loss of trabeculae weakens the bone and increases the risk of fracture.
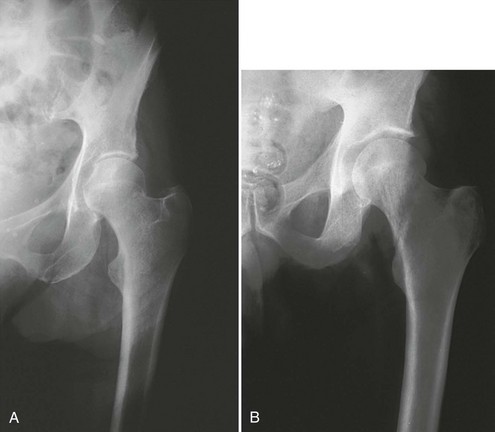
Osteoarthritis of the Hip
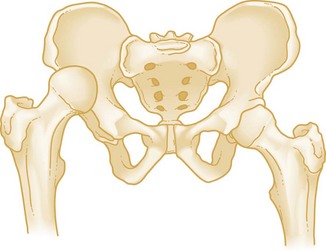
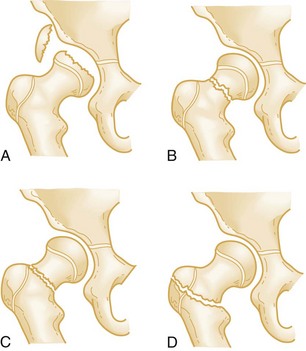
As the population ages, a greater percentage of the population will develop chronic pain from degenerative osteoarthritis of the hip. Overall, osteoarthritis ranks fifth in health impact (measured in years lost to disability) in high-income countries and ninth in low- and middle-income countries.14 Disability often results from persistent pain and limited physical mobility. The progression of osteoarthritis can be demonstrated with serial radiographs of the affected hip (Fig. 56-5); however, radiographic findings do not necessarily correlate with symptoms.15
Avascular Necrosis
When a patient has an increasingly painful hip, buttock, thigh, or knee and no history of recent trauma, AVN of the femoral head should be considered. AVN has been referred to as aseptic necrosis, ischemic necrosis, and osteonecrosis. It is the result of ischemic bone death of the femoral head after compromise of its blood supply (Fig. 56-6). AVN is bilateral in 40 to 80% of patients. It is common in relatively young patients, the mean age at diagnosis being 38 years.16 Although a specific causative disorder is not identified in 20% of the cases, known atraumatic causes include chronic corticosteroid therapy, chronic alcoholism, hemoglobinopathy (e.g., sickle cell anemia), dysbarism, and chronic pancreatitis.16,17 AVN also is an emerging complication associated with human immunodeficiency virus (HIV) infection. It is unclear whether the virus itself or the treatments are the pathogenic agents.17
Traumatic AVN is a subacute manifestation after hip dislocation or femoral neck fracture. It is a direct result of disruption of the blood supply to the femoral head. It is more common in males and African Americans. The incidence of AVN as a subacute complication is clearly related to both the initial degree of trauma and the amount of time the femoral head remains out of joint. Reduction of the hip within 6 hours after dislocation significantly decreases the incidence of AVN.18 Multiple studies have shown that there is relationship between the length of time the hip is dislocated and the rates of AVN, with as few as 4.8% of patients developing AVN with reduction within 6 hours, and as many as 58.8% developing AVN with reduction after more than 12 hours. For this reason, hip dislocation should be considered an orthopedic emergency. The emergency physician should perform reduction of the hip if there is any delay in orthopedic consultation.
Even with optimal treatment, femoral neck fractures are complicated by AVN in 11 to 19% of cases. For all practical purposes, femoral neck fractures are effectively intra-articular fractures. Acutely, bleeding from the fracture site may cause high intracapsular pressure and a tamponade effect on the femoral head, thereby further impairing the blood supply to it.19 In addition, if the bone fragments are not impacted, synovial fluid will lyse the blood clot. Such lysis prevents the development of capillary buds and the scaffolding needed for osseous repair. These factors all contribute to make AVN of the femoral head a common complication. Conversely, intertrochanteric and subtrochanteric fractures are located in an area of rich blood supply provided by an extracapsular arterial supply. AVN rarely complicates these fractures.
Myositis Ossificans
Myositis ossificans (heterotrophic ossification) is pathologic bone formation at a site where bone is not normally found. Traumatic myositis ossificans results most commonly from a direct blow to muscle. The thigh and hip muscles are often involved. The incidence of myositis has been reported as up to 17% of patients undergoing medical evaluation of thigh contusions, and the condition is thought to be related to the severity of the injury.20–22 The incidence of myositis ossificans after hip surgery is approximately 2%, but these lesions are clinically significant in only 10 to 20% of cases.21 Increased susceptibility to myositis ossificans has been described in persons with hemophilia or other bleeding disorders in conjunction with soft tissue injury.21
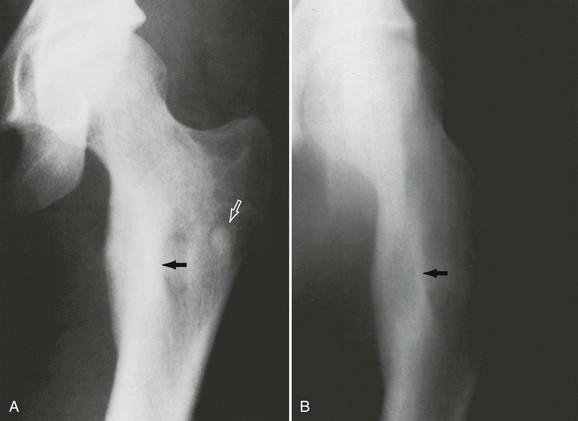
Radiographically, myositis ossificans appears as irregularly shaped masses of heterogeneous bone in the soft tissues around the joint or along fascial planes (Fig. 56-7). It may be seen as early as 10 to 21 days after injury, but radiographic evidence typically lags behind onset of symptoms by weeks.20 Its appearance may simulate primary bone neoplasm, especially when the periosteum is involved. Osteosarcoma and periosteal osteogenic sarcoma should be considered in the differential diagnosis. Computed tomography (CT) scan can sometimes be helpful in distinguishing between neoplasm and myositis ossificans, as the lesions of myositis ossificans begin to calcify at the periphery and progress toward the center, and those of osteosarcoma begin to calcify at the center first. Orthopedic follow-up should be arranged for these patients.
Initial treatment of contusions is aimed at preventing myositis ossificans by use of the RICE principle of rest, ice, compression, and elevation. Immobilization of the extremity may prevent retraction of ruptured muscle and increasing size of hematoma formation but should be limited to less than 48 hours. Once a stable scar has formed, range of motion within limits of pain should be initiated. If myositis ossificans has already formed, the mainstay of treatment is supportive with rest, slow return to normal activity, and physical therapy. Although indomethacin is commonly used to prevent heterotopic ossification after surgery, it has not been validated for the prevention as well as the treatment of myositis ossificans.20,21 Its use based on the principle of inhibition of bone formation does not seem to be contraindicated.20 Operative removal of a mature lesion may be indicated if the lesion is near a joint or is causing permanent impairment or pain.
Calcific Bursitis and Calcifying Peritendinitis
Calcification surrounding tendons and bursae or occurring in the joint capsule is referred to as calcific bursitis or calcifying peritendinitis. The cause of these lesions is unknown. No relationship has been documented between the radiographic findings and acute symptoms. Calcific bursitis of the hip is uncommon, but when it does occur, it most frequently affects the trochanteric bursa (Fig. 56-8). Other possible affected areas include gluteal muscles and the hip flexors and adductors. The bursal calcification is seen on radiographs as an amorphous, poorly marginated line that is clearly separate from the cortex of the femur. Treatment should focus on stretching and strengthening of the hip.
Neoplastic Disease in the Hip
The most common neoplastic disease of bone is metastatic, generally from breast, kidney, lung, thyroid, or prostate tumors. Primary bone lesions also occur, with the most common being osteoid osteoma (Fig. 56-9). Bone lesions may be osteoblastic or osteolytic. Patients may come to the ED with significant bone pain or a large bothersome mass, such as a solitary osteochondroma (Fig. 56-10). Neoplasms place the patient at higher risk for pathologic fracture, especially if the lesions are large or lytic or have eroded the cortex.
Clinical Features
Age and gender are predisposing factors for certain injuries. A detailed description of any antecedent trauma or other precipitating events is often helpful. With trauma, details of the mechanism of injury may aid in predicting injury patterns. With stress fractures, an alteration in physical activity or exercise routine provides a clue to the diagnosis. Systemic illnesses or known metabolic disorders should be noted. Previous cancer, irradiation, and chemotherapy are clues to pathologic fractures. Any past steroid use, including inhaled steroids, is important to identify because it predisposes patients to AVN of the femoral head. A linear relationship has been recognized between the cumulative steroid dose and the incidence and severity of osteoporosis and hip fracture.23
Ascertainment of the location of the patient’s pain is paramount; true hip joint pain is often groin pain. However, pediatric patients with hip pathology often have knee pain as the sole presenting complaint. A review of systems should include information that may help in ascertaining hip or femur pathology versus another cause. Atypical pain may be the result of nephrolithiasis, pelvic inflammation, infection or tumor, inguinal and femoral hernia, or adenopathy from genital or cutaneous infection. A history of low back pain may suggest radiculopathy as the cause of the patient’s pain. A differential diagnosis of hip pain without obvious fracture on radiographs is listed in Box 56-1.
The history should also focus on comorbid conditions and injuries. Elderly patients with a hip fracture sustained in a fall at home may be unable to summon help for hours to days. They often have severe dehydration, electrolyte abnormalities, rhabdomyolysis, and renal insufficiency and require a thorough evaluation of these metabolic parameters before surgery is considered.24 In addition, the reason for the fall should be determined, as it may reveal other comorbid conditions (e.g., syncope, cardiac dysrhythmias, polypharmacy, alcoholism). Sedative or antihypertensive medications predispose elderly patients to falling and should be prescribed carefully. In a fall, elderly patients may have sustained additional injuries; most commonly, these injuries involve fracture of a vertebral body or wrist. Cervical spine and intracranial injuries also are considered. Young patients with a hip fracture resulting from high-energy mechanisms have concomitant injuries in 40 to 75% of cases.18
Physical Examination
Systematic examination of the injured extremity will reveal any focal tenderness or warmth that may indicate injury or infection. Active and passive range of motion, and muscle strength, though offering important information, are frequently limited by pain. Detailed neurovascular assessment is vital. Femoral nerve and arterial injury often occur with subtrochanteric and femoral shaft fractures or anterior hip dislocation. The sciatic nerve can be injured with a hip fracture or posterior hip dislocation. Neurologic examination includes evaluation of light touch and pinprick sensation. Femoral, popliteal, dorsalis pedis, and posterior tibial pulses are assessed. Comparative blood pressures obtained by Doppler examination in the injured and uninjured extremities (arterial pressure index) may be useful in diagnosing occult femoral arterial injuries. If the systolic pressure in the affected extremity is 90% or less (ratio less than 0.9) than that in the unaffected extremity, additional diagnostic studies should be undertaken. Additional diagnostic studies include Doppler flow ultrasound imaging, CT angiography, or angiography alone. The ankle-brachial index (ABI) also can be similarly determined by comparing the systolic pressures of the affected extremity and of the ipsilateral arm. An index less than 0.9 necessitates further diagnostic studies.25,26
Diagnostic Strategies
Radiographic Anatomy and Evaluation
Normal radiographic and skeletal anatomy is familiar to emergency physicians (Fig. 56-11).
