CHAPTER 26 Femoral nerve block
Clinical anatomy
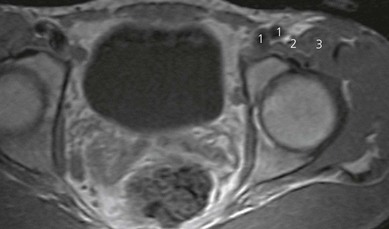
The femoral nerve arises from the ventral rami of the second, third, and fourth lumbar nerves. It descends through the substance of the psoas major, emerging from the muscle at the lower part of its lateral border, and passes down between it and the iliacus muscle, deep to the fascia iliaca (Fig. 26.1). It then passes behind the inguinal ligament to enter the thigh. The nerve lies deep to the fascia lata and fascia iliaca. The fascia iliacus separates it from the vascular bundle containing the femoral artery and vein (Fig. 26.2). It divides into two major branches (anterior and posterior) early in the proximal anterior thigh (Fig. 26.1).
Surface anatomy
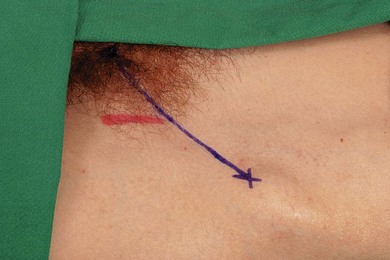
The main landmarks for femoral nerve block are the anterior superior iliac spine, the pubic tubercle, inguinal ligament, inguinal crease, and femoral artery (Fig. 26.3). The pubic tubercle can be palpated three fingers’ breadth from the midline, along the upper border of the pubis. The inguinal ligament is outlined by a line connecting the anterior superior iliac spine and the pubic tubercle.
Sonoanatomy
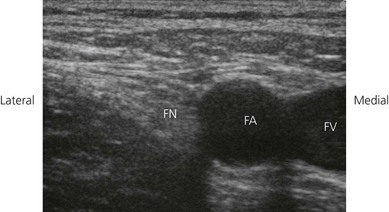
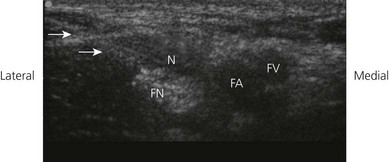
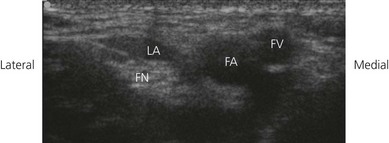
The femoral nerve is found lateral to the femoral artery in the groin, lying outside the femoral sheath and beneath the fascia lata and iliaca. These fascial layers are seen as hyperechoic lines. Its appearance on ultrasound (Fig. 26.4) is similar to many peripheral nerves, and described as multiple round or oval hypoechoic (dark) areas encircled by hyperechoic (bright) rims. The hypoechoic structures are the nerve fascicles. The femoral nerve may be identified on ultrasound as an oval (95% oval beneath the inguinal ligament) or triangular-shaped structure measuring approximately 3 mm in anteroposterior diameter and 10 mm in mediolateral diameter. Correct transducer angulation is essential for adequate nerve visualization. Femoral nerve anisotropy occurs with transducer angulation of as little as 10° from the vertical. Anisotropy is a property of muscles, nerves, and tendons which relates to the change in ultrasound appearance of the target structure with the scanning angle used. Nerves are best visualized when the ultrasound beam hits them at 90°. In this case, the femoral nerve becomes isoechoic with surrounding structures, and disappears from view, when the transducer is angled 10–13° from the vertical.
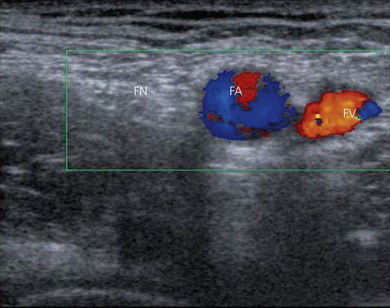
To identify the femoral nerve, the transducer is placed over the femoral vessels on the anterior thigh at 90° to the expected orientation of the nerve and vessels (Fig. 26.5). The vessels may be identified as large round hypoechoic structures, and blood flow may be demonstrated using colorflow Doppler (Fig. 26.6). The femoral nerve is then visualized a variable distance lateral to the femoral artery.
