CHAPTER 5 Femoroacetabular Impingement: Pincer
Femoroacetabular impingement (FAI) was first reported over 70 years ago.1 However, it was not until recently was it described as a cause of hip osteoarthritis.2–4 Multiple forms of proximal femur and acetabular dysplasias have been described,5–7 but two specific mechanisms of lesion are acknowledged as being responsible for FAI, cam and pincer. Cam impingement occurs when an abnormally shaped femoral head contacts a normal acetabulum, particularly during flexion and internal rotation. Pincer impingement involves a normal femoral head contacting an abnormally shaped, deep, or retroverted acetabulum. The patterns of intra-articular soft-tissue injury resulting from the impingement appear to be unique to the distinct type of deformity.8
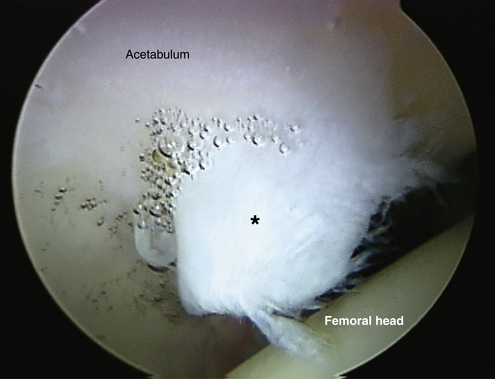
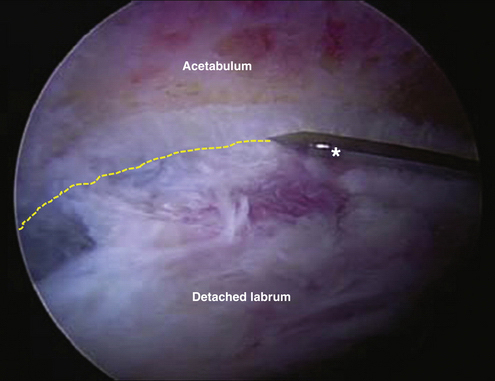
In cam impingement, the “bump” at the femoral head-neck junction produces a shearing force, displacing the labrum toward the capsule and the adjacent articular cartilage into the joint.2,8 Softening of the articular cartilage can be observed as a wave sign when arthroscopically probed before frank chondral delamination.9 With repeated insults, the labrum may completely detach from the acetabular rim, and the cartilage may fully delaminate (Fig. 5-1).
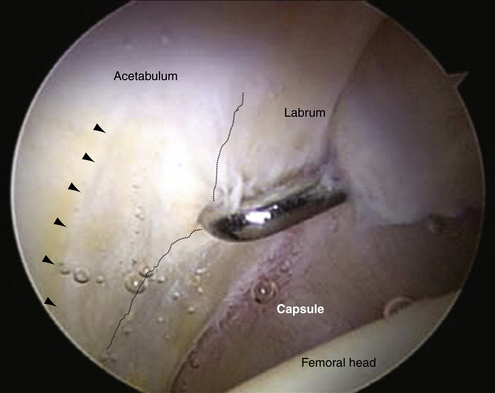
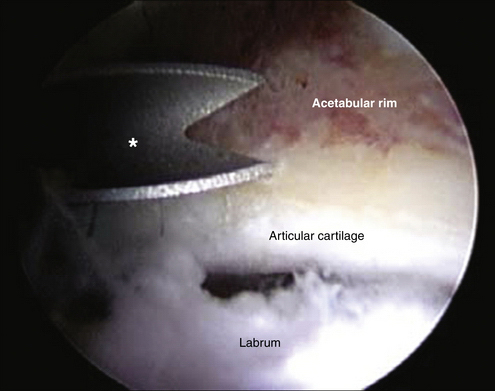
In pincer impingement, the labrum is essentially trapped between the bony structures; thus, it often bruises and flattens.2,8 With persistent pincer impingement, the labrum may degenerate, with cyst formation or ossification of the fibrocartilage. Persistent pincer impingement may lead to a chondral defect (a contrecoup lesion) at the posteroinferior acetabulum or posteromedial femoral head. The chondral injuries resulting from a pincer impingement are typically less severe than those resulting from a cam impingement (Fig. 5-2).