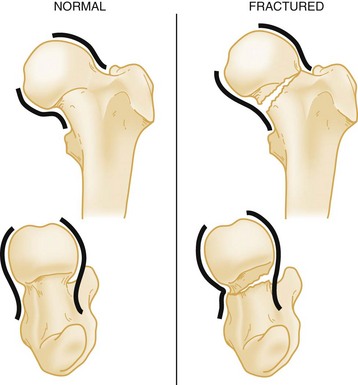
True AP and lateral radiographs of the femur are usually adequate for the evaluation of potential fractures. The femur should be in as much internal rotation as possible. Fracture lines may be very subtle, particularly with femoral neck fractures. Experts have found three methods useful for identifying inconspicuous fractures. The use of Shenton’s line is described in a subsequent section on hip dislocations. (A second method is illustrated in Fig. 56-15.) In searching for a fracture of the femoral neck, both the medial and lateral cortical margins of the femoral head and neck should be carefully examined for the normal S and reverse S curves seen on radiographs of nonfractured hips. The convex outline of a normal femoral head smoothly joins the concave outline of the femoral neck when in anatomic position. This produces an S curve and a reverse S curve, regardless of the orientation of the radiographic projection. A fracture produces a tangential or sharp angle, indicative of disruption of the normal anatomic relationship. A third method, useful in the evaluation of seemingly unremarkable hip radiographs, is to trace the trabecular lines as they pass from the femoral shaft to the femoral head. These lines will be disrupted as they pass through the fracture site, and such disruption often provides the only, albeit subtle, clue. If a fracture is found, radiographs of the knee should be obtained as well. It is a basic orthopedic principle to image the joint above and below any fracture.25
One common inaccuracy in hip radiography merits clarification: The soft tissue linear radiolucencies superolateral and inferomedial to the femoral head and neck do not represent the hip capsule, as is commonly believed. Instead, they represent the fat within the fascial plane covering the gluteus minimus superiorly and the tendon of the iliopsoas muscle inferiorly.27 Comparison of these lines on the symptomatic side with those on the unaffected side should not be used to determine whether an effusion of the hip is present.
Occult Hip Fracture
If radiographs do not show a fracture, or suggestion of injury, ambulation may be attempted. Inability to ambulate or difficulty in ambulation heightens the suspicion of occult fracture. Approximately 2 to 10% of all hip fractures are radiographically “occult” on plain films.28 Failure to detect these injuries results in increased mortality, risk of subsequent displacement of the fracture, and a higher incidence of AVN.29,30 When a painful hip prevents ambulation and plain radiographs do not reveal a fracture, magnetic resonance imaging (MRI) should be performed.28,29 In addition, elderly patients with unexplained chronic hip pain for more than 3 weeks may harbor an occult fracture even if they continue to ambulate. T1-weighted MRI will reveal a fracture that was imperceptible at the time of injury with 100% accuracy and has been found to be cost-effective when compared with other strategies.29 A small study comparing CT scans with MRI in the diagnosis of occult hip fractures revealed a 66% misdiagnosis rate for CT scans.29 MRI remains the “gold standard” modality for diagnosing occult hip fractures and helps determine the treatment of these fractures (Fig. 56-12).
Management
Patients with traumatic fracture of the hip or femur should have blood typed and crossmatched for at least 2 units of blood. The potential for significant blood loss and the multiple common associated injuries constitute important justification for this recommendation. Hemodynamic instability may result from dehydration and blood loss of up to 3 units into the fracture site. Currently, treatment of these fractures is hemiarthroplasty or open reduction and internal fixation for femoral neck fractures. Internal fixation with a sliding compression screw generally is used to treat intertrochanteric fractures. The goal is to promote immediate postoperative mobilization. It has become widely accepted that the risks of surgery in elderly patients are minimal when compared with the risks of prolonged bed rest, deep vein thrombosis, pulmonary embolism, pneumonia, and urosepsis from an indwelling Foley catheter. If possible, the repair is conducted with use of spinal anesthesia to decrease the operative risk. Operative repair should be performed after the patient is resuscitated and is in optimal preoperative condition. Care of an elderly patient with a hip fracture requires a multidisciplinary approach and often involves coordination of the efforts of the emergency physician, orthopedist, internist, neurologist, and cardiologist to stabilize the patient before surgery. Comprehensive hip fracture programs for the elderly that include comanagement by geriatricians and orthopedic surgeons have been shown to improve short-term outcomes and may even lower mortality, highlighting the importance of medical management of these complex patients.31,32
Traction and Immobilization
Contraindications to the use of traction splints include pelvic fractures, patellar fractures, ligamentous knee injuries, and tibia or fibula fractures. Traction in the prehospital setting should not be applied to any open fracture that has exposed bone. Such reduction pulls grossly contaminated bone fragments back into the wound before adequate débridement can be undertaken in the operating room. A study that evaluated patients with multisystem trauma in whom traction splints were placed in the field for femur fractures showed that up to 38% of the cases had contraindications to the splints that were placed.33
With or without traction, the injured extremity should be immobilized when the patient is moved, to prevent further damage from mobile bone fragments. This can be done with simple splinting in the prehospital setting. In the ED, maintaining the leg in slight flexion at the hip reduces intracapsular pressure, whereas extension of the leg increases pressure and potential for ischemic necrosis of the femoral head. Therefore traction for proximal femur fractures may be discontinued once the patient has arrived in the ED. The leg may be supported in a position of comfort with a pillow placed under the thigh. The theoretic advantages for continuation of traction in the ED are pain control and fracture reduction, making operations easier to perform. This is likely true in femoral shaft fractures; however, a Cochrane systematic review looking at preoperative traction for fractures of the proximal femur in adults found no evidence to support these proposed advantages.34
Open Fracture Care
By definition, an open fracture is any fracture in which a break in the integrity of the skin and soft tissue allows communication with the fracture and its hematoma. Any nearby wound or break in the skin must be considered to communicate with the fracture. Open fractures are divided into three categories (Table 56-2). A bone piercing from the inside outward often causes only a small wound. The contaminated bone tip may then slip deceptively back into the soft tissue; therefore any break in the integrity of the skin makes the fracture an open one. Open wounds should be irrigated and then covered with sterile saline-moistened gauze.
Table 56-2
Classification of Open Fractures
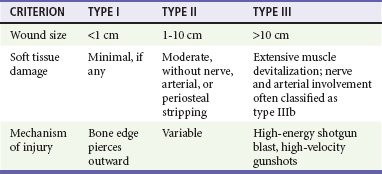
From Hoff WS, Bonadies JA, Cachecho R, Dorlac W: East Practice Management Guidelines Work Group: update to practice management guidelines for prophylactic antibiotic use in open fractures. J Trauma 70:751-754, 2011.
For all type I open fractures, a first-generation cephalosporin should be administered intravenously. Types II and III may require additional gram-negative coverage because of the amount of devitalized tissue and increased gram-negative skin flora found in the groin.35 This additional coverage could be provided by an aminoglycoside such as gentamicin or tobramycin. The use of perioperative first-generation cephalosporins has been shown to reduce postoperative infection even in closed fractures in patients who are to undergo surgery.35
Compartment Syndrome
Because of the thigh’s larger volume, compartment syndrome within the thigh is far less common than in the lower part of the leg. A large amount of bleeding into the compartment is required before the pressure rises above capillary perfusion pressure. When compartment syndrome does occur in the thigh, only 50% of the cases are associated with a femur fracture.36 It is difficult to clinically differentiate the expected swelling after an injury from early compartment syndrome. Clinical examination and the use of direct compartment pressure measurements can detect the development of compartment syndrome at an early stage.
Pain Management
It is well known that control of pain in EDs is often inadequate.37 In the case of femoral fractures, narcotic analgesia is often indicated in combination with other pain-relief strategies including immobilization of the injured extremity, placement of the injured extremity in a position of comfort, and the consideration of local analgesia in the form of nerve blocks.
Femoral Nerve Block
Femoral nerve blocks have been used to treat femoral shaft fractures for more than 50 years. Despite proven effectiveness and a low complication rate, this technique has not been widely embraced by emergency physicians or surgeons.38 The femoral nerve block is an excellent option as an adjunct or alternative to systemic analgesics in patients at risk for hypotension. It has been shown to significantly decrease time to lowest pain score as compared with intravenous narcotics, and patients have been found to require significantly lower doses of narcotics in conjunction with femoral nerve blocks.38,39 The block can be performed with the assistance of a peripheral nerve stimulator to localize the nerve, or bedside ultrasound to directly visualize the nerve before anesthetic injection.40 Femoral nerve blocks have been shown to be effective when performed by newly trained emergency physicians without the assistance of peripheral nerve stimulators or ultrasound.39 If a long-acting anesthetic such as bupivacaine is used, the expected onset of analgesia is within 30 minutes, and its duration is 6 to 8 hours.41
Hip Arthroplasty
Sir John Charnley first described the modern form of total hip arthroplasty (THA) in 1961. Despite many changes in both the design and materials used, Charnley’s essential design has been established as the standard.42 The number of THA procedures performed annually in the United States rose from 65,000 in 1982 to more than 230,000 in 2007.43 The most common indication for THA is joint failure resulting from severe osteoarthritis. Other indications include rheumatoid arthritis, certain types of hip fracture, AVN, and certain tumors. Arthritis associated with Paget’s disease, trauma, ankylosing spondylitis, and juvenile rheumatoid arthritis are also relative indications for THA or partial hip arthroplasty.