Technique
Landmark-based approach
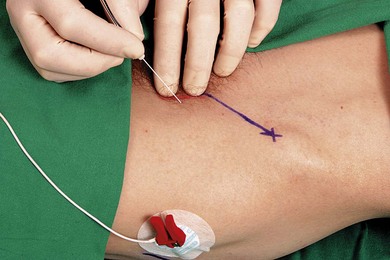
The patient is placed in the supine position with the operator standing on the side to be blocked, at the level of the patient’s thigh. The needle insertion point is infiltrated with local anesthetic using a 25-G needle. A 50-mm 21-G insulated needle is oriented in a 45° cephalad and posterior orientation lateral to the palpated femoral artery at the inguinal crease (Fig. 26.7). The stimulating current is set at 1.0 mA, 2 Hz, and 0.1 ms.
Incremental injections of local anesthetic are made with repeated aspiration. Fifteen milliliters of local anesthetic will adequately block the femoral nerve, but if a three-in-one block is required then use 30 mL in an adult (Figs 26.8 and 26.9). If a quadriceps contraction is not elicited, the needle is aimed 10° laterally. Contraction of the sartorius muscle is not appropriate; the needle should be oriented 10° laterally from this point and inserted slightly deeper. Multi-injection techniques have been described.

Figure 26.9 Sagittal T1-weighted MR image of spread after injection of 30 mL of contrast. Note similarity of spread in Figure 26.8. Note that contrast covers the femoral nerve and spreads laterally toward the anterior superior iliac spine, where the lateral cutaneous nerve of the thigh lies. The contrast did not reach the roots of the lumbar plexus. 1: Anterior superior iliac spine; 2: psoas muscle; 3: iliacus muscle; 4: contrast spread; 5: injection site.
Ultrasound-guided approach
The operator stands or sits on the side to be blocked, and with the patient in a supine position (Fig. 26.10). The skin is disinfected with antiseptic solution and draped. A sterile sheath (CIVCO Medical Instruments, Kalona, IA, USA) is applied over the ultrasound transducer with sterile ultrasound gel (Aquasonic, Parker Laboratories, Fairfield, NJ, USA). Another layer of sterile gel is placed between the sterile sheath and the skin. The infrainguinal region is scanned with a 6–13 MHz linear transducer. The ultrasound screen should be made to look like the scanning field. That is, the right side of the screen represents the right side of the field. Adjustable ultrasound variables such as scanning mode, depth of field, and gain are optimized.
A transverse image of the femoral nerve, artery, and vein is obtained (Fig. 26.4). The femoral nerve is kept in the centre of the field of view. The needle entry site is at the lateral-most end of the linear transducer. A 23-gauge needle is advanced under real-time ultrasound guidance and local anesthetic is deposited along the needle entry path. A free hand technique rather than the use of a needle guide is preferred. A 21-GA × 50-mm insulated needle (B. Braun, Bethlehem PA) is inserted parallel to the axis of the beam of the ultrasound transducer, with the bevel facing the transducer (Fig. 26.11). The needle is attached to sterile extension tubing, which is connected to a 20 mL syringe and flushed with local anesthetic solution to remove all air from the system. It is then introduced at the lateral-most end of the transducer and visualized along its entire path to the femoral nerve (Fig. 26.12). It is important not to advance the needle without good visualization. This may require needle or ultrasound transducer adjustment.
Once the needle has approached the femoral nerve, 1–2 mL of local anesthetic may be injected to confirm correct needle placement. Local anesthetic appears as a hypoechoic image. Correct needle placement is confirmed by observing solution surrounding the femoral nerve (Fig. 26.13). Should this not occur, the needle may need to be repositioned, and the procedure repeated. Following confirmation of correct needle placement, 10–20 mL of local anesthetic solution can be injected to achieve blockade.
Saphenous nerve block landmark-based approach
The saphenous nerve passes within the adductor canal beneath the sartorius muscle, and then curves around the posteriomedial aspect of the knee to divide into branches along the anteriomedial aspect of the proximal tibia (Fig. 26.14).