Demographically, cam impingement seems to be more common in young male athletes and pincer impingement in female athletes.2,10,11 Cam and pincer impingement rarely occur in isolation, and the combination has been termed mixed cam-pincer impingement. With this disorder, an abnormal femoral head or head-neck junction articulates with an abnormal acetabulum. In one epidemiologic study of 149 hips with impingement, 26 (17.4%) had isolated cam impingement, 16 (10.7%) had isolated pincer impingement, and 107 (71.8%) had combined cam-pincer impingement.8
CLINICAL PRESENTATION
Pincer impingement may be caused by general acetabular overcoverage (coxa profunda) or acetabular retroversion and has been shown to be associated with osteoarthritis of the hip.2–4,7 During flexion of the hip, the edge of the anterior wall and the anterosuperior roof of a retroverted acetabulum are vulnerable to impingement because they tend to lie directly in the path of the femoral neck.
Reynolds and colleagues7 have described the clinical presentation of acetabular retroversion. In this condition, there is not necessarily any change in the range of movement of the hip. When the retroversion is marked, however, there is a demonstrable alteration in the pattern of hip flexion in the neutral line. This may be limited to as little as 90 degrees, progressing to a full range only when allowed to move simultaneously into external rotation and abduction in a Drehman sign–like pattern.12,13 The contact of the femoral neck to the edge of the acetabulum on maximum flexion and the need to contour its retroverted mouth to continue the full range of motion explains that phenomenon.7 In these individuals, the limb tends to lie at rest in a position externally rotated at the hip. The range of external rotation, especially in the flexed position, is more generous than usual, often exceeding 60 degrees. The range of internal rotation may be limited proportionally. Asked to sit on the floor, such patients are comfortable only with their hips flexed, abducted, and externally rotated. Some describe a dislike of sitting in a chair with legs crossed, especially with the symptomatic leg crossed over the other. In some cases of coxa profunda, abduction may be limited by the lateral impingement of the femoral neck to the acetabulum.14
In the early presentation, the impingement test usually will elicit discomfort felt in the groin.7,15–17 The onset of the symptoms may be related to a new athletic activity, and females seem to be particularly susceptible. The pain is often intermittent and exacerbated by an excessive demand on hip flexion, such as occurs with athletic activities and in very flexible hips. In many cases, individuals take part in athletic activities or have occupations in which some discomfort is accepted as part of the activity. For that reason, a delayed diagnosis is not uncommon.7 Despite the recent attention directed to this condition, some patients have even had surgery in other sites because of a missed diagnosis.
The late presentation will be found in the age range of 30 to 50 years.7 Usually, the patient will remember few or no troublesome symptoms from their younger years, but direct questioning may reveal otherwise. In the impingement test, passive internal rotation induces shear forces at the labrum and will create a sharp pain when there is a labral and/or chondral lesion.2,15–18 Patients with impingement can have pain with athletic activities and even while sitting with the hip extremely flexed. Mechanical symptoms and limitations to athletic and daily activities may be present; these usually indicate intra-articular soft-tissue damage related to the impingement.11 Degenerative signs may predominate after a prolonged time without treatment.19,20
IMAGING
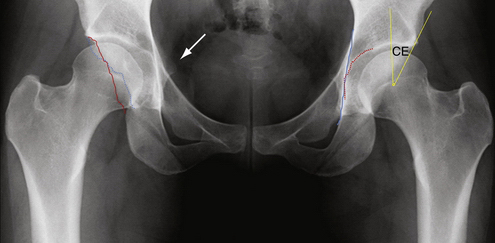
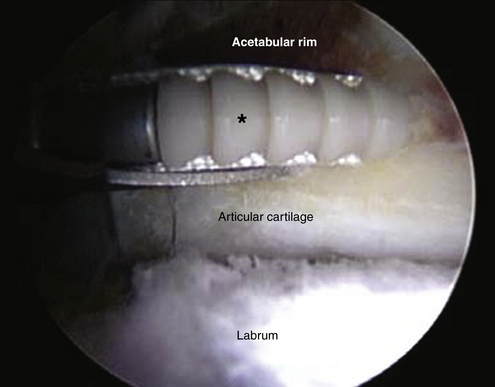
Pincer impingement is the result of overcoverage of the hip. It is commonly associated with acetabular protrusion, coxa profunda, or a retroverted acetabulum.7 Pincer impingement is also the result of a linear contact between the acetabular rim and femoral head-neck junction because of general or focal acetabular overcoverage (Fig. 5-3).7,13