Outcomes and Complications
THA provides an immediate, substantial reduction of pain and improvement in functional ability and overall quality of life. A 10-year follow-up study of patient outcomes, including gait, perception of pain, physical mobility, sleep patterns, and energy scores, showed positive results in more than 90% of cases.44 Despite the tremendous success of THA, numerous complications have been reported. Aseptic loosening of the prosthesis is the most common. Other complications include component wear, infection, adjacent femoral fractures, deep vein thrombosis, and postoperative dislocation of the femoral component. In general, flexion past 90 degrees, adduction, and internal rotation place the hip at risk for dislocation. This combination can occur when patients bend at the waist (e.g., to sit on a normal low toilet or to get out of a chair) or cross the legs45 (Fig. 56-13).
Specific Injury Patterns
Fractures of the Hip and Femur
Avulsion Fractures
The pain of avulsion injuries of the hip may manifest as referred pain to the thigh; these fractures are most common in adolescents and young adult athletes. The incidence of avulsion fractures is increasing as a result of the growth of competitive sports participation, especially in teenage athletes.46,47 The muscular origin of this type of injury commonly involves the pelvic apophyses, which may not fully ossify until age 25. Avulsion at the site of the growth plate is the result of sudden maximal muscular exertion. It may occur with rapid acceleration or sudden changes in speed or direction. The athlete classically experiences a sudden piercing pain at the site of injury, along with a “snapping” or “popping,” and frequently falls to the ground because of the intensity of this pain. As depicted in Figure 56-14, avulsion at the ASIS involves the separation of a thin piece of bone as the sartorius muscle suddenly contracts (see Fig. 56-14A). The anterior inferior iliac spine (AIIS) is avulsed by the rectus femoris, and the hamstring group may pull off the ischial tuberosity (see Fig. 56-14B). Avulsion fractures of the ASIS and AIIS are managed nonoperatively with conservative treatment. Treatment of avulsion fractures of the ischial tuberosity is more controversial. Most experts recommend conservative treatment for avulsion injuries with less than 2 cm of displacement. Fractures with more than 2 cm of displacement may benefit from operative fixation to prevent nonunion, as well as union with exuberant callus formation.47,48
Proximal Femoral Fractures
Classification Systems.: Fractures of the proximal end of the femur have been classified on the basis of their relationship to the hip capsule (e.g., intracapsular and extracapsular), anatomic location (neck, trochanteric, intertrochanteric, subtrochanteric, and shaft fractures), and degree of displacement. A working knowledge of the classification system will allow the emergency physician to communicate with the consulting orthopedist regarding the fracture’s pattern and stability and treatment options.
Femoral Neck Fractures
Pathophysiology.: Many experts now refer to femoral neck fractures as insufficiency fractures in acknowledgment of the major role played by osteoporosis. Age-related bone loss is believed to be the most important etiologic factor in femoral neck fractures.49 The theory that these fractures result from primary skeletal pathology is supported by the fact that minimal or no injury is associated with most of these fractures. Pathologic fractures from metastatic carcinoma are also well described.
Classification.: Although several classification systems were formerly used to describe these fractures, they have been abandoned because of poor inter-rater reliability and limited clinical utility. Currently, femoral neck fractures should be classified as either nondisplaced or displaced fractures.
From 15 to 20% of all femoral neck fractures are nondisplaced fractures. The fracture line often may be very subtle. Techniques described for detection of subtle fracture lines may be useful for this reason. Evaluation of the continuity of the subcapital cortical lines, search for an indistinct broad band of increased subcapital density, and identification of the S and reverse S curves (Fig. 56-15) will lead to the correct diagnosis in most cases. In impacted femoral neck fractures, the neck cortex is driven into the cancellous femoral head. Bone impaction lends a certain inherent stability (Fig. 56-16). Because of this inherent stability, two different management approaches have been advocated: early ambulation and internal fixation. Internal fixation has been associated with a reduced length of hospital stay and improved rehabilitation and has become the preferred treatment modality. Without impaction, a nondisplaced femoral neck fracture is unstable and will become displaced without internal fixation.
Outcome and Complications.: The mortality rate during the first year after a femoral neck fracture is 14%, as compared with 9% for the control population. Factors affecting mortality include age, male sex, psychiatric illness, end-stage renal disease, and congestive heart failure.50 Institutionalized patients have a death rate up to three times higher than noninstitutionalized patients.51 Complications can be minimized by early reduction, stable internal fixation, early ambulation, and close attention to medical comorbidities.
AVN and nonunion are the two major complications of femoral neck fractures. AVN is the most common complication, despite optimal treatment, because of the complex arterial anatomy. Deep infection in the form of osteomyelitis or septic arthritis is more common with femoral neck fractures because the fracture line extends into the joint. The rate of infection has been dramatically reduced with the use of perioperative antibiotics. Pulmonary embolism is another significant complication and is the leading cause of death 7 days after fracture in orthopedic patients. Anticoagulation is recommended for at least 10 days after any hip surgery in patients without significant contraindications. Fondaparinux has been shown to be an effective anticoagulant in this setting.52
Intertrochanteric Fractures
Anatomy.: The fracture line of intertrochanteric fractures extends between the greater and lesser trochanters of the femur. These injuries are considered to be extracapsular fractures. The fracture line extends through cancellous bone, which has an excellent blood supply. The hip’s short external rotators remain attached to the distal fracture fragment, and the internal rotators are attached to the proximal fracture fragment. Owing to the strong action of the iliopsoas muscle, the leg is shortened and externally rotated.
Pathophysiology.: An intertrochanteric fracture in younger adults usually is the result of high-speed collisions or high-energy trauma, such as falls from heights. An elderly person may sustain this injury during a fall from any height. The fracture lines are the result of both direct and indirect forces. The direct forces act along the axis of the femur and on the greater trochanter as it strikes the ground. Indirect forces are produced as the iliopsoas pulls the lesser trochanter and the abductors pull the greater trochanter; these forces often cause fractures at the site of insertion.
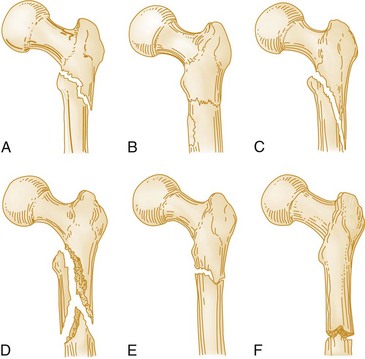
Classification.: A large number of classification systems for intertrochanteric fractures have been proposed to predict the possibility of achieving and maintaining stable reduction.53 A useful system designates the fracture according to the number of separate bone fragments produced (Fig. 56-17).
Management.: Intertrochanteric fractures carry particular management pitfalls for the emergency physician. Great care must be taken to maintain focus on the entire patient and not on the fracture alone. Hemodynamic instability may result from blood loss of up to 3 units into the fracture site.54 Poor nutrition before the fall, chronic diuretic use, and decreased oral intake in patients who have to wait until they are found will contribute to the level of dehydration. Up to 70% of these patients are under-resuscitated.24 Associated distal radius fractures, proximal humerus fractures, rib fractures, and compression fractures of the lumbar and thoracic spine often are overlooked because the femoral fracture distracts the attention of both patient and physician.
A substantial majority of intertrochanteric fractures will require some type of internal fixation. Such fixation allows rapid mobilization, decreased hospital length of stay, reduced mortality, and improved function.25 The procedure should be performed on an urgent rather than an emergent basis. Mortality is increased when the patient is taken to the operating room on the day of injury; however, early repair within 24 to 48 hours is associated with a 1-year mortality reduction.55 Preoperative medical optimization by multidisciplinary medical teams may decrease the incidence of 1-year mortality in these patients.32
Outcomes.: Intertrochanteric fractures have an associated mortality rate of 10 to 30% in the first year.32 Life expectancy returns to normal among patients who survive that year. Survival is most commonly related to the patient’s age and preexisting medical conditions. Additional risks associated with operative treatment include mechanical failure (1-16%), implant migration (2-10%), and infection (2-8%).56 Mechanical failure and nonunion are much more common in unstable fractures and those that were not adequately reduced. Approximately half of patients sustaining these fractures are eventually able to regain their original level of ambulation. Yearly infusion of zoledronic acid (a bisphosphonate) beginning within 90 days of hip fracture repair reduces the incidence of new fractures and decreases mortality.49,57
Isolated Fractures of the Greater or Lesser Trochanter
Fractures of the greater or lesser trochanter are rare. They occur in women more often than in men and are the result of a fall directly onto the trochanter or avulsion by the iliopsoas muscle. There may be a comminuted fracture involving only part of the greater trochanter or more subtle impaction of the lateral cortex. If avulsed, the fragments are displaced superiorly and posteriorly25 (Fig. 56-18).
Subtrochanteric Fractures
Anatomy and Pathophysiology.: Subtrochanteric fractures occur between the lesser trochanter and the proximal 5 cm of the femoral shaft. They may accompany intertrochanteric fractures. The subtrochanteric region is composed almost entirely of cortical bone, which lacks the vascularity important to new bone growth and repair. When fractured, it is more likely to be comminuted than bone with a higher cancellous content. In addition, the greater portion of the biomechanical forces of the femur is transmitted down the curved medial cortex of the femoral shaft. If this cortex is disrupted, the metal hardware undergoes the majority of the stress. This mechanism accounts for the increased incidence of hardware failure when the medial cortex is largely involved.
Epidemiology.: Subtrochanteric fractures account for 11% of all fractures of the proximal end of the femur. Although 10% of these fractures are caused by gunshots, the usual mechanism of injury is direct blunt trauma.58 A bimodal distribution for these injuries has been recognized. The first group consists of elderly patients who experience a fall, in whom the fracture occurs through an area of weakened cortical bone. Pathologic fractures from metastatic lesions, Paget’s disease, renal osteodystrophy, osteogenesis imperfecta, and osteomalacia are well-recognized clinical entities in these patients. The second group comprises victims of extreme high-energy trauma. In these patients, the subtrochanteric fracture is rarely an isolated injury because of the tremendous force required to produce it. Associated thoracic and abdominal injuries are common and should be aggressively sought to ensure adequate management. From 30 to 50% of patients with subtrochanteric fractures have associated fractures of the pelvis, spine, or other long bones. Stress fractures can occur in this region but are extremely uncommon.
Classification.: Various classification systems for these fractures have been proposed, although none is widely accepted.53 From a practical standpoint, it is best to define and describe these fractures by location (proximal or distal), angle (transverse, oblique), and the presence of comminution (Fig. 56-19).
Management.: Hemodynamic instability may result from blood loss of up to 3 units into the fracture site.54 Although such blood loss can lead to hypovolemic shock, other causes of hypotension in a trauma patient need to be considered. Open fractures are rare and when present are accompanied by significant soft tissue injury. Vascular and neurologic injuries are also uncommon.