Saphenous nerve block ultrasound-guided approach
The operator stands on the side to be blocked, with the patient in a supine position, the knee flexed to 45° and the hip externally rotated (Fig. 26.15). The skin is disinfected with antiseptic solution and draped. A sterile sheath (CIVCO Medical Instruments, Kalona, IA, USA) is applied over the ultrasound transducer with sterile ultrasound gel (Aquasonic, Parker Laboratories, Fairfield, NJ, USA). Another layer of sterile gel is placed between the sterile sheath and the skin. The infrainguinal region is scanned with a 6–13 MHz linear transducer. The ultrasound screen should be made to look like the scanning field. That is, the right side of the screen represents the right side of the field. Adjustable ultrasound variables such as scanning mode, depth of field, and gain are optimized.
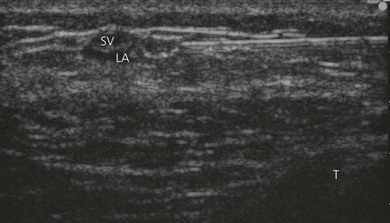
A transverse image of the great saphenous vein is obtained (Fig. 26.16). A thigh tourniquet can facilitate this. The saphenous vein is kept in the centre of the field of view. The saphenous nerve lies in its proximity. The needle entry site is at the lateral-most end of the linear transducer. A 23-gauge needle is advanced under real-time ultrasound guidance and local anesthetic is deposited along the needle entry path. A free hand technique rather than the use of a needle guide is preferred. A 21-GA × 50-mm insulated needle (B. Braun, Bethlehem PA) is inserted parallel to the axis of the beam of the ultrasound transducer (Fig. 26.17). The needle is attached to sterile extension tubing, which is connected to a 10 mL syringe and flushed with local anesthetic solution to remove all air from the system. It is then introduced at the lateral-most end of the transducer and visualized along its entire path to the saphenous nerve. It is important not to advance the needle without good visualization. This may require needle or ultrasound transducer adjustment.
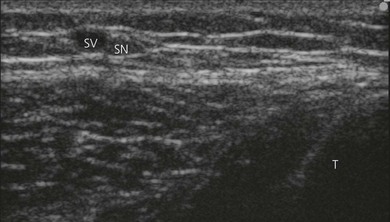
Figure 26.16 Ultrasound identification of saphenous nerve and vein. SN : saphenous nerve; SV : saphenous vein; T: tibia.
Once the needle has approached the saphenous nerve, 1–2 mL of local anesthetic may be injected. Local anesthetic appears as a hypoechoic image. Correct needle placement is confirmed by observing solution surrounding the saphenous nerve (Fig. 26.18). Should this not occur, the needle may need to be repositioned, and the procedure repeated. Following confirmation of correct needle placement, 5–10 mL of local anesthetic solution can be injected to achieve blockade. A trans-sartorial peri-femoral technique has also been described.
Adverse effects
Clinical pearls
Casati A, Fanelli G, Beccaria P, et al. The effects of the single or multiple injection technique on the onset time of femoral nerve blocks with 0.75% ropivacaine. Anesth Analg. 2000;91:181-184.
Fredrickson MJ, Ball CM, Dalgleish AJ, et al. A prospective randomized comparison of ultrasound and neurostimulation as needle end points for interscalene catheter placement. Anesth Analg. 2009;108(5):1695-1700.
Gray AT, Collins AB. Ultrasound-guided saphenous nerve block. Reg Anesth Pain Med. 2003;28(2):148.
Gray AT, Collins AB, Schafhalter-Zoppoth I. An introduction to femoral nerve and associated lumbar plexus nerve blocks under ultrasonic guidance. Techniques in Regional Anesthesia and Pain Management. 2004;8:155-163.
Gruber H, Peer S, Kovacs P, et al. The ultrasonographic appearance of the femoral nerve and cases of iatrogenic impairment. J Ultrasound Med. 2003;22(2):163-172.
Marhofer P, Nasel C, Sitzwohl C, et al. Magnetic resonance imaging of the distribution of local anesthetic during the three-in-one block. Anesth Analg. 2000;90:119-124.
Tsui BC, Ozelsel T. Ultrasound-guided transsartorial perifemoral artery approach for saphenous nerve block. Reg Anesth Pain Med. 2009;34(2):177-178.
Vloka JD, Hadzic A, Drobnik L, et al. Anatomical landmarks for femoral nerve block: a comparison of four needle insertion sites. Anesth Analg. 1999;89:1467-1470.
Winnie AP, Ramamurthy S, Durrani Z. The inguinal paravascular technique of lumbar plexus anesthesia: the ‘3-in-1 block’. Anesth Analg. 1973;52:989-996.