Normally, general acetabular overcoverage is correlated with the radiologic depth of the acetabular fossa. A normal hip appears on an anteroposterior pelvic radiograph with the acetabular fossa line lying laterally to the ilioischial line. A coxa profunda is defined with the floor of the acetabular fossa touching or overlapping the ilioischial line medially. Protrusio acetabuli occurs when the femoral head is overlapping the ilioischial line medially. Both forms relate to an increased depth of the acetabulum; however, at this stage, no clear information exists that the two entities are a continuation of each other.13 Generally, a deep acetabulum is associated with excessive acetabular coverage that can be quantified with the lateral center edge angle or the acetabular index.20 Another parameter for quantification of femoral coverage is the femoral head extrusion index.21 An additional observation on plain radiographs may be juxta-articular fibrocystic changes (herniation pits) at the anterosuperior aspect of the femoral neck.22
The lateral center edge angle is the angle formed by a vertical line and a line connecting the femoral head center with the lateral edge of the acetabulum. A normal lateral center edge angle varies between 25 (which defines a dysplasia)20 and 39 degrees (which is an indicator for acetabular overcoverage).6
The acetabular index is the angle formed by a horizontal line and a line connecting the medial point of the sclerotic zone with the lateral center of the acetabulum. In hips with coxa profunda or protrusio acetabuli, the acetabular index (also called the acetabular roof angle) is typically 0 degree or even negative.13
The femoral head extrusion index defines the percentage of femoral head that is uncovered when a horizontal line is drawn parallel to the interteardrop line.21 A normal extrusion index is less than 25%23; however, to our knowledge, no study has defined a minimum extrusion.13
Focal acetabular overcoverage can occur in the anterior or the posterior part of the acetabulum. Anterior overcoverage is called cranial acetabular retroversion or anterior focal acetabular retroversion; it causes anterior femoroacetabular impingement that can be reproduced clinically with painful flexion and internal rotation.7 By careful tracing on an anteroposterior (AP) pelvis radiograph, the anterior and posterior acetabular rims can be identified. A normal acetabulum is anteverted and has the anterior rim line projected medially to the posterior wall line. To distinguish between a too prominent anterior wall and a deficient posterior wall, the posterior wall must be depicted in more detail. These situations can be distinguished by the crossover sign, the ischial spine sign and the posterior wall sign.13,24
A focal overcoverage of the anterosuperior acetabulum causes a cranially retroverted acetabulum. This is defined with the anterior rim line being lateral to the posterior rim in the cranial part of the acetabulum and crossing the latter in the distal part of the acetabulum. This figure-of-eight configuration is called the crossover sign.7
The posterior wall sign was introduced as an indicator for a prominent posterior wall. This can cause posterior impingement with reproducible pain in hip extension and external rotation. In a normal hip, the visible outline of the posterior rim descends approximately through the center point of the femoral head. If the posterior line lies laterally to the femoral center, a more prominent posterior wall is present. In contrast, a deficient posterior wall has the posterior rim medial to the femoral head center.7 A deficient posterior wall is often correlated with acetabular retroversion or dysplasia,23 and an excessive posterior wall can often be seen in hips with coxa profunda or protrusio acetabuli but can also occur as an isolated entity.
The ischial spine sign consists of a pre-eminent projection of that structure to the pelvis on an AP radiograph. It denotes not only global acetabular retroversion, but also the involvement of the whole hemipelvis in the deformity.24
The common use for computed tomography (CT) scans in the evaluation of impingement is to allow three-dimensional reconstruction of the hip joint for detailed definition of femoral head-neck asphericities and reduced offset, which cause osseous impingement, as well as determination of the version of the femoral neck and acetabulum.25,26 Magnetic resonance imaging (MRI) is useful to assess labral injury and the articular cartilage and to evaluate concomitant conditions.26
TECHNIQUE
Surgical Setup
Arthroscopy of the hip can be performed with the patient in a lateral or supine position.27,28 Our preference is the modified supine approach.29 We recommend a combination of general anesthesia with a lumbar plexus sciatic regional block for complete muscular paralysis.30 After the induction of anesthesia, the patient is positioned on a standard fracture table that allows independent lower extremity traction.