Definitive management of subtrochanteric fractures is a complex issue. Maintaining limb length and controlling rotation are difficult. Open reduction with internal fixation generally is the treatment of choice. However, in the rare case with severe comminution or an open, grossly contaminated fracture, nonoperative management may be preferable.59 Children younger than 10 years also may be managed nonoperatively. The amount of remodeling and growth stimulation occurring in children of this age usually ensures good results without internal fixation.
Outcomes.: The bone in the subtrochanteric region is largely cortical and relatively avascular when compared with the cancellous intertrochanteric region. It logically follows that healing is comparatively slow. Comminution is common and increases the likelihood of nonunion. Comminuted and distal subtrochanteric fractures carry a worse prognosis.
Complications include fat embolism in patients of all ages, and the adverse effects of prolonged immobilization in the elderly. Reported mortality rates from subtrochanteric fractures range from 9.6 to 13.3%.59 The violent force and common associated injuries contribute to the high mortality among patients who sustain these fractures.
Femoral Shaft Fractures
Pathophysiology.: Femoral shaft fractures are common injuries in young adults after high-energy trauma. As is the case with other femoral cortical fractures, considerable violent force is required to produce a fracture in a normal shaft. Automobile and motorcycle accidents, falls, and pedestrian accidents account for a majority of femoral shaft fractures. The femoral shaft usually fails under tensile strain, and a transverse fracture results. Higher forces produce varying degrees of segmentation or comminution. Open fractures of the femoral shaft are less frequent and are often the result of a gunshot wound. Pathologic fractures occur from a low-mechanism force that may produce torsion and spiral fractures.60
Classification.: There is no commonly accepted or easily remembered classification for femoral shaft fractures. Location and geometry of the fracture line should be used to describe these fractures. Transverse, oblique, spiral, wedge, and comminuted are useful terms for describing these fractures.
Clinical Features.: Patients often arrive in the ED with the injured extremity immobilized by traction devices, which should be removed while immobilization of the limb is maintained. Neurovascular injuries are rarely associated with closed femoral shaft fractures.61 Significant hemorrhage into the thigh can occur with a femoral shaft fracture, just as it can with intertrochanteric and subtrochanteric fractures. Injuries commonly occurring in the presence of femoral shaft fractures include hip fractures, fracture-dislocations, femoral neck fractures, supracondylar femoral fractures, and patellar fractures.62 Almost half of femoral shaft fractures have associated ligamentous damage in the knee. If the patient has a femoral fracture, pain often prevents adequate evaluation of knee stability. Any attempt to evaluate the stability of the knee acutely will result in additional pain and hemorrhage without providing useful, reliable information.
Management.: Internal fixation with intramedullary rods has been demonstrated to shorten both hospitalization and total disability time with most femoral shaft fractures. The vast majority of femoral shaft fractures heal well in time, regardless of the mode of treatment. Severely comminuted fractures are more likely to be treated by closed reduction.
Outcomes.: Femoral shaft fractures have close to a 100% union rate, and most patients are able to return to work after approximately 6 months. Even a minor degree of limb shortening or malalignment can result in arthritis of the hip or knee or chronic back pain.63 Refracture is a rare occurrence that is most likely at two times during the healing process: during early healing and callus formation or during the brief period after the hardware is removed. After the hardware removal, the unsupported bone is required to bear the entire weight of axial loading and is at risk for refracture.
Fractures with Minimal or No Trauma
Most patients who arrive in the ED with hip or thigh pain will provide a clear history of a traumatic event. Hip or knee pain in the young, in athletes, and in the elderly deserves investigation, even when minimal or no trauma has been reported. This patient population commonly has occult hip pathology and occasionally femoral pathology. Although senile osteoporosis is the leading cause of femoral neck fractures after minor trauma, pathologic fractures of the femur may result from metastatic, metabolic, or endocrine disease.64
Stress Fractures
Pathophysiology.: Stress fracture of the femoral neck was first reported in 1905 by Blecher.65 Stress fractures occur when normal bone is repeatedly subjected to submaximal forces. This recurring stress stimulates the bones to remodel and strengthen. In a stress fracture, osteoblasts are unable to lay down new bone and remodel fast enough, so the bone fails. Stress fractures can also occur in diseased bone when it is subjected to repeated minimal stress.66
Clinical Features.: The symptoms of a stress fracture of the femoral neck often are so subtle that they may be mistaken for muscle strain or an overuse injury. Early symptoms frequently include morning stiffness and aching in the hip on the first steps after a period of rest. The pain gradually increases during prolonged exercise and may reach the point at which bearing weight becomes impossible. Pain is felt in the groin or along the medial aspect of the thigh toward the knee.
Diagnostic Strategies.: Radiographs are helpful if they demonstrate a fracture, but findings often are negative until 10 to 14 days after the injury.25 Endosteal or subperiosteal callus develops at the fracture site during this period. In addition to the standard AP and lateral views of the hip, oblique views may delineate the fracture line. Close attention should be paid to the trabecular fibers of the femoral neck. A stress fracture often can be identified as an isolated disruption of either the tensile (lateral aspect of the femoral neck) (Fig. 56-20A) or the compressive (medial aspect of the femoral neck) (Fig. 56-20B) trabecular fibers. If a fracture is suspected clinically but radiographic findings are negative, the next step is MRI.30 If a fracture is found, the contralateral hip should be extensively evaluated because of the significant incidence of bilateral stress fractures.
Management.: Treatment of stress fractures of the femoral neck is determined by the involvement of the compressive or tensile aspect. Compressive-side fractures involving less than half of the cortex are inherently stable and can be treated conservatively with partial weightbearing with crutches. Tension-side fractures and compressive-side fractures involving more than half the cortex are considered unstable and at risk for displacement. These fractures should be treated operatively with screw fixation.67
Dislocations and Fracture-Dislocations of the Hip and Femur
Epidemiologists have identified injury patterns in victims according to the mechanism of injury.68 Pedestrians who are struck by a car may have head, chest, pelvic, arm, and femur injuries. Motorcyclists tend to sustain pelvic and ipsilateral leg injuries. A person who stumbles and falls seldom has major associated injuries unless there is underlying bone pathology (e.g., osteogenesis imperfecta, osteoporosis). Each of these main categories of injury is discussed next.
Hip Dislocations
Dislocations and fracture-dislocations of the hip are two true orthopedic emergencies. The hip joint possesses impressive inherent strength and stability; therefore considerable force is required to produce these injuries. With this understanding, a hip dislocation serves as a “red flag” for multisystem injury and should prompt a diligent search for other occult injuries. Serious associated injuries are found in up to 95% of patients with a dislocated hip. There is an associated acetabular fracture in up to 70% of cases. Knee fractures, ligamentous injuries, and dislocations are present in up to 30% of patients sustaining a hip dislocation.69 It is highly recommended that in the presence of this type of injury, patients be managed as major trauma victims.
Mechanism and Biomechanics.: Traumatic hip dislocations occur primarily in patients sustaining severe multisystem trauma, most often as a result of a high-speed MVC. Failure to use seat belts is a significant risk factor. Less common mechanisms include falls, sports injuries, and pedestrians struck by automobiles.
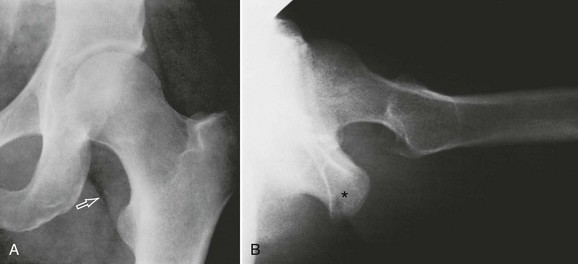
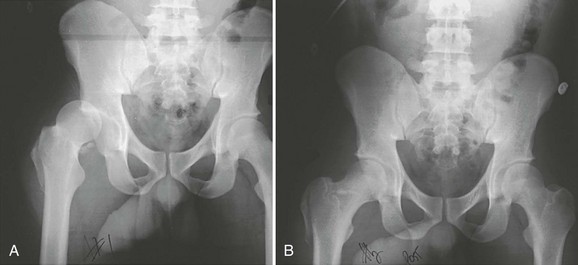
Classification.: The relationship of the femoral head to the acetabulum is used to classify dislocations into anterior, posterior, central, and inferior types. A fracture-dislocation includes an associated fracture of the acetabulum or femoral head. Posterior dislocations (Fig. 56-21) account for 80 to 90% of dislocations. Anterior dislocations (Fig. 56-22) are seen in 10 to 15% of patients. In anterior dislocations the femoral head may dislocate medially toward the obturator foramen (obturator dislocation) (Fig. 56-23) or laterally toward the pubis (pubic dislocation), or toward the iliac crest. Central dislocations, which occur in 2 to 4% of cases, are not true dislocations because the entire femoral head is forced centrally through a comminuted fracture of the acetabulum. Inferior dislocation of the hip associated with inversion of the femoral shaft (luxatio erecta femoris) is a very rare condition that may occur with or without associated trochanteric fracture.70
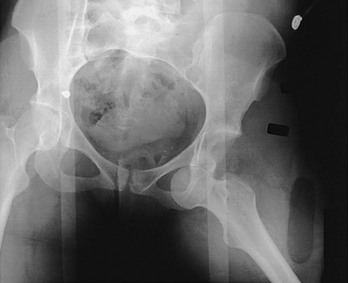
Figure 56-23 Radiograph of obturator dislocation.
Clinical Features.: The position of the injured extremity may provide valuable clues in the evaluation of a hip dislocation. A patient with a posterior dislocation typically holds the hip flexed, adducted, and internally rotated. The knee of the affected extremity rests on the opposite thigh. The extremity generally is shortened, and the greater trochanter and buttock may be unusually prominent. By contrast, a patient with an anterior dislocation holds the hip in abduction, slight flexion, and external rotation, and the leg may appear lengthened. These physical findings may be absent in patients with an associated ipsilateral femoral shaft fracture.
The neurovascular examination should focus on the sciatic nerve and femoral vessels. Sciatic palsy is present in approximately 10% of patients with hip dislocation and most commonly involves the peroneal nerve branch. The most sensitive clinical sign of peroneal nerve palsy is weakness of the extensor hallucis longus; other signs include weakness of dorsiflexion and numbness or tingling over the dorsum of the foot. The femoral vessels and nerve are particularly prone to injury after an anterior dislocation.71
Diagnostic Strategies.: Radiologic investigation begins with an AP view of the pelvis. This view alone will identify a majority of hip dislocations. An AP pelvis film should be obtained in all trauma patients with the aforementioned deformities. The AP radiograph should include the entire pelvis and the proximal third of the femur to allow comparison of both hips. When a dislocation is found or suspected, a lateral view of the hip will provide additional definition of the injury.