Portal Placement
Accurate portal placement is essential for optimal visualization of all intra-articular structures and safe access to the hip joint. We used to do three portals to perform FAI surgeries—the anterolateral, anterior, and distal lateral accessory portals.31 Currently, we think that for most cases, only the anterolateral (lateral paratrochanteric) and midanterior portals are required.10
The midanterior portal is placed approximately 7 cm distal and medial to the anterolateral portal, in a line subtending about 45 degrees with the longitudinal axis of the leg. This entry point is less likely to cause injury to the lateral cutaneous femoral nerve and provides a good angle for anchor insertion in the acetabulum and to approach the peripheral compartment. The needle is inserted aiming proximally and medially, so that it penetrates the capsule under direct visualization of the arthroscope in the center of the anterior triangle formed by the labrum, femoral head, and capsule (Fig. 5-4).10,29,30
Joint Inspection
At this point, a complete inspection of the central compartment must be performed. A group of specialists recently developed a geographic zone system to describe and record the surgical findings,32 although the clock system has been used in many studies.10,11,27,29,31,33-35 The identification of anatomic landmarks (e.g., stellate crease, transverse ligament, synovial folds) help guide the location and amount of bone resection that will be later performed.
On joint entry, a systematic examination should be performed of the entire acetabular labrum. The fibrocartilaginous labrum is normally adhered to the acetabular rim and transitions to the hyaline articular cartilage in a zone of approximately 1 to 2 mm.36 The labrum is widest anteriorly and thickest superiorly, corresponding to the weight-bearing region of the acetabulum.37 The labrum has been shown to provide approximately 5 mm of additional femoral head coverage and primarily functions as a physiologic joint seal.38 A torn labrum is thought to alter load transmission in the joint and increase articular cartilage consolidation.38 In our practice, we have observed five types of labral tears—detached, midsubstance longitudinal, flap, frayed, and degenerative. Chondral lesions may be cartilage softening, fraying, or fissuring, subchondral cysts, chondral flaps, or full-thickness abrasion with subchondral bone exposure.16
In patients with pincer lesions, the most common finding is a bruised, flattened, and degenerative labrum caused by abutment against the femoral neck.8,39 Intrasubstance labral cysts and labral ossification may occur.2 Labral ossification accounts for additional acetabular overhanging and may contribute to the impingement. In pincer lesions, a more circumferential pattern of labral and chondral damages was found compared with cam lesions. It has been reported that chondral lesions may occur from 7 to 5 o’clock in the right hip (zones 1 to 5), but most of the lesions are encountered from 12 to 2 o’clock in the right hip (zones 2 and 3).40 Nevertheless, those lesions tend to be less severe and are concentrated on the periphery of the joint (watershed zone). The area of chondral lesion often delineates the area with excessive bone overhang. Experimental studies in cadavers predicted a lack of accuracy in resection of acetabular bone by arthroscopic rim-trimming procedure of about 19 degrees,35 but those studies were performed in specimens without pincer deformity and therefore lacked this important intraoperative sign to help in the arthroscopic orientation of the bone resection.
Another typical intra-articular finding in pincer deformities is the posterior-inferior chondral lesion in the acetabulum, sometimes accompanied by a kissing lesion on the femoral head, known as a contrecoup lesion.2 The attributed cause for these injuries is a leverage of the femoral neck against the anterior margin of the acetabulum, leading to posterior dislocation of the hip mechanism, with a chondral lesion in the area under shear stress.
Capsulotomy
After thorough inspection, capsulotomy is performed about 1 cm distal to the labral margin. The extension of the capsulotomy will depend on the ability to maneuver the instruments to perform all the necessary procedures.30 The procedure usually consists of performing the capsulotomy from the correspondent area of the anterolateral portal in the capsule to the midanterior portal. Although preserving the iliofemoral ligament by avoiding excessive anterior extension of the capsulotomy anteriorly is desired, this should not impede adequate exposure and instrumentation. Therefore, further extension of the capsulotomy anteriorly and posteriorly is allowed as long as the ligament is repaired afterward.10 At all stages, the capsulotomy should be performed under direct visualization. It should be noted that the lateral retinacular vessels that provide an important source of blood supply to the femoral head lie under the lateral synovial fold, and would be at risk if blind transection were performed too laterally.33,41
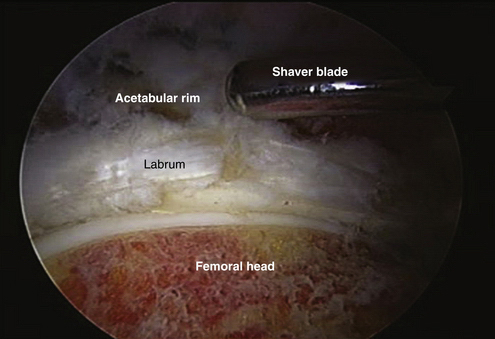
Rim Trimming with Labral Takedown
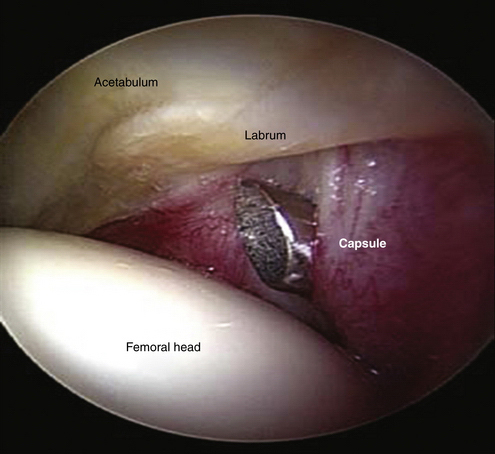
In there is labral detachment at its base, which is particularly common in cases with associated cam impingement, the labrum should be separated in the watershed zone so that the underlying bone deformity can be corrected and the labrum reattached with suture anchors.30 First, we delineate the chondrolabral junction by controlled application of a monopolar radiofrequency (RF) chisel. This will contract the fibrocartilage and better define the tear, preventing sacrifice of healthy labral tissue and stabilizing the adjacent acetabular cartilage. Any chondral flaps are removed after demarcation with the aid of the same RF device. The area between the labrum and capsule is dissected with a shaver and the labrum is completely detached from the acetabular rim as much as is needed. The acetabular bony overhang responsible for the pincer deformity can be removed with a motorized burr before or after complete labral detachment, depending on the amount of resection required (Figs. 5-5 and 5-6). The amount should be determined preoperatively by analysis of the imaging studies. There is a correlation between the center edge (CE) angle and the amount of lateral resection in millimeters. The resection should allow a postoperative CE angle of at least 25 degrees.42 The working portal to perform most of the resection is the lateral portal, although switching portals is essential for complete assessment of the resection.
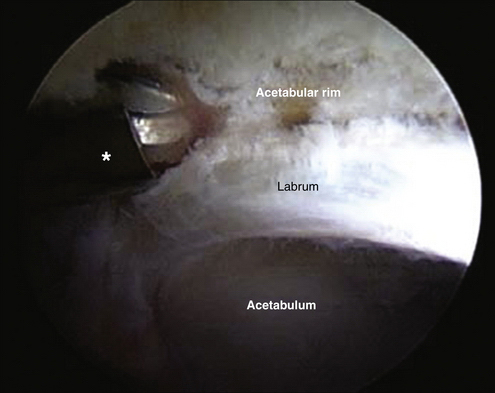
FIGURE 5-5 Acetabular rim trimming with an arthroscopic burr (*) can be performed before labral takedown.
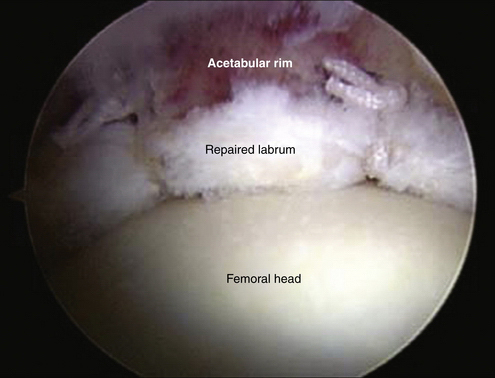
Labral Reattachment
The acetabular rim, now reshaped, is the ideal site at which to reattach the labrum. A bleeding cancellous bed has been reported as necessary for labral refixation because of the relatively avascular nature of the labrum.43 Experimental studies have demonstrated that it can heal directly to the bone, as well as to the surrounding capsule.44 The acetabular rim provides solid fixation for the anchors and a stable base to allow for labral repair. We use one bioabsorbable 2.9-mm anchor for every 1 cm of labral detachment. Smaller patients might require 2.3-mm anchors. More anchors should be placed, as needed, to provide good stability and shape to the labrum so that it can exert its physiologic functions.10,11
The anchors are placed about 2 mm off the acetabular rim in the area of the rim trimming under direct visualization of the entry point and adjacent articular surface (Fig. 5-7).30 In general, the anterolateral portal allows the insertion of anchors in the superolateral aspect of the acetabulum, where most of the lesions are found. Because the guide sleeve is directed to the trimmed acetabular margin in a divergent direction to avoid intra-articular penetration, a cranial angle of about 45 degrees is often observed in the coronal plane. The direction in the transverse plane for placement of anchors at the 12 o’clock position (zone 3) in the acetabulum is parallel to the ground. As more anterior placements are necessary, a forward inclination of the guide is performed. The limit for that is usually the position corresponding to 2 o’clock (considering the right acetabulum), where the insertion angle may be too acute. For the insertion of anterior-most anchors (beyond the 2 o’clock position, or zone 1), the midanterior portal should be used. Fluoroscopy may be used during the procedure to ensure optimal placement.