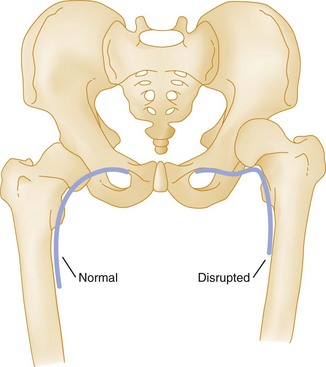
Although most hip dislocations are seen clearly with these two views, several more subtle radiographic signs may assist physicians in making a confident diagnosis. The first indicator involves the position of the lesser trochanter. Because a posteriorly dislocated hip is internally rotated, the lesser trochanter is superimposed on the femoral shaft and is not seen on the AP projection. By contrast, an anteriorly dislocated hip is externally rotated, and the lesser trochanter appears in profile. The second clue is found in the size of the femoral head. Because a posteriorly dislocated hip is closer than the unaffected side to the x-ray cassette, it appears smaller. The converse is true in anterior dislocations, in which the hip is farther from the x-ray cassette than the contralateral side is and thus appears larger. The third finding relates to the integrity of Shenton’s line (Fig. 56-24). This line is a smooth, curved line drawn on the radiograph along the superior border of the obturator foramen and medial aspect of the femoral metaphysis. Disruption of this line should raise suspicion for a femoral neck fracture or hip dislocation.72
An obvious dislocation may distract the emergency physician from a search for concomitant fractures. Examination of the trabecular pattern can identify associated fractures of the acetabulum and femoral head, neck, or shaft. It is important to identify acetabular fractures before closed reduction is attempted because intra-articular bone fragments may interfere with effective reduction.73 Although these fractures may make the reduction more difficult, their presence is not a contraindication to reduction.
Management.: Hip dislocations constitute a true orthopedic emergency, and reduction should be performed within 6 hours. The earlier the reduction, the better the results. The incidence of AVN, traumatic arthritis, permanent sciatic nerve palsy, and joint instability logarithmically increases with the length of time for which the hip remains dislocated.73,74
Reduction Techniques.: Stimson’s technique and the Allis technique are the methods most commonly used for reduction of posterior hip dislocations25 (Fig. 56-25). The Allis technique usually is effective for both posterior and obturator dislocations (Fig. 56-26). It is perhaps the most commonly used method for hip reductions in the ED.

Figure 56-25 Radiograph of posterior dislocation identified by loss of the lesser trochanter on the anteroposterior view.
Allis technique for reduction of posterior hip dislocation:
1. The patient is placed in the supine position, and the pelvis is stabilized by an assistant.
2. With the knee flexed, the operator applies steady traction in line with the deformity.
3. The hip is slowly brought to 90 degrees of flexion while steady upward traction and gentle rotation are applied.
4. The assistant pushes the greater trochanter forward toward the acetabulum.
5. Once reduction has been achieved, the hip is brought to the extended position while traction is maintained.
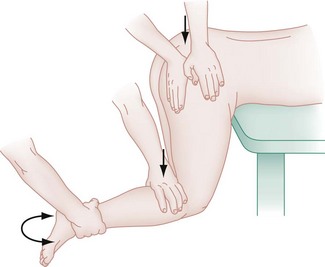
Stimson’s technique (Fig. 56-27) uses the weight of the limb and the force of gravity to reduce the dislocation and is relatively atraumatic. Although Stimson’s technique generally is effective, placing an acutely and often multiply injured trauma patient in the required prone position may be a challenge. Adequate radiographic clearance of the spine usually has not yet been accomplished, and the administration of sedatives and analgesics in a prone patient has inherent risks.
Stimson’s technique for reduction of posterior hip dislocation:
1. The patient is placed in a prone position, with the leg hanging over the edge of the bed. The hip and knee are flexed at 90 degrees.
2. An assistant stabilizes the pelvis.
3. The operator applies steady downward traction in line with the femur.
4. The femoral head is gently rotated, and the assistant pushes the greater trochanter anteriorly toward the acetabulum.
5. Once reduction has been achieved, the hip is brought to the extended position while traction is maintained.
Other techniques for closed reduction of posterior hip dislocations include the Rochester method,75 the Whistler method,76 and the traction-countertraction technique.77
Postreduction Management.: After closed reduction, the hip should be tested for stability, which is accomplished by gently taking it through a full range of motion to see whether it will redislocate. After testing has ensured stability, the injured extremity should be placed in a knee immobilizer and an abduction pillow should be applied to prevent repeat dislocation. An AP radiograph of the pelvis should be obtained to verify the adequacy of reduction. The radiograph should be carefully inspected to verify that the femoral head is in the acetabulum, the shaft of the femur is in neutral position, Shenton’s line is intact, and the profile of the lesser trochanter is well visualized. The intra-articular space should be symmetrical and, when measured, of the same depth as in the unaffected joint. Asymmetry signals an entrapped intra-articular fragment and is an indication for CT scanning (Fig. 56-28).
Outcomes.: The precarious blood supply to the femoral head is particularly important with regard to the long-term consequence of hip dislocations. The development of AVN of the femoral head has been reported in 1 to 17% of dislocations.74 Other risk factors for the development of AVN include the total dislocation time, the severity of the injury, the number of reduction attempts, and the presence of comorbid conditions.
Fracture-Dislocation of the Femoral Head
Epidemiology and Mechanism.: Hip dislocations may be associated with fractures of the femoral head (Fig. 56-29A). Femoral head fracture occurs in 35 to 55% of anterior hip dislocations and in 10 to 16% of posterior hip dislocations.78 These injuries are almost always the result of high-speed vehicular trauma. Because of the tremendous force required to produce this injury pattern, coexistent multisystem trauma is the rule.
When a femoral head fracture and hip dislocation coexist, patients assume the position typical for the dislocation. Hip mobility is markedly reduced, and pain usually is severe. After initial stabilization, the involved extremity should be carefully examined for associated fractures of the femoral shaft and knee. The neurovascular examination should assess for femoral or sciatic nerve injury. Radiographs should be evaluated carefully for any femoral head fracture in all patients with hip dislocations. Evidence for fracture of the femoral head can be subtle. These fractures may be detected on radiographs by following the curve of the dislocated head and the acetabular cup to search for a small fragment that may otherwise be overlooked. Known or suspected injuries can be further defined by CT or MRI.73,78
In most cases, satisfactory results can be obtained with closed reduction (see Fig. 56-29B).73 Several experts recommend obtaining a CT scan of the hip before closed reduction to further define the injury and locate fracture fragments.73 If the hip cannot be reduced by manipulation or if reduction of the femoral head fragment is unsatisfactory, open reduction will be required.
Dislocation of Hip Prosthetics
An increasing number of patients have undergone hip arthroplasty. In addition to those procedures performed for treatment of femoral neck fractures, more than 230,000 patients undergo elective primary THA each year.79 Postoperative dislocation may occur in 0.5 to 3% of patients with primary THA and in 5 to 27% of patients with a revised THA.80 Although most dislocations take place within 3 months of surgery, “late dislocations” have been reported up to 10 years after the operative procedure; such dislocations can result from major trauma or from trivial events (e.g., rising from a seated position). Posterior dislocations account for 75 to 90% of cases (see Fig. 56-13).79 Reduction techniques for prosthetic hip dislocations are identical to those described earlier. Consultation with an orthopedic surgeon is essential for safe reduction and development of a long-term treatment plan for the patient. Reduction of the prosthesis does not carry the same urgency as for reduction of a dislocated native hip because there is no risk for the development of AVN once the femoral head has been replaced. Traction on the sciatic nerve can occur, however, making early reduction more compelling. In addition, the reduction itself carries the unique dangers of loosening of the components, fracturing of the surrounding bone, and movement of the acetabular cup. Reduction is best performed with an orthopedic consultant.
Soft Tissue Injuries
Muscular Injuries
Strenuous exercise in a poorly conditioned person, sudden exertion, and direct trauma all may traumatize soft tissues. Cold temperature, vascular or infectious disease, fatigue, and poor training are known predisposing conditions for muscular injury.81
Sports Injury Patterns.: Athletes commonly experience muscular injury from accidents and overtraining. The two most common injuries involve the hamstrings and the quadriceps.
The Hamstrings.: Hamstring muscle strains are common in sports involving running and sudden acceleration. The injury is accompanied by sudden intense pain in the posterior aspect of the thigh. Any active or passive motion at the hip is poorly tolerated because of the intense pain that movement causes. Ischial avulsion fractures can occur, and pelvic radiographs should be obtained if the examination reveals bony tenderness. Crutches and toe-touch weightbearing are recommended until the patient is evaluated by a physician trained in sports medicine. Toe-touch weightbearing refers to walking with crutches while the toes of the injured extremity rest on the ground without placing any weight on it. Appropriate weight-training programs have been shown to speed rehabilitation of this injury. Complete recovery from a hamstring muscle strain may take weeks to months.
The Quadriceps.: The quadriceps is the most common muscular group to sustain complete tears. This injury occurs when the muscles are contracted suddenly against the body’s weight, as may occur when an athlete slips or stumbles and attempts to avoid a fall. Ambulation is significantly affected. There is pain with active and passive knee extension. In significant tears, the patient may be unable to actively extend the knee or maintain its extension against gravity. A palpable depression just proximal to the superior pole of the patella suggests a complete tear. It is imperative to document an intact patellar mechanism on examination because a complete tear of the quadriceps most often requires surgical repair and extensive rehabilitation.
Iliopsoas Strain.: Gymnasts and dancers are the group of athletes most likely to experience an injury to the iliopsoas as a result of sudden forceful hip flexion against resistance. Severe pain often is experienced in the groin, thigh, or low back region. Severe intra-abdominal pain is common at the muscle origin and may dominate the clinical picture. Examination reveals groin tenderness and pain with active hip flexion. Radiographs of the femur should be obtained to identify an avulsion fracture of the lesser trochanter. CT frequently will demonstrate a large hematoma. Bed rest with partial flexion at the knee and hip generally is required for 7 to 10 days. With severe strains, symptoms may persist for 2 to 3 months.
Hip Adductor Strain.: Injury to the hip adductors occurs as the thigh is forcefully abducted, as in a straddle injury. The patient reports pain in the groin, the pubic region, and the medial proximal aspect of the thigh. Abduction and adduction often are limited because of pain. Swelling and skin discoloration may confirm presence of the tear. If the tear is complete, a defect in the muscle may be felt by the examiner along the medial aspect of the thigh near the groin. Treatment is conservative, with patients initially benefiting from rest, with gradual progression in a stretching and strengthening program.