We recommend tapping the sleeve slightly into the acetabular rim and after drilling the anchor path, manually driving anchor into place using tactile sensation as a guide.30 While drilling, it is critical to visualize the articular surface of the acetabulum to ensure that it is not being compromised. If bulging of the articular surface is noted, the angle of the anchor must be redirected. Once the anchor it is in place, the articular surface should again be visualized to verify that it has not been penetrated (Fig. 5-8).
A clear 8.25-mm cannula is then introduced through the working portal and the sutures are drawn back through it. It can be also inserted before the anchor delivery device. However, in more extreme positions, it may hinder the mobility of the guide. The next step is to deliver a limb of suture between the labrum and acetabular rim with a suture passer. As the suture is pulled out through the clear cannula, it is important to visualize the anchor to ensure that the correct suture limb is being retrieved. The cannula must then be pulled back slightly for improved visualization, and the suture is tied down using standard arthroscopic knot-tying technique. In some cases, traction may be released while it is being tied to get better knot fixation (Figs. 5-8 and 5-9).
A translabral suture stitch may be done in a thick labrum (on the weight-bearing zone) to provide better apposition. In that case, one limb of the suture is delivered intra-articularly between the labrum and acetabular rim. The labrum is pierced with the suture passer in its midsubstance in an outside-in direction and a loop of the intra-articular limb of the suture is pulled through it. The suture passer is removed from the labrum and is used to pull the free end of the same suture limb completely through the loop, retrieving it through the cannula. At this point, as both limbs of the suture are tensioned simultaneously, the labrum gets closer to the acetabular rim, allowing a suture-free margin of it to be in contact with the femoral head. The suture is then tied using standard arthroscopic knot-tying technique (Fig. 5-10).
Rim Trimming Without Labral Takedown
In rare cases without labral tear and in which a minimum amount of acetabular bone resection is required, the rim trimming can be performed without labral takedown.10,45 Most of those cases are accompanied by cam deformities and we use the following surgical strategy.
To obtain adequate space to work between the capsule and labrum, we release traction, extend the capsulotomy, and treat the peripheral compartment first. We use a shaver to dissect the space between the capsule and labrum, exposing the underlying bone. The resection is then performed as planned. Traction is introduced again and the labrum is inspected. Unless a very modest resection was performed (1 mm), the chondrolabral junction usually is torn or so thin that an additional attachment to the acetabular rim is necessary. It is our impression that the junction is not able to handle the physiologic stresses when the supportive bone to the labrum has been removed. Failure in the watershed zone is to be expected when it is the only attachment of the labrum. In fact, the senior author (MJP) has revised one case in which that procedure was performed without additional fixation of the labrum to the bone; the intraoperative findings were labral tear at the transition (watershed) zone and adherence of the labrum to the adjacent capsule, despite no history of new trauma. Therefore, we currently perform and recommend anchor placement and suture fixation of the labrum to the acetabulum in those situations, despite not taking down the labrum. Additional studies are required to establish whether this precaution should be taken. However, we think that this practice at least allows a more active rehabilitation process, which we believe is very important to prevent adherences and allow early return to most activities.46
The technique for anchor placement without labral detachment does not differ much from that described for the other. It may be slightly more difficult to inspect the entry point and articular surface constantly during anchor insertion. The suture fixation follows the same technique, except that the chondrolabral junction must be pierced to pass one of the suture limbs between the labrum and acetabulum.