Tendon Injuries
A groin pull is the lay term for an injury to the tendons of the hip adductors. One study found adductor strains to be the most common groin injury in athletes, with 62% of the cases involving the adductor longus muscle.81 The adductor magnus and brevis and the pectineus often are involved as well.82 This injury commonly occurs in skaters and cross-country skiers when an accidental stress abducts the thigh during a powerful contraction of the adductors. These muscles also may be injured from overuse in an unconditioned patient. Local pain is noted at the inferior pubic ramus and the ischial tuberosity. Extension, abduction, and adduction of the hip are painful. The pain may radiate to the back of the thigh.
Osteitis Pubis
Osteitis pubis is a poorly understood disorder. It is characterized by pubic symphysis pain and joint disruption and is most common in distance runners and soccer players.83 The adductor muscles act as a “compression strut,” displacing forces across the hip. The most likely mechanism is repetitive pulling of the adductor muscles, causing increased shearing at the pubic symphysis.
Clinically, patients have groin pain of insidious onset, with most reporting pain at the symphysis and adductor muscles.84 Pain usually can be elicited on palpation of the symphysis and also can be provoked by adduction of the hip or by sit-ups. Plain radiographs show widening of the symphysis, irregular contour of the articular surfaces, or periarticular sclerosis (a late finding) (Fig. 56-30). These features are not specific and in one study were seen in 76% of asymptomatic soccer players. MRI is the imaging study of choice and will show marrow edema on T2 images early in disease. Osteitis pubis has been associated with spontaneous cases of pubic symphysis osteomyelitis, and this should be considered in the differential diagnosis.84
Vascular Injuries
Hip dislocations and femoral fractures may have associated arterial injury. The vessel may be partially lacerated, dissected, completely severed, or thrombosed. Lack of distal arterial flow may also represent a stretched vessel in spasm. The superficial femoral artery is most commonly injured with trauma to the hip and thigh. The common and the deep femoral arteries are less frequently injured. In the acute setting, penetrating trauma is the usual mechanism of injury. Arterial injury with femoral shaft fractures is rare. Anterior- and superior-type dislocations may produce femoral artery injury.25
Comparative blood pressures obtained by Doppler examination in the injured and uninjured extremities at the ankle may be useful in suspected arterial injuries. If the systolic pressure in the affected extremity is 90% or less (index less than 0.9) than that in the unaffected extremity, additional diagnostic studies should be undertaken. The ABI also can be similarly determined by comparing the systolic pressures of the affected extremity and of the ipsilateral arm. An index less than 0.9 necessitates further diagnostic studies.23 Additional diagnostic studies include Doppler flow ultrasound imaging, CT angiography, and angiography alone. CT angiography, however, is becoming more prevalent, with recent studies showing 96 and 97% sensitivity and specificity, respectively, when compared with conventional radiography.85
Neurologic Injuries
Femoral Nerve.: When the femoral nerve is injured, the iliac and femoral arteries are commonly involved because of their anatomic proximity. The femoral nerve is most often traumatized in penetrating trauma of the pelvis, groin, or thigh. Femoral neuropathy can occasionally result from compression by a hematoma within the abdominal wall or the iliopsoas as a complication of hemophilia, anticoagulant therapy, or severe trauma.86
Sciatic Nerve.: Sciatic injury is rare with femur fractures, but occasionally it may be the result of traction used to stabilize the fracture during the initial management period. Complete traumatic injury may result from a deep penetrating wound in the hip, thigh, or buttock. Posterior hip dislocations and fracture-dislocations produce sciatic neurapraxia in 10 to 14% of these injuries.25,71 Patients with complete sciatic neuropathy have paralysis of the hamstring muscles and all muscles below the knee. With partial injury, a peroneal palsy with weakness of the extensor hallucis longus muscle is the most sensitive clinical sign. There is sensory loss below the knee and along the posterior aspect of the thigh. The deep tendon reflex at the ankle is absent or diminished. Sciatic nerve palsy from inadvertent injection into the nerve or secondary to intraneural or extraneural hemorrhage in patients taking anticoagulants has been described.
Special Pediatric Considerations
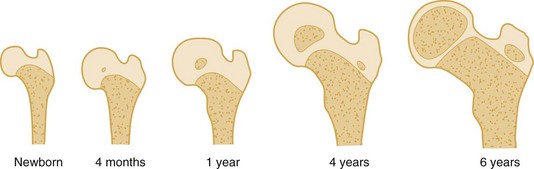
Development of the femoral head and neck with its growth plates and two primary ossification centers is illustrated in Figure 56-31. A significant proportion of the pediatric hip is cartilage and developing new bone. For this reason, almost any type of trauma in this location carries the potential for premature growth arrest. Recognition that large portions of the pediatric hip are radiolucent will counter the tendency to focus attention on the ossified elements only.
Hip and Femur Fractures
The Salter-Harris classification of fractures in the pediatric population is not used for hip fractures. The Delbet classification is a well-accepted system used for pediatric femoral fractures.87 This system separates fractures through the physis and the transcervical, cervicotrochanteric, and intertrochanteric regions (Fig. 56-32).
Spiral Shaft Fractures
If seemingly trivial trauma has resulted in a spiral femoral shaft fracture in a child, nonaccidental trauma and pathologic fracture should be considered.88,89 Common causes of pathologic fracture include unicameral bone cysts, fibrous dysplasia, osteogenesis imperfecta, and malignancy.89
Management.: Although these pediatric injuries are extremely rare, their complications are significant. Unlike in an adult, a child’s femur has growth potential, and any disruption carries the possibility of lifetime disability. Treatment of femoral shaft fractures in adults is aimed at prevention of the complications of prolonged immobilization. Unlike adults, children tolerate bed rest well, which allows more treatment options. The primary goal in children is prevention of the many complications common with femoral fractures. Premature closure of the physeal plate results in a valgus deformity of the hip. AVN, malunion, nonunion, and limb-length discrepancy all are complications frequently seen with pediatric femoral fractures. For these reasons, referral to a pediatric orthopedist is recommended.87
Child with a Limp
Etiology of the Limp
Inflammation and Infection.: Inflammation of the articular surface, the intra-articular synovium, or the joint capsule creates pain. Weightbearing increases the pain. The child limps in an attempt to limit the time during which the affected hip bears the body’s weight.
The diagnosis of transient synovitis is one of exclusion of more serious diseases that mimic this condition. Acute joint inflammation and pain may be associated with septic arthritis, juvenile rheumatic arthritis, systemic lupus erythematosus, Perthes’ disease, and tuberculous arthritis. Ultrasound imaging of the hip joint will detect an effusion in 78% of cases of transient synovitis but cannot distinguish this condition from septic arthritis.90 Joint aspiration may be required when the diagnosis is in doubt.
Distinguishing between transient synovitis and septic arthritis can be a diagnostic dilemma. Key predictors may include temperature higher than 38.5° C in the preceding week, non–weight-bearing status (refusal or inability to bear weight even with support), erythrocyte sedimentation rate higher than 40 mm/hr, and a white blood cell count greater than 12,000/mL. These four predictors were developed in a retrospective study and then validated in a prospective study.91,92 Based on the validation study, the probability of septic arthritis was 2% for zero predictors, 9.5% for one predictor, 35% for two predictors, 73% for three predictors, and 93% for four predictors.93
The use of C-reactive protein (CRP) assay is becoming more prevalent in the evaluation of septic arthritis. A positive CRP (defined as a result greater than 2.0 mg/dL) has been identified as a strong independent risk factor for septic arthritis.94,95 Taken together, all of these predictors should be used in conjunction with clinical assessment.
Acute bacterial infections of the hip and femur require early identification and intervention to minimize subsequent morbidity and disability.93 Unfortunately, the diagnosis often is missed initially because the child may appear relatively nontoxic in the early phases of infection. Signs and symptoms of systemic illness usually accompany infection of the femur or hip. Fever, malaise, decreased oral intake, a limp, and refusal to bear any weight are common.96 Whereas osteomyelitis most commonly develops in the metaphysis in adults, the physeal region often is the infected site in children. Septic arthritis (pyarthrosis) may result from hematogenous seeding or direct extension of osteomyelitis. The hip and the knee are the most commonly infected joints.
Identification of acute osteomyelitis on plain radiographs is difficult until 2 to 3 weeks after onset of infection. Pyarthrosis may manifest with widening of the space between the femoral head and the acetabular roof and bulging of the joint capsule and surrounding soft tissues. This is seen as a change in the contour of the gluteus minimus and iliopsoas fat stripes (Fig. 56-33). Care should be taken to identify the normal shadow of the muscles and the joint capsule, as described earlier in this chapter (see Fig. 56-11). Plain radiographs are seldom useful in the initial identification of infection because visualization of a joint effusion has low sensitivity for pyarthrosis. Bone scan, MRI, CT, and ultrasound-guided joint aspiration are appropriate to diagnose a septic joint.
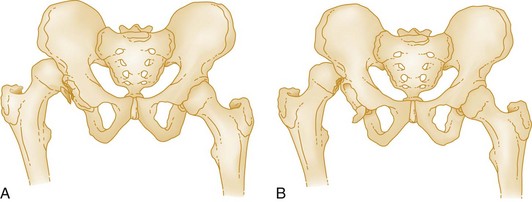
Slipped Capital Femoral Epiphysis:
Anatomy.: The capital femoral epiphysis appears during the first year of life. The epiphysis of the greater trochanter appears by the age of 5 years and that of the lesser trochanter during the 13th year of life. All of these structures unite at age 17 to 19 years. The anatomic relationship has been compared with a scoop of ice cream sitting on a cone. This relationship remains symmetrical on both AP and frogleg lateral radiographs (Fig. 56-34A and B). Asymmetry in any view represents either SCFE or a subcapital fracture (Fig. 56-35).
Epidemiology and Pathophysiology.: SCFE is the most common hip disorder in adolescents, with an incidence of approximately 5 per 100,000 population per year. From 25 to 50% of the cases are bilateral.46,97 SCFE occurs twice as frequently in boys as in girls, with the respective peaks of incidence at the ages of 13 and 11 years.
Epidemiologic data have provided clues to the pathophysiology of this injury. SCFE is associated with the onset of puberty and is rare before the age of 10 years. It most commonly is seen in boys 10 to 17 years of age during their period of rapid growth. It is believed to be the result of a structural weakness in physeal cartilage associated with pubescence.9
The specific cause of SCFE is not well understood, and most cases are deemed idiopathic. There are likely genetic and environmental factors that influence the development of SCFE. It occurs more frequently in male African Americans than in the Caucasian population and has seasonal and geographic variation.9 Other risk factors identified are obesity, previous irradiation or chemotherapy, renal osteodystrophy, hypothyroidism, and neglected septic arthritis.98
Clinical Features.: SCFE is usually an insidious process extending over weeks to months. Initially, the only complaint may be slight discomfort in the groin, thigh, or knee after activity. Shear stress combined with a weaker physeal plate leads to slippage of the epiphysis inferiorly and posteriorly in the direction of weight-bearing force. Pain worsens as slippage progresses, and eventually pain may occur at rest as well. Referred pain to the knee is a classic manifestation, and patients frequently have groin, thigh, or knee pain rather than hip pain. This presentation often causes delay in diagnosis, potentially increasing displacement and worsening the prognosis.99 Parents often bring the child in for medical evaluation when they notice the child beginning to limp. Physical examination may reveal hip tenderness, decreased hip range of motion, and an abducted, externally rotated thigh.
Diagnostic Strategies and Treatment.: Children with unexplained hip or knee pain merit clinical as well as radiographic evaluation. Initially, AP, lateral, and frogleg lateral radiographs of the hip should be obtained. The frogleg lateral projection shows the hip in a plane midway between the AP and lateral views. The earliest radiographic findings are subtle, with the abnormality visualized on only one projection. The most reliable initial finding with SCFE is asymmetry of the femoral epiphysis in relation to the neck. Small amounts of slippage can be detected by examining the epiphyseal edge as it becomes flush with the superior border of the femoral neck. This can be visualized as “the scoop slipping off the ice cream cone.” The dome of the epiphysis may be flattened. On the radiograph, a line drawn along the superior margin of the femoral neck (Klein’s line) should intersect some part of the normal femoral head. Failure of this line to intersect the head indicates medial and posterior movement of the head on the epiphysis.97 Comparative views of the two hips are indicated if initial radiographic findings are equivocal. If occult fracture is suspected, MRI or CT should be performed.27,100 The goal of treatment is to prevent further slippage and subsequent injury to the physis. The patient should be placed on non–weight-bearing status and referred for orthopedic management. Surgery is required to anchor the epiphysis and prevent further slippage.
Perthes’ Disease.: Perthes’ disease is the name given to AVN of the pediatric femoral head (Fig. 56-36). It also has been called Legg-Calvé-Perthes disease and Calvé-Perthes disease. A majority of cases are diagnosed at ages 4 to 8, with the peak incidence at 6 years. It occurs five times more often in boys than in girls and affects both hips 15 to 24% of the time.101
Isolated Fracture of the Greater or Lesser Trochanter in Children.: An isolated fracture of the greater trochanter is a rare injury. In children, this fracture occurs when the entire greater trochanteric epiphysis is avulsed from the femur. Children and adolescents aged 7 to 17 years are most commonly affected. The mechanism of injury generally is a powerful muscular contraction of the lateral rotators of the hip joint during a twisting fall. If the fragment is large and displaced by more than 1 cm, open reduction and internal fixation may be indicated.
An isolated fracture of the lesser trochanter occurs when a forceful contraction of the iliopsoas muscle avulses the lesser trochanter from the physis during sudden hip flexion (Fig. 56-37). Eighty-five percent of all cases occur in patients younger than 20 years, with a peak incidence in males between aged 13 to 17 years.102 Marked tenderness can be elicited in the femoral triangle, and hip flexion against resistance is painful. Clinically, the seated patient is unable to lift the foot of the affected leg from the floor. Treatment of an isolated lesser trochanter avulsion fracture usually involves bed rest and early mobilization. Painless active hip motion is achieved within 3 weeks.
References
1. Paré, A. The Work of That Famous Chirurgeon, Ambrose Paré, translated out of Latin and compared with the French by Tho Johnson, book XV. London: T Cotes & R Young; 1634.
2. Von Langenbeck, B. Verhandld, Deutch, p 92. Gesellsch F, Chir 1878. As found in Davis GG: The operative treatment of intracapsular fracture of the neck of the femur. Am J Orthop Surg. 1908-1909;6:481.
3. National Osteoporosis Foundation. America’s Bone Health: The State of Osteoporosis and Low bone Mass in Our Nation. Washington, DC: National Osteoporosis Foundation; 2002.
4. Koval, KJ, Zuckerman, JD. Functional recovery after fracture of the hip. J Bone Joint Surg Am. 1994;77:751.
5. Burge, R, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–475.
6. Dominguez, S, Liu, P, Roberts, C, Mandell, M, Richman, PB. Prevalence of traumatic hip and pelvic fractures in patients with suspected hip fracture and negative initial standard radiographs—a study of emergency department patients. Acad Emerg Med. 2005;12:366–369.
7. Kesmezacar, H, Aynan, E, Uniu, M, Seker, A, Karaca, S. Predictors of mortality in elderly patients with an intertrochanteric or a femoral neck fracture. J Trauma. 2010;68:153–158.
8. Perry, DC, Hall, AJ. The epidemiology and etiology of Perthes disease. Orthop Clin North Am. 2011;42:279–283.
9. Lehmann, CL, Arons, RR, Loder, RT, Vitale, MG. The epidemiology of slipped capital femoral epiphysis: An update. J Pediatr Orthop. 2006;26:286–290.
10. Gray, H. Anatomy, Descriptive and Surgical, 17th ed. New York: Bounty Books; 1997.
11. Lane, NE. Epidemiology, etiology, and diagnosis of osteoporosis. Am J Obstet Gynecol. 2006;194:S3.
12. Gehibach, SH, Avrunin, JS, Puleo, E. Trends in hospital care for hip fractures. Osteoporos Int. 2007;18:585.
13. Brunner, LC, Eshilian-Oates, L. Hip fractures in adults. Am Fam Physician. 2003;67:537.
14. Mathers, C, Fat, DM. The Global Burden of Disease—2004 Update. Geneva: World Health Organization; 2004.
15. Lane, NE. Osteoarthritis of the hip. N Engl J Med. 2007;357:1413.
16. Lavernia, CJ, Sierra, RJ, Grieco, FR. Osteonecrosis of the femoral head. J Am Acad Orthop Surg. 1999;7:250–261.
17. Mont, MA, Jones, LC, Hungerford, DS. Nontraumatic osteonecrosis of the femoral head: Ten years later. J Bone Joint Surg Am. 2006;88:1117–1132.
18. Sahin, V, et al. Traumatic dislocation and fracture dislocation of the hip: A long-term follow-up study. J Trauma. 2003;54:520.
19. Bachiller, FG, Caballer, AP, Portal, LF. Avascular necrosis of the femoral head after femoral neck fracture. Clin Orthop Relat Res. 2002;399:87.
20. Järvinen, TA, et al. Muscle injuries: Optimising recovery. Best Pract Res Clin Rheumatol. 2007;21:317.
21. Beiner, JM, Jokl, P. Muscle contusion injury and myositis ossificans traumatica. Clin Orthop Relat Res. 2002;403:S110.
22. Muir, B. Myositis ossificans traumatica of the deltoid ligament in a 34 year old recreational ice hockey player with a 15 year post-trauma follow-up: A case report and review of the literature. J Can Chiropr Assoc. 2010;54:229–242.
23. Vestergaard, P, et al. Corticosteroid use and risk of hip fracture: A population-based case-control study in Denmark. J Intern Med. 2003;254:486.
24. Koval, KJ, Chen, AL, Aharonoff, GB, Egol, KA, Zuckerman, JD. Clinical pathway for hip fractures in the elderly: the Hospital for Joint Diseases experience. Clin Orthop Relat Res. 2004;425:72.
25. Tornetta, P. Hip dislocations and fractures of the femoral head. In Bucholz RW, Heckman JD, Court-Brown JM, Tornetta P, eds.: Rockwood and Green’s Fractures in Adults, 7th ed, Philadelphia: JB Lippincott, 2009.
26. Feliciano, DV. Management of peripheral arterial injury. Curr Opin Crit Care. 2010;16:602–608.
27. Harris, JH, Harris, WH, Novelline, RA. The Radiology of Emergency Medicine, 3rd ed. Baltimore: Williams & Wilkins; 1993.
28. Rizzo, PF, Gould, ES, Lyden, JP, Asnis, SE. Diagnosis of occult fractures about the hip: Magnetic resonance imaging compared with bone scanning. J Bone Joint Surg Am. 1993;73:395.
29. Lubovsky, O, Liebergall, M, Mattan, Y, Weil, Y, Mosheiff, R. Early diagnosis of occult hip fractures MRI versus CT scan. Injury. 2005;36:788.
30. Perron, AD, Miller, MD, Brady, WJ. Orthopedic pitfalls in the emergency department: Radiographically occult hip fracture. Am J Emerg Med. 2002;20:234.
31. Vidán, M, Serra, JA, Moreno, C, Riquelme, G, Ortiz, J. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: A randomized controlled trial. J Am Geriatr Soc. 2005;53:1476–1482.
32. Schnell, S, Friedman, SM, Mendelson, DA, Bingham, KW, Kates, SL. The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil. 2010;1:6–13.
33. Wood, SP, Vrahas, M, Wedel, SK. Femur fracture immobilization with traction splints in multisystem trauma patients. Prehosp Emerg Care. 2003;7:241.
34. Parker, MJ, Handoll, HH. Pre-operative traction for fractures of the proximal femur in adults. Cochrane Database Syst Rev. 3, 2006.
35. Brillman, J, Quenzer, RW. Infectious Disease in Emergency Medicine, 2nd ed. Philadelphia: Lippincott-Raven; 1998.
36. Mithöfer, K, Lhowe, DW, Vrahas, MS, Altman, DT, Altman, GT. Clinical spectrum of acute compartment syndrome of the thigh and its relation to associated injuries. Clin Orthop Relat Res. 2004;425:223.
37. Rupp, T, Delaney, KA. Inadequate analgesia in emergency medicine. Ann Emerg Med. 2004;43:494.
38. Fletcher, AK, Rigby, AS, Heyes, FLP. Three-in-one femoral nerve block as analgesia for fractured neck of the femur in the emergency department: A randomized controlled trial. Ann Emerg Med. 2003;41:227.
39. Mutty, CE, Jensen, EJ, Manka, MA, Jr., Anders, MJ, Bone, LB. Femoral nerve block for diaphyseal and distal femoral fractures in the emergency department. J Bone Joint Surg Am. 2007;89:2599.
40. Beaudoin, FL, Nagdev, A, Merchant, RC, Becker, BM. Ultrasound-guided femoral nerve blocks in elderly patients with hip fractures. Am J Emerg Med. 2010;28:76–81.
41. Spektor, M, Kelly, J. Nerve blocks of the thorax and extremities. In Roberts J, Hedges J, eds.: Clinical Procedures in Emergency Medicine, 5th ed, Philadelphia: WB Saunders, 2010.
42. Harkness, JW. Arthroplasty of the hip. In Canale ST, ed.: Campbell’s Operative Orthopaedics, 9th ed, St Louis: Mosby, 1998.