Other Lesions and Completing the Procedure
Peripheral chondral lesions, usually related to pincer lesion, often disappear after the resection of the underlying pathologic bone. The remaining chondral edge then needs to be stabilized; a flexible RF probe may be used for that purpose and to contour the edges of the labrum. However, more extensive chondral damage may be present, mainly when other conditions are associated or the treatment was performed long after the onset of symptoms. In those cases, local débridement, thermal chondroplasty, or microfractures may be performed, depending on the lesion type.10,47
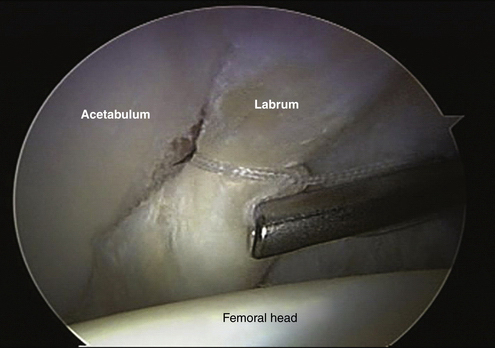
It is important to note that isolated pincer lesions occur in only 10.7% of the cases.8 Femoral deformities usually coexist and should be addressed to prevent failure of the treatment.48 After all lesions are treated, dynamic inspection of the joint, without traction must be done arthroscopically to disclose any possible conflict between the labrum and femoral neck. Any signs of impingement should elicit further bone reshaping or labral contouring. The need for more anchors is commonly noted at this time.10 We always test all the possible movements related to patient activities to obtain maximum range of motion without impingement (Fig. 5-11). Dynamic fluoroscopy may aid in determining the adequacy of bone resection, but is not a substitute for direct arthroscopic inspection. Following dynamic visualization, we close the capsule, which we believe to be important to resume rehabilitation and prevent instability.49
PEARLS& PITFALLS
LABRAL REATTACHMENT
Pearls
REHABILITATION
Rehabilitation following arthroscopic femoroacetabular impingement treatment includes restrictions of weight bearing, rotation, and movement. Patients are kept at 20 lb of weight bearing with 8 to 12 hours daily of continuous passive movement (CPM) for 4 weeks. An antirotation bolster to prevent external hip rotation of the hip is used for 10 days after surgery.10,30,46,49 Microfracture treatment of chondral lesions involves 6 to 8 weeks of partial weight bearing and continued CPM.47 Physiotherapy is used first to restore passive motion, followed by active motion and then strengthening exercises. Internal rotation is gained first, and then external rotation. We also recommend passive hip pendulums or circumduction movements to prevent adhesion formation.
SUMMARY
In conclusion, this approach to treat pincer lesions resembles those previously described to trim the acetabular rim and repair the labrum, with some modifications.31 Our current approach has resulted from experience treating over 2000 patients with FAI arthroscopically, and it has shown to be efficient and reproducible.10
1. Smith-Petersen MN. Treatment of malum coxae senilis, old slipped upper femoral epiphysis, intrapelvic protrusion of the acetabulum, and coxa plana by means of acetabuloplasty. J Bone Joint Surg. 1936;18:869-880.
2. Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112-120.
3. Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264-272.
4. Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:263-269.
5. Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin: Springer; 1987.
6. Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747-1770.
7. Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281-288.
8. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012-1018.
9. Johnston TL, Schenker ML, Briggs KK, Philippon MJ. Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy. 2008;24:669-675.
10. Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91:16-23.
11. Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clin Sports Med. 2006;25:299-308.
12. Drehmann F. Drehmann’s sign: a clinical examination method in epiphysiolysis (slipping of the upper femoral epiphysis)—description of signs, aetiopathogenetic considerations, clinical experience [in German]. Z Orthop Ihre Grenzgeb. 1979;117:333-344.
13. Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540-1552.
14. Shindle MK, Voos JE, Nho SJ, et al. Arthroscopic management of labral tears in the hip. J Bone Joint Surg Am. 2008;90:2-19.
15. Philippon MJ, Maxwell RB, Johnston TL, et al. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1041-1047.
16. Philippon MJ, Souza BGS. Identifying labral tears in daily practice. Sports Med Update. 2009;2:3-6.
17. Burnett RS, Della Rocca GJ, Prather H, et al. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88:1448-1457.
18. McCarthy JC, Noble PC, Schuck MR, et al. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001;393:25-37.
19. Maheshwari AV, Malik A, Dorr LD. Impingement of the native hip joint. J Bone Joint Surg Am. 2007;89:2508-2518.
20. Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. J Bone Joint Surg Am. 1995;77:985-989.
21. Heyman CH, Herndon CH. Legg-Perthes disease: a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950;32:767-778.
22. Leunig M, Beck M, Kalhor M, et al. Fibrocystic changes at anterosuperior femoral neck: prevalence in hips with femoroacetabular impingement. Radiology. 2005;236:237-246.
23. Li PLS, Ganz R. Morphologic features of congenital acetabular dysplasia. Clin Orthop Relat Res. 2003;416:245-253.
24. Kalberer F, Sierra RJ, Madan SS, et al. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466:677-683.
25. Yamamoto Y, Tonotsuka H, Ueda T, Hamada Y. Usefulness of radial contrast-enhanced computed tomography for the diagnosis of acetabular labrum injury. Arthroscopy. 2007;232:1290-1294.
26. Fadul DA, Carrino JA. Imaging of femoroacetabular impingement. J Bone Joint Surg Am. 2009;91:138-143.
27. Byrd JW. Hip arthroscopy in the supine position. Oper Tech Sports Med. 2002;10:184-195.
28. Glick JM, Sampson TG, Gordon RB, et al. Hip arthroscopy by the lateral approach. Arthroscopy. 1987;3:4-12.
29. Kelly BT, Williams RJ3rd, Philippon MJ. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med. 2003;31:1020-1037.
30. Philippon MJ, Stubbs AJ, Schenker ML, et al. Arthroscopic management of femoroacetabular impingement: osteoplasty technique and literature review. Am J Sports Med. 2007;35:1571-1580.
31. Philippon MJ, Schenker ML. A new method for acetabular rim trimming and labral repair. Clin Sports Med. 2006;25:293-297.
32. Ilizaliturri VMJr, Byrd JW, Sampson TG, et al. A geographic zone method to describe intra-articular pathology in hip arthroscopy: cadaveric study and preliminary report. Arthroscopy. 2008;24:534-539.
33. Dvorak M, Duncan CP, Day B. Arthroscopic anatomy of the hip. Arthroscopy. 1990;6:264-273.
34. Kelly BT, Weiland DE, Schenker M, et al. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21:1496-1504.
35. Zumstein M, Hahn F, Sukthankar A, et al. How accurately can the acetabular rim be trimmed in hip arthroscopy. for pincer-type femoral acetabular impingement: a cadaveric investigation. Arthroscopy. 2009;25:164-168.
36. Seldes RM, Tan V, Hunt J, et al. Anatomy, histologic features and vascularity of the adult acetabular labrum. Clin Orthop Relat Res. 2001;382:232-240.
37. Tan V, Seldes RM, Katz MA, et al. Contribution of acetabular labrum to articulating surface area and femoral head coverage in adult hip joints: an anatomic study in cadavera. Am J Orthop. 2001;30:809-812.
38. Ferguson SJ, Bryant JT, Ganz R, et al. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36:171-178.
39. Lavigne M, Parvizi J, Beck M, et al. Anterior femoroacetabular impingement Part 1: techniques of joint-preserving surgery. Clin Orthop Relat Res. 2004;418:61-66.
40. Tannast M, Goricki D, Beck M, et al. Hip damage occurs at the zone of femoroacetabular impingement. Clin Orthop Relat Res. 2008;466:273-280.
41. Ilizaturri VMJr. Complications of arthroscopic femoroacetabular impingement treatment: a review. Clin Orthop Relat Res. 2009;467:760-768.
42. Philippon MJ, Wolff AB, Briggs KK, et al. Rim reduction for the treatment of pincer-type FAI correlates with pre- and postoperative CE angle, Paper presented at: 2009. Annual Meeting of the American Academy of Orthopaedic Surgeons; February 2009, Las Vegas: American Academy of Orthopaedic Surgeons; 2009.
43. Espinosa N, Rothenfluh DA, Beck M, et al. Treatment of femoroacetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925-935.
44. Philippon MJ, Arnoczky SP, Torrie A. Arthroscopic repair of the acetabular labrum: a histologic assessment of healing in an ovine model. Arthroscopy. 2007;23:376-380.
45. Sampson TG. Arthroscopic treatment of femoroacetabular impingement. Am J Orthop. 2008;37:608-612.
46. Philippon MJ, Christensen JC, Wahoff MS. Rehabilitation after arthroscopic repair of intra-articular disorders of the hip in a professional football athlete. J Sport Rehabil. 2009;18:118-134.
47. Philippon MJ, Schenker ML, Briggs KK, Maxwell RB. Can microfracture produce repair tissue in acetabular chondral defects? Arthroscopy. 2008;24:46-50.
48. Wenger DE, Kendell KR, Miner MR, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;426:145-150.
49. Ranawat AS, McClincy M, Sekiya JK. Anterior dislocation of the hip after arthroscopy in a patient with capsular laxity of the hip: a case report. J Bone Joint Surg Am. 2009;91:192-197.
50. Enseki KR, Martin RL, Draovitch P, et al. The hip joint: arthroscopic procedures and postoperative rehabilitation. J Orthop Sports Phys Ther. 2006;36:516-525.