43. Hall, MJ, DeFrances, CJ, Williams, SN, Golosinkly, A, Schwartzman, A. National Hospital Discharge Survey: 2007 summary. Natl Health Stat Report. 2010;29:1.
44. Liu, SS, Della Valle, AG, Besculides, MC, Gaber, LK, Memtsoudis, SG. Trends in mortality, complications and demographics for primary hip arthroplasty in the United States. Int Orthop. 2009;33:643.
45. Shaw, JA, Greer, RB. Complications of total hip replacement. In Epps CH, Jr., eds.: Complications in Orthopedic Surgery, 3rd ed, Philadelphia: JB Lippincott, 1994.
46. Kocher, JS, Tucker, R. Pediatric athlete hip disorders. Clin Sports Med. 2006;25:241.
47. Rossi, F, Dragoni, S. Acute avulsion fractures of the pelvis in adolescent competitive athletes. Prevalence, location, and sports distribution of 203 cases collected. Skeletal Radiol. 2001;30:127–131.
48. Gidwani, S, Bircher, M. Avulsion injuries of the hamstring origin—a series of 12 patients and management algorithm. Ann R Coll Surg Engl. 2007;89:394.
49. Johnell, O, et al. Predictive value of BMD for hip and other fractures. J Bone Miner Res. 2005;20:1185.
50. Dobbs, RE, Parvize, J, Lewallen, DG. Preoperative morbidity and 30-day mortality after intertrochanteric hip fractures treated by internal fixation or arthroplasty. J Arthroplasty. 2005;20:963.
51. Ahmad, LA, Eckhof, DG, Kramer, AM. Outcome studies of hip fractures: A functional viewpoint. Orthop Rev. 1994;23:19.
52. Shorr, AF, et al. Venous thromboembolism after orthopedic surgery: Implications of the choice for prophylaxis. Thromb Res. 2007;121:17.
53. De Boeck, H. Classification of hip fractures. Acta Orthop Belg. 1994;60(Suppl 1):106.
54. Adunsky, A, Lichtenstein, A, Mizrahi, E, Arad, M, Heim, M. Blood transfusion requirements in elderly hip fracture patients. Arch Gerontol Geriatr. 2003;36:75.
55. Huddleston, JM, Whitford, KJ. Medical care of elderly patients with hip fractures. Mayo Clin Proc. 2001;76:295.
56. Stern, R. Are there advances in the treatment of extracapsular hip fractures in the elderly? Injury. 2007;38(Suppl 3):S77.
57. Lyles, KW, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799.
58. Nork, SE, Reilly, MC. Subtrochanteric fractures of the femur. In: Browner BD, et al, eds. Skeletal Trauma. Philadelphia: Saunders, 2008.
59. Craig, NJ, Maffuli, N. Subtrochanteric fractures: Current management options. Disabil Rehabil. 2005;27:1181.
60. Zlowodzki, M, Bhandari, M, Marek, DJ, Cole, PA, Kregor, PJ. Operative treatment of acute distal femur fractures: Systematic review of 2 comparative studies and 45 case series (1989 to 2005). J Orthop Trauma. 2006;20:366–371.
61. Hafez, HM, Woolgar, J, Robbs, JV. Lower extremity vascular injury: Results of 550 cases and review of the risk factors associated with limb loss. J Vasc Surg. 2001;33:122.
62. Hau, T, et al. Fixation of femoral fractures in multiply-injured patients with combined chest and head injuries. Aust N Z J Surg. 2003;73:1018.
63. Nork, SE. Femoral shaft fractures. In Bucholz RW, Heckman JD, Court-Brown JM, Tornetta P, eds.: Rockwood and Green’s fractures in adults, 7th ed, Philadelphia: JB Lippincott, 2009.
64. Stein, E, Shane, E. Secondary osteoporosis. Endocrinol Metab Clin North Am. 2003;32:115.
65. Blecher, A. Über den Einfluß des Parademarsches auf der Entstehung der Fußgeschwulst. Med Klin. 1905;1:305.
66. DeFranco, MJ, Recht, M, Schils, J, Parker, RD. Stress fractures of the femur in athletes. Clin Sports Med. 2006;25:89.
67. Harrast, MA, Colonno, D. Stress fractures in runners. Clin Sports Med. 2010;29:399–416.
68. Leung, KS, So, WS, Lam, TP, Leung, PC. Treatment of ipsilateral femoral shaft fractures and hip fractures. Injury. 1993;24:41.
69. Ferguson, KL, Harris, V. Inferior hip dislocation in an adult: Does a rare injury now have a common mechanism? Am J Emerg Med. 2000;16:117.
70. Kolar, MK, Joseph, S, McLaren, A. Luxatio erecta of the hip. J Bone Joint Surg Br. 2011;93:273.
71. Cornwall, R, Radomisli, TE. Nerve injury in traumatic dislocation of the hip. Clin Orthop Relat Res. 2000;377:84.
72. Newton, E, Love, J. Emergency department management of selected orthopedic injuries. Emerg Med Clin North Am. 2007;25:763–793.
73. Brooks, RA, Ribbans, WJ. Diagnosis and imaging studies of traumatic hip dislocations in the adult. Clin Orthop Relat Res. 2000;377:15–23.
74. Yang, EC, Cornwall, R. Initial treatment of traumatic hip dislocation in the adult. Clin Orthop Relat Res. 2000;377:24.
75. Stefanich, RJ. Closed reduction of posterior hip dislocation: The Rochester method. Am J Orthop. 1999;28:401.
76. Walden, PD, Hamer, JR. Whistler technique used to reduce traumatic dislocation of the hip in the emergency department setting. J Emerg Med. 1999;17:441.
77. Dahner, LE, Hundley, JD. Reduction of posterior hip dislocations in the lateral position using traction-countertraction: Safer for the surgeon? J Orthop Trauma. 1999;13:373.
78. Potter, HG, Montgomery, KD, Heise, CW, Helfet, DL. MR imaging of acetabular fractures: Value of detecting femoral head injury, intraarticular fragments, and sciatic nerve injury. AJR Am J Roentgenol. 1994;163:881.
79. National Institutes of Health. Total hip replacement. NIH Consens Statement. 1999;12:1.
80. Kosashvili, Y, Backstein, D, Safir, O, Lakstein, D, Gross, AE. Dislocation and infection after revision of total hip arthroplasty: Comparison between the first and multiply revised total hip arthroplasty. J Arthroplasty. 2011;26:1170–1175.
81. Armfield, DR, Kim, DH, Towers, JD, Bradley, JP, Robertson, DD. Sports-related muscle injury in the lower extremity. Clin Sports Med. 2006;25:803.
82. Järvinen, TA, Järvinen, TL, Kääriäinen, M, Kalimo, H, Järvinen, M. Muscle injuries: Biology and treatment. Am J Sports Med. 2005;33:745.
83. Morelli, V, Smith, V. Groin injuries in athletes. Am Fam Physician. 2001;64:1405.
84. Knoeller, SM, Uhl, M, Herget, GW. Osteitis or osteomyelitis of the pubis? A diagnostic and therapeutic challenge: Report of 9 cases and review of the literature. Acta Orthop Belg. 2006;72:541.
85. Willmann, JK, et al. Aortoiliac and lower extremity arteries assessed with 16-detector row CT angiograpy: Prospective comparison with digital subtraction angiography. Radiology. 2005;236:1083.
86. Rathjen, KE, Birch, JG. Pathologic fractures associated with tumors and unique conditions of the musculoskeletal system. In Beaty JH, Kasser JR, eds.: Rockwood and Green’s Fractures in Children, 7th ed, Philadelphia: JB Lippincott, 2010.
87. Boardman, MJ, Herman, MJ, Buck, B, Pizzutillo, PD. Hip fractures in children. J Am Acad Orthop Surg. 2009;17:162–173.
88. Arkader, A, Friedman, JE, Warner, WC, Jr., Wells, L. Complete distal femoral metaphyseal fracture: A harbinger of child abuse before walking age. J Pediatr Orthop. 2007;27:751.
89. Coffey, C, Haley, K, Hayes, J, Groner, JI. The risk of child abuse in infants and toddlers with lower extremity injuries. J Pediatr Surg. 2005;40:120.
90. Kocher, MS, Zurakowski, D, Kasser, JR. Differentiating between septic arthritis and transient synovitis of the hip in children: An evidence-based clinical prediction algorithm. J Bone Joint Surg Am. 1999;81:1662.
91. Kocher, MS, Mandiga, R, Zurakowski, D, Barnewolt, C, Kasser, JR. Validation of a clinical prediction rule for the differentiation between septic arthritis and transient synovitis of the hip in children. J Bone Joint Surg Am. 2004;86:1629.
92. Perry, DC, Bruce, C. Evaluating the child who presents with an acute limp. BMJ. 2010;341:c4250.
93. Frank, G, Mahoney, HM, Eppes, SC. Musculoskeletal infections in children. Pediatr Clin North Am. 2005;52:1083.
94. Levine, MJ, McGuire, KJ, McGowan, KL, Flynn, JM. Assessment of the test characteristics of C-reactive protein for septic arthritis in children. J Pediatr Orthop. 2003;23:373.
95. Caird, MS, et al. Factors distinguishing septic arthritis from transient synovitis of the hip in children. J Bone Joint Surg Am. 2006;88:1251.
96. Choi, IH, Yoo, WJ, Cho, TJ, Chung, CY. Operative reconstruction for septic arthritis of the hip. Orthop Clin North Am. 2006;37:173.
97. Perron, AD, Miller, MD, Brady, WJ. Orthopedic pitfalls in the emergency department: Slipped capital femoral epiphysis. Am J Emerg Med. 2002;20:484.
98. Sink, EL, Blaiser, D. Fractures and traumatic dislocations of the hip. In Beaty JH, Kasser JR, eds.: Rockwood and Green’s Fractures in Children, 7th ed, Philadelphia: JB Lippincott, 2010.
99. Ankarath, S, Ng, AB, Giannoudis, PV, Scott, BW. Delay in diagnosis of slipped upper femoral epiphysis. J R Soc Med. 2002;95:356.
100. Tins, B, Cassar-Pullicino, V, McCall, I. The role of pre-treatment MRI in established cases of slipped capital femoral epiphysis. Eur J Radiol. 2009;70:570–578.
101. McErlean, MA. The child with a limp. In: Graff J, ed. Critical Decisions in Emergency Medicine. Irving, Texas: American College of Emergency Physicians, 2004.
102. Giacomini, S, Di Gennaro, GL, Donzelli, O. Fracture of the lesser trochanter. Chir Organi Mov. 2002;87:255–258.